Coronary Artery Disease
Overview
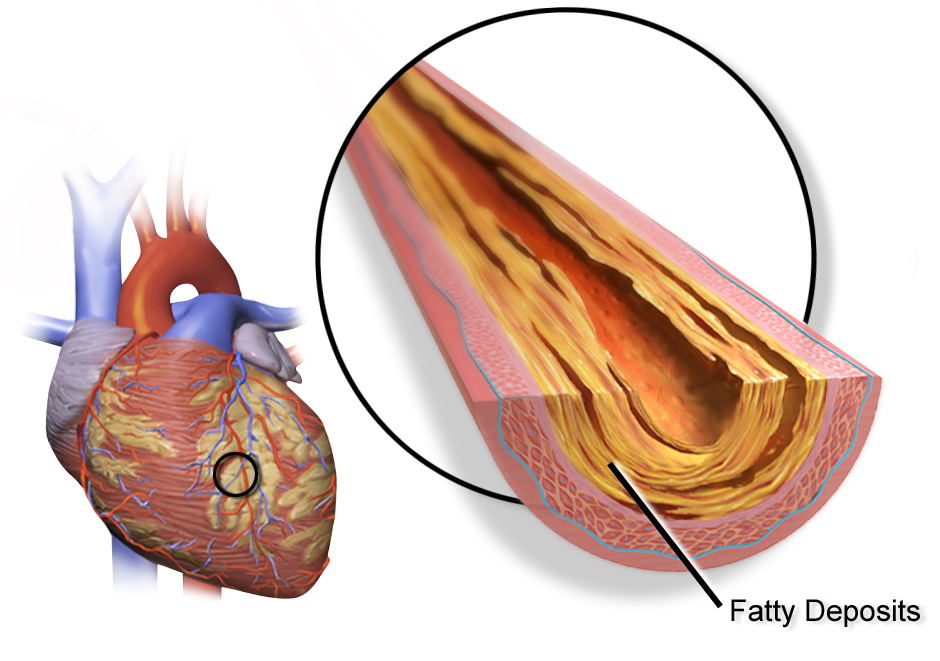
Coronary artery disease is a common heart condition. The major blood vessels that supply the heart (coronary arteries) struggle to send enough blood, oxygen and nutrients to the heart muscle. Cholesterol deposits (plaques) in the heart arteries and inflammation are usually the cause of coronary artery disease.
Signs and symptoms of coronary artery disease occur when the heart doesn't get enough oxygen-rich blood. If you have coronary artery disease, reduced blood flow to the heart can cause chest pain (angina) and shortness of breath. A complete blockage of blood flow can cause a heart attack.
Coronary artery disease often develops over decades. Symptoms may go unnoticed until a significant blockage causes problems or a heart attack occurs. Following a heart-healthy lifestyle can help prevent coronary artery disease.
Coronary artery disease may also be called coronary heart disease.
Symptoms
Symptoms may go unrecognized at first, or they may only occur when the heart is beating hard like during exercise. As the coronary arteries continue to narrow, less and less blood gets to the heart and symptoms can become more severe or frequent.
Coronary artery disease signs and symptoms can include:
- Chest pain (angina). You may feel pressure or tightness in your chest. Some people say it feels like someone is standing on their chest. The chest pain usually occurs on the middle or left side of the chest. Activity or strong emotions can trigger angina. The pain usually goes away within minutes after the triggering event ends. In some people, especially women, the pain may be brief or sharp and felt in the neck, arm or back.
- Shortness of breath. You may feel like you can't catch your breath.
- Fatigue. If the heart can't pump enough blood to meet your body's needs, you may feel unusually tired.
- Heart attack. A completely blocked coronary artery will cause a heart attack. The classic signs and symptoms of a heart attack include crushing chest pain or pressure, shoulder or arm pain, shortness of breath, and sweating. Women may have less typical symptoms, such as neck or jaw pain, nausea and fatigue. Some heart attacks don't cause any noticeable signs or symptoms.
