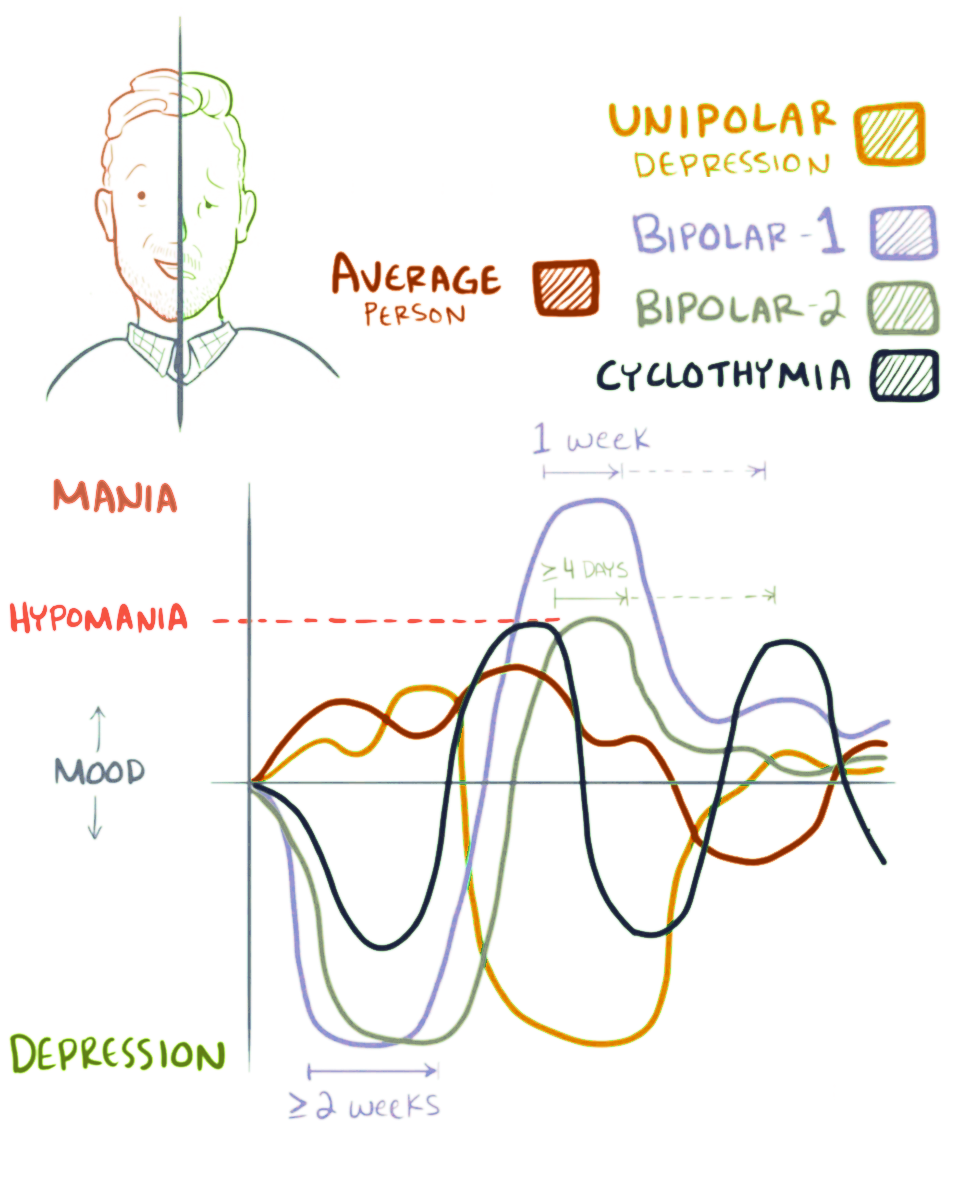
Bipolar II disorder is a bipolar spectrum disorder (see also: Bipolar I disorder) characterized by at least one episode of hypomania and at least one episode of major depression. Diagnosis for bipolar II disorder requires that the individual must never have experienced a full manic episode. Otherwise, one manic episode meets the criteria for bipolar I disorder.
