Emery-Dreifuss Muscular Dystrophy 1, X-Linked
A number sign (#) is used with this entry because X-linked Emery-Dreifuss muscular dystrophy-1 (EDMD1) is caused by mutation in the gene encoding emerin (EMD; 300384) on chromosome Xq28.
DescriptionEmery-Dreifuss muscular dystrophy is a degenerative myopathy characterized by weakness and atrophy of muscle without involvement of the nervous system. Flexion deformities of the elbows dating from early childhood, mild pectus excavatum, signs of cardiac involvement and absence of muscle pseudohypertrophy, involvement of the forearm muscles, and mental retardation distinguish the Emery-Dreifuss form (EDMD1) from the Becker form (300376).
Genetic Heterogeneity of Emery-Dreifuss Muscular Dystrophy
Autosomal dominant Emery-Dreifuss muscular dystrophy-2 (EDMD2; 181350), is caused by mutation in the lamin A/C gene (LMNA; 150330); autosomal recessive EDMD3 (616516) is also caused by mutation in the LMNA gene. Additional autosomal dominant forms include EDMD4 (612998), caused by mutation in the SYNE1 gene (608441), EDMD5 (612999), caused by mutation in the SYNE2 gene (608442), and EDMD7 (614302), caused by mutation in the TMEM43 gene (612048). A second X-linked form (EDMD6; see 300696) is caused by mutation in the FHL1 gene (300163).
Clinical FeaturesDreifuss and Hogan (1961) and Emery and Dreifuss (1966) studied a Virginia kindred in which there were 8 affected males in 3 generations in a typical X-linked pedigree pattern. Onset of muscle weakness, first affecting the lower extremities with a tendency to walk on the toes, was noted around the age of 4 or 5 years. By the early teens, waddling gait with increased lumbar lordosis was marked and weakness of the shoulder girdle musculature appeared later. Slow progression with continued gainful employment is the rule.
Cardiac
The cardiac conduction defect in EDMD patients is the most serious and life-threatening clinical manifestation of the disease.
Cardiac defects have been described in female carriers (Emery, 1989) in the absence of any skeletal muscle abnormality, suggesting a prominent role in cardiac conduction for emerin.
Becker (1972) republished illustrations of typical cases reported by Cestan and LeJonne (1902). Dickey et al. (1984) reported a large kindred in which adults, both male hemizygotes and female heterozygotes, had lethal cardiac disease characterized especially by atrial arrhythmias. Skinner and Emery (1974) pointed out that the serum creatine kinase of carriers is elevated mainly in young women and gave a 'normal' curve for carrier and noncarrier women.
After a period of 25 years, Emery (1987) reinvestigated the original Virginia family. He confirmed that cardiomyopathy, presenting most often as atrioventricular block, is a significant feature of the disease, which is characterized by the triad of (1) slowly progressive muscle wasting and weakness with humeroperoneal distribution in the early stages; (2) early contractures of the elbows, Achilles tendons, and postcervical muscles; and (3) cardiomyopathy.
Takahashi (1971) reported the same disorder as Mawatari and Katayama (1973) in 2 brothers. Wright and Elsas (1980) provided genetic studies of the kindred discussed by Waters et al. (1975). The onset was in the teens, with total disability by the third decade and death by age 50. Type I muscle fibers were affected, resulting in an unusual distribution of atrophy in the proximal upper and distal lower limbs. Cardiac conduction defects often preceded overt muscle atrophy. Cardiac signs began with small P waves and prolonged PR intervals, and progressed to complete AV heart block with bradycardiac idioventricular rhythms and atrial paralysis requiring pacemaker implantation. Cardiac signs were detected as early as age 12. The earliest pacemaker insertion was in a 20-year-old male who could still do heavy physical labor. In the absence of gross muscle atrophy, he had markedly elevated creatine phosphokinase (CPK) levels. In some, contractures at the elbows were evident as early as age 13. Contractures also developed in the neck and Achilles tendons.