When to see a doctor
If you think you're having a heart attack, immediately call 911 or your local emergency number. If you don't have access to emergency medical services, have someone drive you to the nearest hospital. Drive yourself only as a last option.
Smoking or having high blood pressure, high cholesterol, diabetes, obesity or a strong family history of heart disease makes you more likely to get coronary artery disease. If you're at high risk of coronary artery disease, talk to your health care provider. You may need tests to check for narrowed arteries and coronary artery disease.
Causes
Coronary artery disease starts when fats, cholesterols and other substances collect on the inner walls of the heart arteries. This condition is called atherosclerosis. The buildup is called plaque. Plaque can cause the arteries to narrow, blocking blood flow. The plaque can also burst, leading to a blood clot.
Besides high cholesterol, damage to the coronary arteries may be caused by:
- Diabetes or insulin resistance
- High blood pressure
- Not getting enough exercise (sedentary lifestyle)
- Smoking or tobacco use
Risk factors
Coronary artery disease is common. Age, genetics, other health conditions and lifestyle choices can affect the health of the heart arteries.
Coronary artery disease risk factors include:
- Age. Getting older increases the risk of damaged and narrowed arteries.
- Sex. Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
- Family history. A family history of heart disease makes you more likely to get coronary artery disease. This is especially true if a close relative (parent, sibling) developed heart disease at an early age. The risk is highest if your father or a brother had heart disease before age 55 or if your mother or a sister developed it before age 65.
- Smoking. If you smoke, quit. Smoking is bad for heart health. People who smoke have a significantly increased risk of heart disease. Breathing in secondhand smoke also increases the risk.
- High blood pressure. Uncontrolled high blood pressure can make arteries hard and stiff (arterial stiffness). The coronary arteries may become narrow, slowing blood flow.
- High cholesterol. Too much bad cholesterol in the blood can increase the risk of atherosclerosis. Bad cholesterol is called low-density lipoprotein (LDL) cholesterol. Not enough good cholesterol — called high-density lipoprotein (HDL) — also leads to atherosclerosis.
- Diabetes. Diabetes increases the risk of coronary artery disease. Type 2 diabetes and coronary artery disease share some risk factors, such as obesity and high blood pressure.
- Overweight or obesity. Excess body weight is bad for overall health. Obesity can lead to type 2 diabetes and high blood pressure. Ask your health care provider what a healthy weight is for you.
- Chronic kidney disease. Having long-term kidney disease increases the risk of coronary artery disease.
- Not getting enough exercise. Physical activity is important for good health. A lack of exercise (sedentary lifestyle) is linked to coronary artery disease and some of its risk factors.
- A lot of stress. Emotional stress may damage the arteries and worsen other risk factors for coronary artery disease.
- Unhealthy diet. Eating foods with a lot of saturated fat, trans fat, salt and sugar can increase the risk of coronary artery disease.
- Alcohol use. Heavy alcohol use can lead to heart muscle damage. It can also worsen other risk factors of coronary artery disease.
- Amount of sleep. Too little and too much sleep have both been linked to an increased risk of heart disease.
Risk factors often occur together. One risk factor may trigger another.
When grouped together, certain risk factors make you even more likely to develop coronary artery disease. For example, metabolic syndrome — a cluster of conditions that includes high blood pressure, high blood sugar, excess body fat around the waist and high triglyceride levels — increases the risk of coronary artery disease.
Sometimes coronary artery disease develops without any classic risk factors. Other possible risk factors for coronary artery disease may include:
- Breathing pauses during sleep (obstructive sleep apnea). This condition causes breathing to stop and start during sleep. It can cause sudden drops in blood oxygen levels. The heart must work harder. Blood pressure goes up.
- High-sensitivity C-reactive protein (hs-CRP). This protein appears in higher-than-usual amounts when there's inflammation somewhere in the body. High hs-CRP levels may be a risk factor for heart disease. It's thought that as coronary arteries narrow, the level of hs-CRP in the blood goes up.
- High triglycerides. This is a type of fat (lipid) in the blood. High levels may raise the risk of coronary artery disease, especially for women.