Hypomania is a sustained state of elevated or irritable mood that is less severe than mania yet may still significantly affect quality of life and result in permanent consequences including neuroprogression, chronic inflammation and permanent socioeconomic ramifications from reckless spending, damaged relationships and poor judgment. Unlike mania, hypomania is not associated with psychosis. The hypomanic episodes associated with bipolar II disorder must last for at least four days. Commonly, depressive episodes are more frequent and more intense than hypomanic episodes. Additionally, when compared to bipolar I disorder, type II presents more frequent depressive episodes and shorter intervals of well-being. The course of bipolar II disorder is more chronic and consists of more frequent cycling than the course of bipolar I disorder. Finally, bipolar II is associated with a greater risk of suicidal thoughts and behaviors than bipolar I or unipolar depression. Although bipolar II is commonly perceived to be a milder form of Type I, this is not the case. Types I and II present equally severe burdens.
Bipolar II is notoriously difficult to diagnose. Patients usually seek help when they are in a depressed state, or when their hypomanic symptoms manifest themselves in unwanted effects, such as high levels of anxiety, or the seeming inability to focus on tasks. Because many of the symptoms of hypomania are often mistaken for high functioning behavior or simply attributed to personality, patients are typically not aware of their hypomanic symptoms. In addition, many people who suffer from Bipolar II have periods of normal affect. As a result, when patients seek help, they are very often unable to provide their doctor with all the information needed for an accurate assessment; these individuals are often misdiagnosed with unipolar depression. Of all individuals initially diagnosed with major depressive disorder, between 40% and 50% will later be diagnosed with either BP-I or BP-II. Substance abuse disorders (which have high co-morbidity with BP-II) and periods of mixed depression may also make it more difficult to accurately identify BP-II. Despite the difficulties, it is important that BP-II individuals be correctly assessed so that they can receive the proper treatment. Antidepressant use, in the absence of mood stabilizers, is correlated with worsening BP-II symptoms.
Signs and symptoms
Hypomanic episodes
Hypomania is the signature characteristic of Bipolar II disorder. It is a state characterized by euphoria and/or an irritable mood. In order for an episode to qualify as hypomanic, the individual must also present three or more of the below symptoms, and last at least four consecutive days and be present most of the day, nearly every day
- Inflated self-esteem or grandiosity.
- Decreased need for sleep (e.g., feels rested after only 3 hours of sleep).
- More talkative than usual or pressure to keep talking.
- Flight of ideas or subjective experience that thoughts are racing.
- Distractibility (i.e., attention too easily drawn to unimportant or irrelevant external stimuli), as reported or observed.
- Increase in goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation.
- Excessive involvement in activities that have a high potential for painful consequences (e.g., engaging in unrestrained buying sprees, sexual indiscretions, or foolish business investments).
It is important to distinguish between hypomania and mania. Mania is generally greater in severity and impairs function, sometimes leading to hospitalization and in the most severe cases, psychosis. In contrast, hypomania usually increases functioning. For this reason, it is not uncommon for hypomania to go unnoticed. Often it is not until individuals are in a depressive episode that they seek treatment, and even then their history of hypomania may go undiagnosed. Even though hypomania may increase functioning, episodes need to be treated because they may precipitate a depressive episode.
Depressive episodes
It is during depressive episodes that BP-II patients often seek help. Symptoms may be syndromal or subsyndromal. Depressive BP-II symptoms may include five or more of the below symptoms (at least one of them must be either depressed mood or loss of interest/pleasure). In order to be diagnosed, they need to be present only during the same two-week period, as a change from previous hypomanic functioning:
- Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, or hopeless) or observation made by others (e.g., appears tearful). (Note: In children and adolescents, can be irritable mood.)
- Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation).
- Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day. (Note: In children, consider failure to make expected weight gain.)
- Insomnia or hypersomnia nearly every day.
- Psychomotor agitation or retardation nearly every day (observable by others; not merely subjective feelings of restlessness or being slowed down).
- Fatigue or loss of energy nearly every day.
- Feelings of worthlessness or excessive or inappropriate guilt nearly every day (not merely self-reproach or guilt about being sick).
