Glycogen Storage Disease Type Iv
Summary
Clinical characteristics.
The clinical manifestations of glycogen storage disease type IV (GSD IV) discussed in this entry span a continuum of different subtypes with variable ages of onset, severity, and clinical features. Clinical findings vary extensively both within and between families.
- The fatal perinatal neuromuscular subtype presents in utero with fetal akinesia deformation sequence, including decreased fetal movements, polyhydramnios, and fetal hydrops. Death usually occurs in the neonatal period.
- The congenital neuromuscular subtype presents in the newborn period with profound hypotonia, respiratory distress, and dilated cardiomyopathy. Death usually occurs in early infancy.
- Infants with the classic (progressive) hepatic subtype may appear normal at birth, but rapidly develop failure to thrive; hepatomegaly, liver dysfunction, and progressive liver cirrhosis; hypotonia; and cardiomyopathy. Without liver transplantation, death from liver failure usually occurs by age five years.
- Children with the non-progressive hepatic subtype tend to present with hepatomegaly, liver dysfunction, myopathy, and hypotonia; however, they are likely to survive without progression of the liver disease and may not show cardiac, skeletal muscle, or neurologic involvement.
- The childhood neuromuscular subtype is rare and the course is variable, ranging from onset in the second decade with a mild disease course to a more severe, progressive course resulting in death in the third decade.
Diagnosis/testing.
The diagnosis is established in a proband by the demonstration of glycogen branching enzyme (GBE) deficiency in liver, muscle, or skin fibroblasts or the identification of biallelic pathogenic variants in GBE1 on molecular genetic testing.
Management.
Treatment of manifestations: Management should involve a multidisciplinary team including specialists in hepatology, neurology, nutrition, medical or biochemical genetics, and child development. Liver transplantation is the only treatment option for individuals with the progressive hepatic subtype of GSD IV who develop liver failure; however, the risk for morbidity and mortality is high, in part because of the extrahepatic manifestations of GSD type IV, especially cardiomyopathy. Children with skeletal myopathy and/or hypotonia warrant developmental evaluation and physical therapy as needed. Those with cardiomyopathy warrant care by a cardiologist. Heart transplant may be an option in individuals with severe cardiac involvement.
Prevention of secondary complications: Prevent nutritional deficiencies (e.g., of fat-soluble vitamins) by ensuring adequate dietary intake; prevent perioperative bleeding by assessment of a coagulation profile and use of fresh frozen plasma as needed.
Surveillance: No clinical guidelines for surveillance are available. The following evaluations are suggested (with frequency varying according to disease severity): liver function tests including liver transaminases, albumin, and coagulation profile (PT and PTT); abdominal ultrasound examination; echocardiogram; neurologic assessment; nutritional assessment. If cardiomyopathy was not observed on baseline screening echocardiogram at the time of initial diagnosis, repeat echocardiograms every three months during infancy, every six months during early childhood, and annually thereafter.
Evaluation of relatives at risk: If the GBE1 pathogenic variants have been identified in an affected family member, test at-risk relatives to allow for early diagnosis and management of disease manifestations.
Genetic counseling.
GSD IV is inherited in an autosomal recessive manner. Each sib of an affected individual has a 25% chance of being affected, a 50% chance of being an asymptomatic carrier, and a 25% chance of being unaffected and not a carrier. Although affected sibs are expected to manifest the same subtype of GSD IV, the age of onset and presentation may differ. Carrier testing for at-risk family members and prenatal testing for pregnancies at increased risk are possible based on molecular testing if the pathogenic variants in the family have been identified. If the pathogenic variants have not been identified, GBE testing on cultured amniocytes can be performed for prenatal diagnosis.