- Homocysteine. Homocysteine is an amino acid the body uses to make protein and to build and maintain tissue. But high levels of homocysteine may increase the risk of coronary artery disease.
- Preeclampsia. This pregnancy complication causes high blood pressure and increased protein in the urine. It can lead to a higher risk of heart disease later in life.
- Other pregnancy complications. Diabetes or high blood pressure during pregnancy are also known risk factors for coronary artery disease.
- Certain autoimmune diseases. People who have conditions such as rheumatoid arthritis and lupus (and other inflammatory conditions) have an increased risk of atherosclerosis.
Complications
Coronary artery disease can lead to:
- Chest pain (angina). When the coronary arteries narrow, the heart may not get enough blood when it needs it most — like when exercising. This can cause chest pain (angina) or shortness of breath.
- Heart attack. A heart attack can happen if a cholesterol plaque breaks open and causes a blood clot to form. A clot can block blood flow. The lack of blood can damage the heart muscle. The amount of damage depends in part on how quickly you are treated.
- Heart failure. Narrowed arteries in the heart or high blood pressure can slowly make the heart weak or stiff so it's harder to pump blood. Heart failure is when the heart doesn't pump blood as it should.
- Irregular heart rhythms (arrhythmias). Not enough blood to the heart can alter normal heart signaling, causing irregular heartbeats.
Prevention
The same lifestyle habits used to help treat coronary artery disease can also help prevent it. A healthy lifestyle can help keep the arteries strong and clear of plaque. To improve heart health, follow these tips:
- Quit smoking.
- Control high blood pressure, high cholesterol and diabetes.
- Exercise often.
- Maintain a healthy weight.
- Eat a low-fat, low-salt diet that's rich in fruits, vegetables and whole grains.
- Reduce and manage stress.
Diagnosis
To diagnose coronary artery disease, a health care provider will examine you. You'll likely be asked questions about your medical history and any symptoms. Blood tests are usually done to check your overall health.
Tests
Test to help diagnose or monitor coronary artery disease include:
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. It can show how fast or slow the heart is beating. Your provider can look at signal patterns to determine if you're having or had a heart attack.
-
Echocardiogram. This test uses sound waves to create pictures of the beating heart. An echocardiogram can show how blood moves through the heart and heart valves.
Parts of the heart that move weakly may be caused by a lack of oxygen or a heart attack. This may be a sign of coronary artery disease or other conditions.
- Exercise stress test. If signs and symptoms occur most often during exercise, your provider may ask you to walk on a treadmill or ride a stationary bike during an ECG. If an echocardiogram is done while you do these exercises, the test is called a stress echo. If you can't exercise, you might be given medications that stimulate the heart like exercise does.
- Nuclear stress test. This test is similar to an exercise stress test but adds images to the ECG recordings. A nuclear stress test shows how blood moves to the heart muscle at rest and during stress. A radioactive tracer is given by IV. The tracer helps the heart arteries show up more clearly on images.
-
Heart (cardiac) CT scan. A CT scan of the heart can show calcium deposits and blockages in the heart arteries. Calcium deposits can narrow the arteries.
Sometimes dye is given by IV during this test. The dye helps create detailed pictures of the heart arteries. If dye is used, the test is called a CT coronary angiogram.
-
Cardiac catheterization and angiogram. During cardiac catheterization, a heart doctor (cardiologist) gently inserts a flexible tube (catheter) into a blood vessel, usually in the wrist or groin. The catheter is gently guided to the heart. X-rays help guide it. Dye flows through the catheter. The dye helps blood vessels show up better on the images and outlines any blockages.
If you have an artery blockage that needs treatment, a balloon on the tip of the catheter can be inflated to open the artery. A mesh tube (stent) is typically used to keep the artery open.
Treatment
Treatment for coronary artery disease usually involves lifestyle changes such as not smoking, eating healthy and exercising more. Sometimes, medications and procedures are needed.
Medications
There are many drugs available to treat coronary artery disease, including:
- Cholesterol drugs. Medications can help lower bad cholesterol and reduce plaque buildup in the arteries. Such drugs include statins, niacin, fibrates and bile acid sequestrants.