Buckley et al. (1999) investigated the cardiac status in 3 patients with EDMD. The effect on the heart became apparent in the teenage years and was characterized by cardiac conduction defects and infiltration of the myocardium by fibrous and adipose tissue. It first affected the atria, which resulted in atrial paralysis; treatment with ventricular pacing was usually needed. The authors found that female carriers can develop heart problems and are at risk of sudden death.
Skeletal
Dubowitz (1973) gave the name rigid spine syndrome to the disorder in a 17-year-old boy with a myopathy and stiffness of the back and neck from an early age and progressive scoliosis in his teens. For several years he had had difficulty in extending his elbows. Creatine phosphokinase was moderately elevated. Dubowitz (1973) made reference to 3 other similar cases he had seen. Wettstein et al. (1983) suggested that this may be an X-linked disorder and may be related to the Emery-Dreifuss muscular dystrophy with contractures. Rigid spine syndrome (602771) is distinguished from Emery-Dreifuss muscular dystrophy by lack of cardiac involvement and autosomal recessive inheritance.
Scapuloperoneal Syndrome
Although Davidenkow (1939) of Leningrad considered X-linked scapuloperoneal syndrome to be a distinct disorder, many kindreds reported to have an X-linked scapuloperoneal syndrome, or humeroperoneal neuromuscular disease, have been determined to have Emery-Dreifuss muscular dystrophy.
Under the designation scapuloperoneal syndrome, Thomas et al. (1972) described a kindred with typical X-linked inheritance of a myopathy manifesting as muscular weakness and wasting, affecting predominantly the proximal muscles of the legs. Accompanying features were contractures of the elbows, pes cavus, and, in adulthood, cardiomyopathy. Pseudohypertrophy was absent. Close linkage with deutan colorblindness (303800) was found. The authors pointed out similarities to the Emery benign type of muscular dystrophy with contractures but thought that the distribution of muscular involvement distinguished the two. They later revised their opinion and concluded that the disorder is in fact EDMD (Thomas and Petty, 1985).
Many studies reached the conclusion that X-linked scapuloperoneal syndrome was the same condition as Emery-Dreifuss muscular dystrophy (Rotthauwe et al., 1972; Mawatari and Katayama, 1973; Rowland et al., 1979; Sulaiman et al., 1981; Thomas and Petty, 1985; Merlini et al., 1986).
Goldblatt et al. (1989) presented clinical and molecular genetic evidence that the Emery-Dreifuss syndrome and X-linked muscular dystrophy with contractures are genetically homogeneous.
Emery (1989) insisted that the designation scapuloperoneal syndrome should be reserved for an autosomal dominant disorder that can be either myopathic (181430) or more often neuropathic (181400), has later onset (in adulthood) with late development of contractures, and does not show cardiac conduction defects.
Limb-Girdle Presentation
Ura et al. (2007) reported 2 unrelated males with EDMD confirmed by genetic analysis who presented with limb-girdle muscular dystrophy. The first patient was a 9-year-old boy who developed proximal muscle weakness and atrophy of the lower limbs, waddling gait, and lordotic posture by age 6. He had showed unsteady gait at age 4. Serum creatine kinase was increased and muscle biopsy showed moderate fiber size variation, internalized nuclei, and absence of emerin staining. Electrocardiogram revealed transient sinus arrhythmia. The second patient was a 50-year-old man who noted progressive proximal muscle weakness in the lower limbs beginning at age 35. He had waddling gait, Gowers sign, and minimal joint contractures. Cardiac studies showed valvular insufficiency and atrioventricular block. The findings expanded the phenotypic features associated with X-linked EDMD.
InheritanceEmery-Dreifuss muscular dystrophy-1 is inherited as an X-linked recessive disorder.