Diagnosis
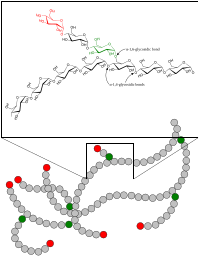
The diagnosis of glycogen storage disease type IV (GSD IV) is suspected based on the clinical presentation and the finding of abnormally branched glycogen accumulation in muscle or liver tissue. The diagnosis is confirmed by the demonstration of glycogen branching enzyme (GBE) deficiency in liver, muscle, or skin fibroblasts [Brown & Brown 1983], and/or the identification of biallelic pathogenic variants in GBE1.
Suggestive Findings
Glycogen storage disease type IV (GSD IV) should be suspected in individuals with the features below. While subtypes with variable ages of onset, severity, and clinical features have been recognized, the GSD IV phenotype represents a continuum that ranges from mild to severe [Burrow et al 2006].
Clinical features by subtype:
- Fatal perinatal neuromuscular subtype. Decreased fetal movements, polyhydramnios, and fetal hydrops that may be detected prenatally; arthrogryposis, severe hypotonia, muscle atrophy at birth, early neonatal death
- Congenital neuromuscular subtype. Profound neonatal hypotonia at birth, respiratory failure, dilated cardiomyopathy, early infantile death
- Classic (progressive) hepatic subtype. Failure to thrive, hepatomegaly, liver dysfunction, progressive liver cirrhosis with portal hypertension, ascites, and esophageal varices, hypotonia, and cardiomyopathy; death typically by age five years from liver failure
- Non-progressive hepatic subtype. Liver dysfunction, myopathy, and hypotonia in childhood
- Childhood neuromuscular subtype. Chronic, progressive myopathy; dilated cardiomyopathy in some individuals
Laboratory features
- Liver enzymes typically elevated in the hepatic subtypes
- Hypoalbuminemia
- Prolonged partial thromboplastin time (PTT) and prothrombin time (PT) with progressive deterioration of liver function
Imaging features. Abdominal ultrasound examination typically reveals enlarged liver with signs of fibrosis or cirrhosis.
Histopathology of affected tissues (e.g., liver, heart, muscle) reveals:
- Markedly enlarged hepatocytes that contain periodic acid-Schiff (PAS)-positive and diastase-resistant inclusions, features characteristic of the abnormally branched glycogen found in GSD IV. Widespread infiltrates of foamy histiocytes with intra-cytoplasmic deposits within the reticuloendothelial system (RES) have been reported [Magoulas et al 2012]. Interstitial fibrosis with wide fibrous septa and distorted hepatic architecture are observed [Moses & Parvari 2002].
- On electron microscopy, fine fibrillary aggregates of electron-dense amylopectin-like material within the cytoplasm of hepatocytes in some individuals.
Establishing the Diagnosis
The diagnosis of glycogen storage disease type IV (GSD IV) is established in a proband by the presence of the above suggestive findings AND identification of:
- Reduced glycogen branching enzyme (GBE) activity (most commonly assayed in cultured skin fibroblasts but may also be assayed in muscle or liver tissue); OR
- Biallelic pathogenic variants in GBE1 on molecular genetic testing (see Table 1).
Molecular genetic testing approaches can include a combination of gene-targeted testing (single-gene testing, multigene panel) and comprehensive genomic testing (exome sequencing, exome array, genome sequencing) depending on the phenotype.
Gene-targeted testing requires that the clinician determine which gene(s) are likely involved, whereas genomic testing does not. Because the phenotype of GSD IV is broad, individuals with the distinctive findings described in Suggestive Findings are likely to be diagnosed using gene-targeted testing (see Option 1), whereas those with a phenotype indistinguishable from many other inherited disorders with liver dysfunction and/or cardiomyopathy are more likely to be diagnosed using genomic testing (see Option 2).
Option 1
When the phenotypic and laboratory findings suggest the diagnosis of GSD IV, molecular genetic testing approaches can include single-gene testing or use of a multigene panel:
- Single-gene testing. Sequence analysis of GBE1 detects small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. Perform sequence analysis first. If only one or no pathogenic variant is found, perform gene-targeted deletion/duplication analysis to detect intragenic deletions or duplications.