-
Aspirin. Aspirin helps thin the blood and prevent blood clots. Daily low-dose aspirin therapy may be recommended for the primary prevention of heart attack or stroke in some people.
Daily use of aspirin can have serious side effects, including bleeding in the stomach and intestines. Don't start taking a daily aspirin without talking to your health care provider.
- Beta blockers. These drugs slow the heart rate. They also lower blood pressure. If you've had a heart attack, beta blockers may reduce the risk of future attacks.
- Calcium channel blockers. One of these drugs may be recommended if you can't take beta blockers or beta blockers don't work. Calcium channel blockers can help improve symptoms of chest pain.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs). These medicines lower blood pressure. They may help keep coronary artery disease from getting worse.
- Nitroglycerin. This medicine widens the heart arteries. It can help control or relieve chest pain. Nitroglycerin is available as a pill, spray or patch.
- Ranolazine. This medication may help people with chest pain (angina). It may be prescribed with or instead of a beta blocker.
Surgeries or other procedures
Sometimes, surgery is needed to fix a blocked artery. Some options are:
-
Coronary angioplasty and stent placement. This procedure is done to open clogged heart arteries. It may also be called percutaneous coronary intervention (PCI). The heart doctor (cardiologist) guides a thin, flexible tube (catheter) to the narrowed part of the heart artery. A tiny balloon is inflated to help widen the blocked artery and improve blood flow.
A small wire mesh tube (stent) may be placed in the artery during angioplasty. The stent helps keep the artery open. It lowers the risk of the artery narrowing again. Some stents slowly release medication to help keep the arteries open.
- Coronary artery bypass graft surgery (CABG). A surgeon takes a healthy blood vessel from another part of the body to create a new path for blood in the heart. The blood then goes around the blocked or narrowed coronary artery. CABG is an open-heart surgery. It's usually done only in those with many narrowed heart arteries.
Clinical trials
Explore Mayo Clinic studies testing new treatments, interventions and tests as a means to prevent, detect, treat or manage this condition.
Lifestyle and home remedies
Making certain lifestyle changes can help keep the arteries healthy and can prevent or slow coronary artery disease. Try these heart-healthy tips:
- Don't smoke. Smoking is a major risk factor for coronary artery disease. Nicotine tightens blood vessels and forces the heart to work harder. Not smoking is one of the best ways to lower the risk of a heart attack.
- Control blood pressure. Adults should get their blood pressure checked by a health care provider at least every two years. You may need more-frequent checks if you have a history of high blood pressure. Ask your health care provider what blood pressure goal is best for you.
- Manage cholesterol. Adults should get a cholesterol test when in their 20s and at least every five years after. Some people need more-frequent checks. The optimal LDL cholesterol level is lower than 130 milligrams per deciliter (mg/dL), or 3.4 millimoles per liter (mmol/L). But it depends on your overall health. If you have other risk factors for heart disease, your target LDL cholesterol may be below 100 mg/dL (2.6 mmol/L). Ask your provider what your cholesterol levels should be.
- Check your blood sugar. If you have diabetes, carefully managing your blood sugar can help reduce the risk of heart disease.
- Eat heart-healthy foods. Eat plenty of fruits, vegetables, whole grains, legumes and nuts. Avoid saturated fats and trans fats. Reduce salt and sugar. Eating one or two servings of fish a week also may help keep the heart healthy.
- Avoid or limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Get moving. Exercise helps manage weight and control diabetes, high cholesterol and high blood pressure — all risk factors for coronary artery disease. Get at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity a week, or a combination of moderate and vigorous activity.
- Maintain a healthy weight. Being overweight increases the risk of coronary artery disease. Losing even a small amount of weight can help reduce risk factors for coronary artery disease.
- Ask about cardiac rehabilitation. If you've had heart surgery, your doctor may suggest a program of education, counseling and exercise training that's designed to help improve your health.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to tame stress.
- Get recommended vaccines. Get a flu (influenza) vaccine each year.