Rudenskaya et al. (1994) described Emery-Dreifuss muscular dystrophy in 4 generations of a family and concluded that the inheritance was autosomal dominant, but the pedigree was also consistent with X-linked dominant inheritance, since all daughters of affected males were affected. The females may have been less severely affected; one, aged 29 years, worked as a crane-driver. They also described 2 sporadic cases, both in males; 1 closely resembled rigid spine syndrome. Rudenskaya et al. (1994) commented on the remarkable intra- and interfamilial variation in the clinical manifestations of EDMD.
DiagnosisManilal et al. (1996) showed that muscle biopsy from an EDMD patient showed complete absence of emerin by both Western blotting and immunohistology and suggested that a simple diagnostic antibody test may be carried out for this disorder.
Nevo et al. (1999), who identified a different mutation in emerin in each of 3 families with EDMD, emphasized the usefulness of early diagnosis because insertion of a pacemaker may be life saving. They also emphasized the finding of numerous private mutations, suggesting that detection of the presence or absence of the emerin protein in tissues may be more practical as a diagnostic tool than mutation screening.
Fujimoto et al. (1999) reported a case of X-linked EDMD in a 3-year-old boy with contractures of the Achilles tendons, but without characteristic contractures of the elbows and cardiac involvement. In immunofluorescent staining of a muscle biopsy, no emerin was noted on the nuclear membrane. RT-PCR and PCR-based genomic DNA analysis of the emerin gene revealed no amplification products in the patient's samples. The authors stressed that emerin staining should be part of the work-up of every unexplained muscular dystrophy, because the early diagnosis of EDMD is very important, especially to avoid cardiac complications that may cause sudden death.
Biochemical FeaturesPearson et al. (1965) found a difference of muscle LDH electrophoretic pattern in Emery-Dreifuss muscular dystrophy as compared with the Duchenne type.
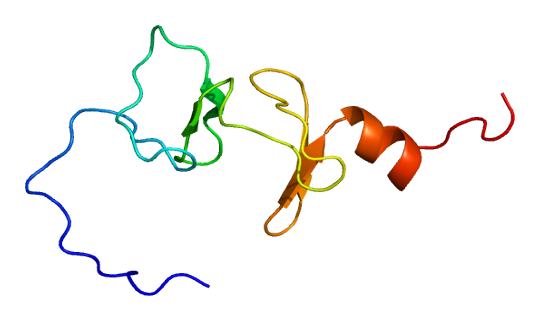
PathogenesisEmerin, the product of the EMD gene, is a ubiquitous protein that decorates the nuclear rim of many cell types. These findings could not explain, however, the role of emerin nor account for the skeletal muscle- and heart-specific manifestations associated with the disorder. Using 2 antisera against synthetic peptide fragments predicted from emerin cDNA, Nagano et al. (1996) found positive nuclear membrane staining in skeletal, cardiac, and smooth muscles in normal controls and in patients with neuromuscular diseases other than EDMD. In contrast, a deficiency in immunofluorescent staining of skeletal and cardiac muscle from EDMD patients was observed.
In heart, the specific localization of emerin to desmosomes and fasciae adherentes could account for the characteristic conduction defects described in patients with Emery-Dreifuss muscular dystrophy (Cartegni et al., 1997).
Manilal et al. (1999) found that affinity-purified antibodies against emerin gave immunostaining only in the nuclear membrane, casting doubt on the hypothesis that cardiac defects in EDMD are caused by absence of emerin from intercalated discs (Cartegni et al., 1997). Although emerin was abundant in the membranes of cardiomyocyte nuclei, it was absent from any nonmyocyte cells in the heart. This distribution of emerin was similar to that of lamin A (LMNA; 150330), which is mutant in the autosomal Emery-Dreifuss syndromes (181350). In contrast, laminin B1 (LMNB1; 150340) was absent from cardiomyocyte nuclei, showing that lamin B1 is not essential for localization of emerin to the nuclear lamina. Lamin B1 was also almost completely absent from skeletal muscle nuclei. Manilal et al. (1999) suggested that in EDMD the additional absence of lamin B1 from heart and skeletal muscle nuclei that already lack emerin may explain why these tissues are particularly affected. They further suggested that a functional interaction between emerin and lamin A in nuclei could explain the identical phenotype in the 2 forms of EDMD.