- Diminished ability to think or concentrate, possible irritability or indecisiveness, nearly every day (either by subjective account or as observed by others).
- Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, a suicide attempt, or a specific plan for completing suicide.
Evidence also suggests that BP-II is strongly associated with atypical depression. Essentially, this means that many BP-II patients exhibit reverse vegetative symptoms. BP-II patients may have a tendency to oversleep and overeat, while typically depressed patients sleep and eat less than usual.
Mixed depression
Depressive mixed states occur when patients experience depression and non-euphoric, usually subsyndromal, hypomania at the same time. As mentioned previously, it is particularly difficult to diagnose BP-II when a patient is in this state.
In a mixed state, mood is depressed, but the following symptoms of hypomania present as well:
- Irritability
- Mental overactivity
- Behavioral overactivity
Mixed states are associated with greater levels of suicidality than non-mixed depression. Antidepressants may increase this risk.
Relapse
In the case of a relapse, the following symptoms often occur and are considered early warning signs:
- Sleep disturbance: patient requires less sleep and does not feel tired
- Racing thoughts and/or speech
- Anxiety
- Irritability
- Emotional intensity
- Spending more money than usual
- Binge behavior, including food, drugs, or alcohol
- Arguments with family members and friends
- Taking on many projects at once
People with bipolar disorder may develop dissociation to match each mood they experience. For some, this is done intentionally, as a means by which to escape trauma or pain from a depressive period, or simply to better organize one's life by setting boundaries for one's perceptions and behaviors.
Studies indicate that the following events may also precipitate relapse in BP-II patients:
- Stressful life events
- Relatives' or peers' criticism
- Antidepressant use
- Disrupted circadian rhythm
Comorbid conditions
Comorbid conditions are extremely common in individuals with BP-II. In fact, individuals are twice as likely to present a comorbid disorder than not. These include anxiety, eating, personality (cluster B), and substance use disorders. For bipolar II disorder, the most conservative estimate of lifetime prevalence of alcohol or other drug abuse disorders is 20%. In patients with comorbid substance abuse disorder and BP-II, episodes have a longer duration and treatment compliance decreases. Preliminary studies suggest that comorbid substance abuse is also linked to increased risk of suicidality. The question of which condition should be designated the index and which the comorbid condition is not self-evident and may vary in relation to the research question, the disease that prompted a particular episode of care, or of the specialty of the attending physician. A related notion is that of complication, a condition that coexists or ensues, as defined in the Medical Subject Headings (MeSH)-controlled vocabulary maintained by the National Library of Medicine (NLM).
Causes
Scientists are studying the possible causes of bipolar disorder and most agree that there is no single cause. There have been very few studies conducted to examine the possible causes of Bipolar II. Those that have been done have not considered Bipolar I and Bipolar II separately and have had inconclusive results. Researchers have found that patients with either Bipolar I or II may have increased levels of blood calcium concentrations, but the results are inconclusive. The studies that have been conducted did not find a significant difference between those with Bipolar I or Bipolar II. There has been a study looking at genetics of Bipolar II disorder and the results are inconclusive; however, scientists did find that relatives of people with Bipolar II are more likely to develop the same bipolar disorder or major depression rather than developing Bipolar I disorder. The cause of Bipolar disorder can be attributed to misfiring neurotransmitters that overstimulate the amygdala, which in turn causes the prefrontal cortex to stop working properly. The bipolar patient becomes overwhelmed with emotional stimulation with no way of understanding it, which can trigger mania and exacerbate the effects of depression.
Diagnosis
The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) recognizes two types of bipolar disorders—bipolar I and bipolar II. People with bipolar I disorder suffer from at least one manic or mixed episode, and may experience depressive episodes. On the contrary, as noted above, people with bipolar II disorder experience a milder form of a manic episode, known as a hypomanic episode as well as major depressive episodes. Although bipolar II is thought to be less severe than bipolar I in regards to symptom intensity, it is actually more severe and distressing with respect to episode frequency and overall course. Those with bipolar II often experience more frequent bouts of depressive episodes. Specific criteria defined by the DSM-V for a bipolar II diagnosis is as follows:
- Criteria have been met for at least one hypomanic episode and at least one major depressive episode.