Regular medical checkups are important. Some of the main risk factors for coronary artery disease — high cholesterol, high blood pressure and diabetes — have no symptoms in the early stages. Early detection and treatment can help you maintain better heart health.
Alternative medicine
Omega-3 fatty acids are a type of unsaturated fatty acid. It's thought that they can lower inflammation throughout the body. Inflammation has been linked to coronary artery disease. However, the pros and cons of omega-3 fatty acids for heart disease continue to be studied.
Sources of omega-3 fatty acids include:
- Fish and fish oil. Fish and fish oil are the most effective sources of omega-3 fatty acids. Fatty fish — such as salmon, herring and light canned tuna — contain the most omega-3 fatty acids and, therefore, the most benefit. Fish oil supplements may offer benefit, but the evidence is strongest for eating fish.
- Flax and flaxseed oil. Flax and flaxseed oil contain a type of omega-3 fatty acid called alpha-linolenic acid (ALA). ALA contains smaller amounts of omega-3 fatty acids than do fish and fish oil. ALA may help lower cholesterol and improve heart health. But research is mixed. Some studies haven't found ALA to be as effective as fish. Flaxseed also contains a lot of fiber, which has various health benefits.
- Other oils. Alpha-linolenic acid (ALA) can also be found in canola oil, soybeans and soybean oil.
Other supplements may help lower blood pressure or cholesterol — two risk factors for coronary artery disease. Some that may be effective are:
- Barley
- Psyllium, a type of fiber
- Oats, a type of fiber that includes beta-glucans and is found in oatmeal and whole oats
- Garlic
- Plant sterols (found in supplements and some margarines, such as Promise, Smart Balance and Benecol)
Always talk to a health care provider before taking herbs, supplements or medications bought without a prescription. Some drugs and supplements can interfere with other drugs.
Preparing for your appointment
If you have symptoms of coronary artery disease or any risk factors, make an appointment with your health care provider. You may be referred to a heart specialist (cardiologist).
Here's some information to help you get ready for your appointment and to know what to expect from your doctor.
What you can do
- Be aware of any pre-appointment restrictions. When you make the appointment, ask if there's anything you need to do in advance, such as restrict your diet. You may need to avoid food or drinks for a short while before some tests.
- Write down any symptoms you're having, including any that may seem unrelated to coronary artery disease.
- Write down your medical information, including other conditions you have and any family history of heart disease.
- Bring a list of medications with you to your appointment. Include doses.
- Ask a family member or friend to go with you to the appointment, if possible. An extra person can help you remember what the provider says.
- Write down questions to ask your health care provider.
Questions to ask your health care provider at your first appointment include:
- What is causing my symptoms?
- What tests do I need?
- Should I see a specialist?
- Do I need to follow any restrictions while I wait for my next appointment?
- When should I call 911 or emergency medical help for my symptoms?
If you're referred to a heart doctor (cardiologist) for coronary artery disease, you may want to ask these questions:
- What is my risk of long-term complications from coronary artery disease?
- What treatment do you recommend?
- If I need medication, what are the possible side effects?
- Do I need surgery? Why or why not?
- What diet and lifestyle changes should I make?
- What restrictions do I need to follow, if any?
- How frequently will you see me for follow-up visits?
- I have other health problems. How can I best manage these conditions together?
Don't hesitate to ask additional questions about your condition.
What to expect from your doctor
A health care provider who sees you for coronary artery disease may ask:
- What are your symptoms?
- When did you begin having symptoms?
- Have the symptoms gotten worse over time?
- Do you have chest pain or difficulty breathing?
- Does exercise or activity make the symptoms worse?
- Do you have heart problems in your family?
- Have you been diagnosed with other health conditions?
- What medications do you take?
- Have you ever had radiation therapy?
- How much do you exercise in a typical week?
- What's your typical daily diet?
- Do you or did you smoke? How much? If you quit, when?
- Do you drink alcohol? How much?
What you can do in the meantime
It's never too early to make healthy lifestyle changes, such as quitting smoking, eating healthy foods and getting more exercise. These habits protect against coronary artery disease and its complications, including heart attack and stroke.