Using FISH and immunofluorescence, Boyle et al. (2001) analyzed the nuclear organization of every human chromosome in diploid lymphoblasts and primary fibroblasts. Most gene-rich chromosomes were concentrated at the center of the nucleus, whereas the more gene-poor chromosomes were located towards the nuclear periphery. There was no significant relationship between chromosome size and position within the nucleus. The intranuclear organization of chromosomes from an individual with X-linked EDMD was not altered in cells lacking the nuclear membrane protein emerin. The authors suggested that emerin may not be necessary for localizing chromosomes at the nuclear periphery, and that the muscular dystrophy phenotype in such individuals may not be due to grossly altered nuclear organization of chromatin.
Zhang et al. (2007) identified mutations in the SYNE1 and SYNE2 genes in patients with EDMD4 and EDMD5. Skin fibroblasts from these patients showed similar defects in nuclear morphology as those described in patients with EDMD due to mutations in the LMNA and EMD genes. SYNE1 and SYNE2 mutant fibroblasts showed a convoluted appearance with micronuclei, giant, and fragmented nuclei, and chromatin reorganization. Patient fibroblasts and muscle cells showed loss of nuclear envelope integrity with mislocalization of LMNA and emerin. Immunofluorescent studies showed loss of SYNE1 or SYNE2 expression in the nuclear envelope and mitochondria of patient fibroblasts. These same changes were also observed in fibroblasts from patients with other genetic forms of EDMD, indicating that loss of nesprin is a characteristic of all forms of EDMD. RNA interference of SYNE1 or SYNE2 recapitulated the nuclear defects membrane defects and changes in the organization of intranuclear heterochromatin observed in patient cells. Overall, the findings showed the importance of the nesprin/emerin/lamin complex in the maintenance of nuclear stability, and suggested that changes in the binding stoichiometry of these proteins is a common feature of EDMD. Zhang et al. (2007) concluded that the disorder is caused in part by uncoupling of the nucleoskeleton and cytoskeleton.
MappingConsistent with the suggested linkage of EDMD with deutan colorblindness (303800; Thomas et al., 1972), Boswinkel et al. (1985) reported possible linkage between EDMD and DXS15, which is located at Xq28 (2 recombinants out of 16 informative meioses). Thomas et al. (1986) found close linkage with factor VIII and with DXS15 in a large family reported in detail by Hopkins et al. (1981). Yates et al. (1986) found no recombination in 11 phase-known meioses informative for the factor VIII gene and 8 phase-known meioses informative for DXS15, giving maximum lod scores of 3.50 and 2.50, respectively, at a recombination fraction of 0. DXS52 (St14) showed 1 recombinant in 12 phase-known meioses, giving a maximum lod score of 2.62 at a recombination fraction of 0.07. Hodgson et al. (1986) found evidence of linkage to markers located at Xq28, thus supporting the observations of others on the location of this form of muscular dystrophy.
Romeo et al. (1988) concluded that the EDMD locus is probably located distal to DXS15; the sum of lod scores from this study and from 2 previous ones was 6.31 at theta = 0.10. In 2 families living in northern Georgia and Alabama, previously described by Waters et al. (1975), Wright and Elsas (1980), and Hopkins et al. (1981), Consalez et al. (1991) found that EDMD is approximately 2 cM from DXS52 (lod = 15.67) and very close to F8C and the red/green color vision loci (see 300821), with respective lod scores of 9.62 and 10.77, without a recombinant. Several instances of recombination between EDMD and 3 proximal Xq28 markers suggested that the gene is located in distal Xq28, probably distal to DXS305. Yates et al. (1993) concluded from a multipoint analysis incorporating published data as well as their own that EDMD and red-green cone pigments (which lie close to each other) are flanked proximally by DXS52 (interval = 2 cM) and distally by F8C (interval = 3 cM).