- There has never been a manic episode.
- The occurrence of the hypomanic episode(s) and major depressive episode(s) is not better explained by schizoaffective disorder, schizophrenia, delusional disorder, or other specified or unspecified schizophrenia spectrum and other psychotic disorder.
- Causes significant stress or impairment in social, occupational, or other important areas of functioning.
Studies have identified major differences between bipolar I and bipolar II in regards to their clinical features, comorbidity rates and family histories. According to Baek et al. (2011), during depressive episodes, bipolar II patients tend to show higher rates of psychomotor agitation, guilt, shame, suicidal ideation, and suicide attempts. Bipolar II patients have shown higher lifetime comorbidity rates of DSM axis I diagnoses such as phobias, anxiety disorders, substance & alcohol abuse, and eating disorders and there is a higher correlation between bipolar II patients and family history of psychiatric illness, including major depression and substance-related disorders. The occurrence rate of psychiatric illness in first degree relatives of bipolar II patients was 26.5%, versus 15.4% in bipolar I patients.
Screening instruments like the Mood Disorders Questionnaire (MDQ) are helpful tools in determining a patient's status on the bipolar spectrum, and getting families involved can also improve chances of an accurate diagnosis and acknowledgment of hypomanic episodes. In addition, there are certain features that have been shown to increase the chances that depressed patients are suffering from a bipolar disorder including atypical symptoms of depression like hypersomnia and hyperphagia, a family history of bipolar disorder, medication-induced hypomania, recurrent or psychotic depression, antidepressant refractory depression, and early or postpartum depression.
Specifiers
- Chronic
- With Anxious Distress (DSM-5)
- With catatonic features
- With melancholic features
- With psychotic features
- With atypical features
- With postpartum onset
- Longitudinal course specifiers (with and without inter-episode recovery)
- With seasonal pattern (applies only to the pattern of major depressive episodes)
- With rapid cycling
Treatments
Treatment typically includes three things: the treatment of acute hypomania, the treatment of acute depression, and the prevention of the relapse of either hypomania or depression. The main goal is to make sure that patients do not harm themselves.
Medications
The most common treatment for reducing bipolar II disorder symptoms is medication, usually in the form of mood stabilizers. However, treatment with mood stabilizers may produce a flat affect in the patient, which is dose-dependent. Concurrent use of SSRI antidepressants may help some with bipolar II disorder, though these medications should be used with caution because it is believed that they may cause a hypomanic switch.
The pharmaceutical management of bipolar II disorder is not generally supported by strong evidence, with limited randomised controlled trials (RCTs) published in the literature. Some medications used are:
- Lithium - There is strong evidence that lithium is effective in treating both the depressive and hypomanic symptoms in bipolar II. In addition, its action as a mood stabilizer can be used to decrease the risk of hypomanic switch in patients treated with antidepressants.
- Anticonvulsants - there is evidence that lamotrigine decreases the risk of relapse in rapid cycling bipolar II. It appears to be more effective in bipolar II than bipolar I, suggesting that lamotrigine is more effective for the treatment of depressive rather than manic episodes. Doses ranging from 100–200 mg have been reported to have the most efficacy, while experimental doses of 400 mg have rendered little response. A large, multicentre trial comparing carbamazepine and lithium over two and a half years found that carbamazepine was superior in terms of preventing future episodes of bipolar II, although lithium was superior in individuals with bipolar I. There is also some evidence for the use of valproate and topiramate, although the results for the use of gabapentin have been disappointing.
- Antidepressants - there is evidence to support the use of SSRI and SNRI antidepressants in bipolar II. Indeed, some sources consider them to be one of the first line treatments. However, antidepressants also pose significant risks, including a switch to mania, rapid cycling, and dysphoria, so many psychiatrists advise against their use for bipolar. When used, antidepressants are typically combined with a mood stabilizer.
- Antipsychotics - there is good evidence for the use of quetiapine, and it has been approved by the FDA for this indication. There is also some evidence for the use of risperidone, although the relevant trial was not placebo controlled and was complicated by the use of other medications in some of the patients.
- Dopamine agonists - there is evidence for the efficacy of pramipexole from one randomized control trial.
