Lymphangioleiomyomatosis
A number sign (#) is used with this entry because lymphangioleiomyomatosis (LAM) can occur in association with tuberous sclerosis complex (TSC; 191100) due to mutations in the TSC1 (605284) or TSC2 (191092) genes. Sporadic LAM typically results from 2 somatic mutations in the TSC2 gene, although a fraction of sporadic LAM is caused by germline mutations in the TSC1 gene.
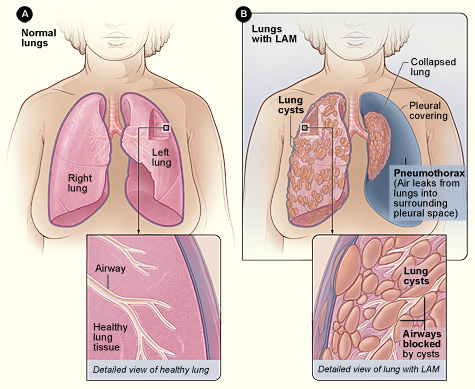
Clinical FeaturesPulmonary lymphangiomyomatosis, also known as pulmonary lymphangioleiomyomatosis (Urban et al., 1999), is a rare disease that occurs almost exclusively in women. It was first described by Van Stossel (1937). The average age at onset of symptoms, which include shortness of breath (67%), lung collapse (25%), coughing (12%), and chest pain (10%), is 33 years (Taylor et al., 1990; Johnson et al., 1993). Chest x-rays typically show a diffuse interstitial infiltrate, with no predominance in any 1 lung zone. Although most cases of LAM are pulmonary, cases with retroperitoneal, pelvic, or perirenal involvement in lymph nodes and extranodal sites have been reported (Torres et al., 1995). The disorder is usually diagnosed by open lung biopsy. Microscopically, there is cystic distortion of the normal pulmonary architecture by an atypical smooth muscle infiltrate. Most patients have a slowly declining clinical course. Lung transplantation is the only effective therapy for patients with end-stage disease (Boehler et al., 1996). Lymphangiomyomatosis can occur as an isolated disorder or in association with TSC. Among patients with TSC, it is said to be the third most frequent cause of TSC-related death, after renal disease and brain tumors (Castro et al., 1995).
Molecular GeneticsRenal angiomyolipomas occur in approximately 50% of sporadic LAM patients and in 70% of TSC patients. Loss of heterozygosity (LOH) in the chromosomal region for the TSC2 gene occurs in 60% of TSC-associated angiomyolipomas. Because of the similar pulmonary and renal manifestations of TSC and sporadic LAM, Smolarek et al. (1998) hypothesized that LAM and TSC have a common genetic basis. They analyzed renal angiomyolipomas from 13 women with sporadic LAM for LOH in the region of the TSC1 (9q34) and TSC2 (16p13) genes. TSC2 LOH was detected in 7 (54%) of the angiomyolipomas. They also found TSC2 LOH in 4 lymph nodes from a woman with retroperitoneal LAM. No TSC1 LOH was found. The findings indicated that the TSC2 gene may be involved in the pathogenesis of sporadic LAM. They noted, however, that genetic transmission of LAM had not been reported. Women with LAM may have low penetrance germline TSC2 mutations, or they may be mosaic, with TSC2 mutations in the lung and the kidney but not in other organs. Examination of DNA from peripheral blood lymphocytes or lymphoblastoid cells of 12 LAM patients and culture of lung cells taken at the time of transplantation for LAM in 8 patients did not reveal any TSC2 mutations (Astrinidis et al., 2000). In 69 patients with pulmonary lymphangioleiomyomatosis, all women, Urban et al. (1999) found no familial instance.
Carsillo et al. (2000) described mutations in the TSC2 gene as a cause of sporadic pulmonary lymphangioleiomyomatosis. They identified somatic TSC2 mutations in 5 of 7 angiomyolipomas from sporadic LAM patients. In all 4 patients from whom lung tissue was available, the same mutation found in the angiomyolipoma was present in the abnormal pulmonary smooth muscle cells. In no case was the mutation present in normal kidney, morphologically normal lung, or lymphoblastoid cells. TSC2 LOH was present in 4 of the 5 angiomyolipomas in which the authors identified TSC2 mutations. Therefore, these 4 angiomyolipomas had inactivation of both alleles of TSC2, consistent with the Knudson 2-hit hypothesis and the role of TSC2 as a tumor suppressor gene. No mutations in the TSC1 gene were found. Carsillo et al. (2000) recognized that a model to account for the presence of TSC2 mutations in the renal angiomyolipoma and pulmonary LAM cells but not in other tissues was necessary. They proposed 2 potential mechanisms, either of which would represent a novel mechanism for a disease associated with tumor suppressor gene mutations. One model suggests that sporadic LAM results from somatic mosaicism for TSC2 mutations. Sporadic LAM patients could have TSC2 mutations only in selected kidney and lung cells, and not in surrounding cells within the normal kidney or lung. According to this model, one would expect multiple independent tumor foci, whereas most sporadic LAM patients have a single angiomyolipoma. The second model entertained by Carsillo et al. (2000) involves the migration or spread of smooth muscle cells from the angiomyolipoma to the lung. Angiomyolipomas are histologically benign neoplasms; however, in patients with sporadic, solitary renal angiomyolipomas, it is not unusual to find angiomyolipoma cells in perirenal lymph nodes, suggesting that these cells are capable of spreading beyond the primary tumor. This is the 'benign metastasis' hypothesis (Karbowniczek et al., 2003).
Sato et al. (2002) studied the TSC1 and TSC2 genes in 6 Japanese patients with pulmonary LAM in association with the TSC complex (TSC-LAM) and 22 patients with sporadic LAM and identified 6 novel mutations. TSC2 germline mutations were detected in 2 (33.3%) of the 6 patients with TSC-LAM, and a TSC1 germline mutation was detected in 1 (4.5%) of the 22 sporadic LAM patients. In accordance with the tumor suppressor model, LOH was detected in LAM cells from 3 of 4 patients with TSC-LAM and from 4 of 8 patients with sporadic LAM. Furthermore, an identical LOH or 2 identical somatic mutations were demonstrated in LAM cells microdissected from several tissues, suggesting that LAM cells can spread from one lesion to another. These results confirmed the prevailing concept of pathogenesis of LAM: TSC-LAM has a germline mutation, but sporadic LAM does not; sporadic LAM is a TSC2 disease with 2 somatic mutations; and a variety of TSC mutations can cause LAM. However, this study indicated that a fraction of sporadic LAM can be a TSC1 disease; therefore, both TSC genes should be examined, even in patients with sporadic LAM.