Molecular GeneticsAmong the many genes located in the distal part of Xq28, Bione et al. (1994) selected 8 transcripts expressed at high levels in skeletal muscle, heart, and/or brain as the best candidates for the site of the mutation causing EDMD. On further study, they found that each of the 5 patients investigated had a unique mutation in one of the genes, previously symbolized STA; see 300384.0001-300384.0005. These mutations resulted in the loss of all or part of the protein.
Wulff et al. (1997) designed a set of primers optimized to amplify and sequence each of the 6 EMD exons. With a heteroduplex analysis of emerin gene exons in 30 unrelated EDMD patients, abnormal patterns of single exons were found in 7 patients. Direct sequencing of the respective exons revealed 6 novel mutations distributed in the promoter region and exons 3-6. This study identified the first mutations in the promoter region and in exon 5. A total of 25 mutations were then known. All of the mutations abolished the synthesis of functional emerin.
Genotype/Phenotype CorrelationsEllis et al. (1999) stated that more than 70 different mutations causing EDMD had been identified in the emerin gene. They described 2 missense mutations involving proline-183 (300384.0008-300384.0009). Biochemical analyses had demonstrated that the mobility and expression levels of the mutant forms of emerin are indistinguishable from those of wildtype emerin, but that they have weakened interactions with nuclear lamina components. In comparison with the usual EDMD phenotype, patients with P183 missense mutations had a later age at onset of first symptoms, elbow contractures, ankle contractures, and upper and lower limb weakness, but there was no difference for the age at onset of cardiac involvement.
In 2 brothers with EDMD, Hoeltzenbein et al. (1999) identified a TCTAC deletion spanning nucleotides 631-635 of the emerin gene (310300.0010). Both showed an unusually severe disease phenotype. The same mutation had been found in 2 brothers with a significantly milder phenotype from an unrelated family (Manilal et al., 1998). The interfamilial heterogeneity in the 2 families was thought to be due to environmental or genetic modification of the disease.
Ben Yaou et al. (2007) reported a large consanguineous Algerian family with digenic inheritance of mutations in the EMD and LMNA genes. Of 9 living affected family members, 6 (3 males and 3 females) had isolated atrial cardiac disease with conduction abnormalities, 1 female had isolated Charcot-Marie-Tooth axonal sensory neuropathy (CMT2B1; 605588), and 2 males had severe Emery-Dreifuss muscular dystrophy, cardiac disease, and CMT. Transmission of the atrial cardiac disease in this family was consistent with X-linked inheritance, and all 6 patients with isolated atrial cardiac disease had a deletion in the EMD gene. All 3 patients with CMT2B1 had a homozygous LMNA mutation (R298C; 150330.0020). The 2 male patients with all 3 phenotypes had both the homozygous LMNA mutation and the EMD deletion. Heterozygous carriers of the LMNA mutation had no associated phenotype. Three affected males carrying the hemizygous EMD deletion, including 1 without and 2 with a heterozygous LMNA mutation, did not have features of muscular dystrophy. A fourth male patient carrying the EMD deletion and without the LMNA mutation was asymptomatic; however, the 3 males with isolated atrial cardiac disease were all over 40 years of age, and the fourth male was 32 years of age. Ben Yaou et al. (2007) concluded that the EMD deletion acted in a dominant fashion and could alone cause isolated atrial cardiac disease in both men and women, but not a complete EDMD phenotype in men. Coexistence of the homozygous LMNA mutation and the hemizygous EMD deletion in men both worsened the cardiac impairment and caused axonal neuropathy and muscular dystrophy, suggesting a synergistic effect of the 2 mutations.