Non-pharmaceutical therapies
Non-pharmaceutical therapies can also help those with the illness. These include cognitive behavioral therapy (CBT), psychodynamic therapy, psychoanalysis, social rhythm therapy, interpersonal therapy, behavioral therapy, cognitive therapy, art therapy, music therapy, psychoeducation, mindfulness, light therapy, and family-focused therapy. Relapse can still occur, even with continued medication and therapy.
Prognosis
There is evidence to suggest that bipolar II has a more chronic course of illness than bipolar I disorder. This constant and pervasive course of the illness leads to an increased risk in suicide and more hypomanic and major depressive episodes with shorter periods between episodes than bipolar I patients experience. The natural course of bipolar II disorder, when left untreated, leads to patients spending the majority of their lives unwell with much of their suffering stemming from depression. Their recurrent depression results in personal suffering and disability.
This disability can present itself in the form of psychosocial impairment, which has been suggested to be worse in bipolar II patients than in bipolar I patients. Another facet of this illness that is associated with a poorer prognosis is rapid cycling, which denotes the occurrence of four or more major Depressive, Hypomanic, and/or mixed episodes in a 12-month period. Rapid cycling is quite common in those with Bipolar II, much more so in women than in men (70% vs. 40%), and without treatment leads to added sources of disability and an increased risk of suicide. To improve a patient's prognosis, long-term therapy is most favorably recommended for controlling symptoms, maintaining remission and preventing relapses. With treatment, patients have been shown to present a decreased risk of suicide (especially when treated with lithium) and a reduction of frequency and severity of their episodes, which in turn moves them toward a stable life and reduces the time they spend ill. To maintain their state of balance, therapy is often continued indefinitely, as around 50% of the patients who discontinue it relapse quickly and experience either full-blown episodes or sub-syndromal symptoms that bring significant functional impairments.
Functioning
The deficits in functioning associated with Bipolar II disorder stem mostly from the recurrent depression that Bipolar II patients suffer from. Depressive symptoms are much more disabling than hypomanic symptoms and are potentially as, or more disabling than mania symptoms. Functional impairment has been shown to be directly linked with increasing percentages of depressive symptoms, and because sub-syndromal symptoms are more common—and frequent—in Bipolar II disorder, they have been implicated heavily as a major cause of psychosocial disability. There is evidence that shows the mild depressive symptoms, or even sub-syndromal symptoms, are responsible for the non-recovery of social functioning, which furthers the idea that residual depressive symptoms are detrimental for functional recovery in patients being treated for Bipolar II. It has been suggested that symptom interference in relation to social and interpersonal relationships in Bipolar II Disorder is worse than symptom interference in other chronic medical illnesses such as cancer. This social impairment can last for years, even after treatment that has resulted in a resolution of mood symptoms.
The factors related to this persistent social impairment are residual depressive symptoms, limited illness insight (a very common occurrence in patients with Bipolar II Disorder), and impaired executive functioning. Impaired ability in regards to executive functions is directly tied to poor psychosocial functioning, a common side-effect in patients with Bipolar II.
The impact on a patient's psychosocial functioning stems from the depressive symptoms (more common in Bipolar II than Bipolar I). An increase in these symptoms' severity seems to correlate with a significant increase in psychosocial disability. Psychosocial disability can present itself in poor semantic memory, which in turn affects other cognitive domains like verbal memory and (as mentioned earlier) executive functioning leading to a direct and persisting impact on psychosocial functioning.
An abnormal semantic memory organization can manipulate thoughts and lead to the formation of delusions and possibly affect speech and communication problems, which can lead to interpersonal issues. Bipolar II patients have also been shown to present worse cognitive functioning than those patients with Bipolar I, though they demonstrate about the same disability when it comes to occupational functioning, interpersonal relationships, and autonomy. This disruption in cognitive functioning takes a toll on their ability to function in the workplace, which leads to high rates of work loss in Bipolar II patient populations. After treatment and while in remission, Bipolar II patients tend to report a good psychosocial functioning but they still score less than patients without the disorder. These lasting impacts further suggest that a prolonged exposure to an untreated Bipolar II disorder can lead to permanent adverse effects on functioning.
Recovery and recurrence
Bipolar II Disorder has a chronic relapsing nature. It has even been suggested that Bipolar II patients have a higher degree of relapse than Bipolar I patients. Generally, within four years of an episode, around 60% of patients will relapse into another episode. Some patients are even symptomatic half the time, either with full on episodes or symptoms that fall just below the threshold of an episode.
Because of the nature of the illness, long-term therapy is the best option and aims to not only control the symptoms but to maintain sustained remission and prevent relapses from occurring. Even with treatment, patients do not always regain full functioning, especially in the social realm. There is a very clear gap between symptomatic recovery and full functional recovery for both Bipolar I and Bipolar II patients. As such, and because those with Bipolar II spend more time with depressive symptoms that do not quite qualify as a major depressive episode, the best chance for recovery is to have therapeutic interventions that focus on the residual depressive symptoms and to aim for improvement in psychosocial and cognitive functioning. Even with treatment, a certain amount of responsibility is placed in the patient's hands; they have to be able to assume responsibility for their illness by accepting their diagnosis, taking the required medication, and seeking help when needed to do well in the future.
Treatment often lasts after remission is achieved, and the treatment that worked is continued during the continuation phase (lasting anywhere from 6–12 months) and maintenance can last 1–2 years or, in some cases, indefinitely. One of the treatments of choice is Lithium, which has been shown to be very beneficial in reducing the frequency and severity of depressive episodes. Lithium prevents mood relapse and works especially well in Bipolar II patients who experience rapid-cycling. Almost all Bipolar II patients who take lithium have a decrease in the amount of time they spend ill and a decrease in mood episodes.
Along with medication, other forms of therapy have been shown to be beneficial for Bipolar II patients. A treatment called a "well-being plan" serves several purposes: it informs the patients, protects them from future episodes, teaches them to add value to their life, and works toward building a strong sense of self to fend off depression and reduce the desire to succumb to the seductive hypomanic highs. The plan has to aim high. Otherwise, patients will relapse into depression. A large part of this plan involves the patient being very aware of warning signs and stress triggers so that they take an active role in their recovery and prevention of relapse.
Mortality
Several studies have shown that the risk of suicide is higher in patients who suffer from Bipolar II than those who suffer from Bipolar I, and especially higher than patients who suffer from major depressive disorder.
In results of a summary of several lifetime study experiments, it was found that 24% of Bipolar II patients experienced suicidal ideation or suicide attempts compared to 17% in Bipolar I patients and 12% in major depressive patients. Bipolar disorders, in general, are the third leading cause of death in 15- to 24-year-olds. Bipolar II patients were also found to employ more lethal means and have more complete suicides overall.
Bipolar II patients have several risk factors that increase their risk of suicide. The illness is very recurrent and results in severe disabilities, interpersonal relationship problems, barriers to academic, financial, and vocational goals, and a loss of social standing in their community, all of which increase the likelihood of suicide. Mixed symptoms and rapid-cycling, both very common in Bipolar II, are also associated with an increased risk of suicide. The tendency for Bipolar II to be misdiagnosed and treated ineffectively, or not at all in some cases, leads to an increased risk.
As a result of the high suicide risk for this group, reducing the risk and preventing attempts remains a main part of the treatment; a combination of self-monitoring, close supervision by a therapist, and faithful adherence to their medication regimen will help to reduce the risk and prevent the likelihood of a completed suicide.
Suicide, which is both a stereotypic yet highly individualized act, is a common endpoint for many patients with severe psychiatric illness. The mood disorders (depression and bipolar manic-depression) are by far the most common psychiatric conditions associated with suicide. At least 25% to 50% of patients with bipolar disorder also attempt suicide at least once. With the exception of lithium—which is the most demonstrably effective treatment against suicide-remarkably little is known about specific contributions of mood-altering treatments to minimizing mortality rates in persons with major mood disorders in general and bipolar depression in particular. Suicide is usually a manifestation of severe psychiatric distress that is often associated with a diagnosable and treatable form of depression or other mental illness. In a clinical setting, an assessment of suicidal risk must precede any attempt to treat psychiatric illness.
History
In 19th century psychiatry, mania covered a broad range of intensity, and hypomania was equated by some to concepts of 'partial insanity' or monomania. A more specific usage was advanced by the German neuro-psychiatrist Emanuel Ernst Mendel in 1881, who wrote "I recommend (taking under consideration the word used by Hippocrates) to name those types of mania that show a less severe phenomenological picture, 'hypomania'". Narrower operational definitions of hypomania were developed from the 1960s/1970s.
The first diagnostic distinction to be made between manic-depression involving mania, and that involving hypomania, came from Carl Gustav Jung in 1903. In his paper, Jung introduced the non-psychotic version of the illness with the introductory statement, "I would like to publish a number of cases whose peculiarity consists in chronic hypomanic behaviour" where "it is not a question of real mania at all but of a hypomanic state which cannot be regarded as psychotic." Jung illustrated the hypomanic variation with five case histories, each involving hypomanic behaviour, occasional bouts of depression, and mixed mood states, which involved personal and interpersonal upheaval for each patient.
In 1975, Jung's original distinction between mania and hypomania gained support. Fieve and Dunner published an article recognizing that only individuals in a manic state require hospitalization. It was proposed that the presentation of either the one state or the other differentiates two distinct diseases; the proposition was initially met with skepticism. However, studies since confirm that bipolar II is a "phenomenologically" distinct disorder.
Empirical evidence, combined with treatment considerations, led the DSM-IV Mood Disorders Work Group to add bipolar II disorder as its own entity in the 1994 publication. (Only one other mood disorder was added to this edition, indicating the conservative nature of the DSM-IV work group.) In May 2013, the DSM-5 was released. Two revisions to the existing Bipolar II criteria are anticipated. The first expected change will reduce the required duration of a hypomanic state from four to two days. The second change will allow hypomania to be diagnosed without the manifestation of elevated mood;that is, increased energy/activity will be sufficient. The rationale behind the latter revision is that some individuals with Bipolar II manifest only visible changes in energy. Without presenting elevated mood, these individuals are commonly misdiagnosed with major depressive disorder. Consequently, they receive prescriptions for antidepressants, which unaccompanied by mood stabilizers, may induce rapid cycling or mixed states.
Society and culture
- Heath Black revealed in his autobiography, Black, that he has been diagnosed with Bipolar II.
- Maria Bamford has been diagnosed with Bipolar II.
- Geoff Bullock, singer-songwriter, was diagnosed with Bipolar II.
- Mariah Carey was diagnosed with Bipolar II in 2001. In 2018, publicly revealed and actively seeking treatment in the form of therapy and medication.
- Charmaine Dragun, former Australian journalist/newsreader. Inquest concluded she had Bipolar II.
- Joe Gilgun has been diagnosed with Bipolar II.
- Shane Hmiel has been diagnosed with Bipolar II.
- Jesse Jackson Jr. has been diagnosed with Bipolar II.
- Thomas Eagleton received a diagnosis of Bipolar II from Dr. Frederick K. Goodwin.
- Carrie Fisher had been diagnosed with Bipolar II.
- Albert Lasker is speculated to have had Bipolar II.
- Demi Lovato has been diagnosed with Bipolar II.
- Evan Perry, subject of the documentary Boy Interrupted, was diagnosed with Bipolar II.
- Sylvia Plath is speculated to have had Bipolar II.
- Richard Rossi, filmmaker, musician, and maverick minister was diagnosed with Bipolar II.
- Rumer has been diagnosed with Bipolar II.
- Robert Schumann is speculated to have had Bipolar II.
- Catherine Zeta-Jones received treatment for Bipolar II disorder after dealing with the stress of her husband's throat cancer. According to her publicist, Zeta-Jones made a decision to check into a "mental health facility" for a brief stay.
See also
- Bipolar disorder
- Bipolar I disorder
- Detailed listing of DSM-IV-TR bipolar disorder diagnostics codes
- Bipolar spectrum
- Cyclothymia
- Emotional dysregulation
- Creativity and bipolar disorder
- Bipolar disorders research
- Temporal lobe epilepsy