- A multigene panel that includes GBE1 and other genes of interest (see Differential Diagnosis) is most likely to identify the genetic cause of the condition at the most reasonable cost while limiting identification of variants of uncertain significance and pathogenic variants in genes that do not explain the underlying phenotype. Note: (1) The genes included in the panel and the diagnostic sensitivity of the testing used for each gene vary by laboratory and are likely to change over time. (2) Some multigene panels may include genes not associated with the condition discussed in this GeneReview. (3) In some laboratories, panel options may include a custom laboratory-designed panel and/or custom phenotype-focused exome analysis that includes genes specified by the clinician. (4) Methods used in a panel may include sequence analysis, deletion/duplication analysis, and/or other non-sequencing-based tests. For this disorder a multigene panel that also includes deletion/duplication analysis is recommended (see Table 1).For an introduction to multigene panels click here. More detailed information for clinicians ordering genetic tests can be found here.
Option 2
When the phenotype is indistinguishable from many other inherited disorders characterized by liver dysfunction, comprehensive genomic testing (which does not require the clinician to determine which gene[s] are likely involved) is the best option. Exome sequencing is most commonly used; genome sequencing is also possible. In addition, many laboratories now offer rapid or critical exome sequencing, which can provide results within a shorter time frame, and thus potentially provide an earlier diagnosis and guide management or treatment decisions.
If exome sequencing is not diagnostic, exome array (when clinically available) may be considered to detect (multi)exon deletions or duplications that cannot be detected by sequence analysis.
For an introduction to comprehensive genomic testing click here. More detailed information for clinicians ordering genomic testing can be found here.
Table 1.
Molecular Genetic Testing Used in Glycogen Storage Disease Type IV
| Gene 1 | Method | Proportion of Pathogenic Variants 2 Detectable by Method |
|---|---|---|
| GBE1 | Sequence analysis 3 | 62/84 (74%) 4, 5 |
| Gene-targeted deletion/duplication analysis 6 | 8/84 (10%) 7 |
- 1.
See Table A. Genes and Databases for chromosome locus and protein.
- 2.
See Molecular Genetics for information on allelic variants detected in this gene.
- 3.
Sequence analysis detects variants that are benign, likely benign, of uncertain significance, likely pathogenic, or pathogenic. Variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. For issues to consider in interpretation of sequence analysis results, click here.
- 4.
Magoulas et al [2012]
- 5.
Of 42 affected individuals, 37 had at least one identifiable variant detected by sequencing analysis; 28 individuals had biallelic pathogenic variants, and six had one identifiable pathogenic variant, implying that the second causative variant was not identified.
- 6.
Gene-targeted deletion/duplication analysis detects intragenic deletions or duplications. Methods used may include quantitative PCR, long-range PCR, multiplex ligation-dependent probe amplification (MLPA), and a gene-targeted microarray designed to detect single-exon deletions or duplications.
- 7.
Of the 42 affected individuals, three were homozygous for exon or multiexon deletions and two were compound heterozygous for one exon or multiexon deletion and one sequence variant detectable by sequence analysis [Li et al 2012, Magoulas et al 2012].
Clinical Characteristics
Clinical Description
The clinical manifestations of glycogen storage disease type IV (GSD IV) span a continuum from mild to severe [Burrow et al 2006]. Within this continuum several different subtypes with variable age of onset, severity, and clinical features have been recognized. While prognosis tends to depend on the subtype of GSD IV, clinical findings vary extensively both within and between families.
The fatal perinatal neuromuscular subtype, the most severe subtype, presents in utero with fetal akinesia deformation sequence, including decreased fetal movements, polyhydramnios, and fetal hydrops. Newborns may have arthrogryposis, severe hypotonia, and muscular atrophy, often resembling infants with the severe forms of spinal muscular atrophy [Tay et al 2004]. Death usually occurs in the neonatal period, frequently as a result of cardiopulmonary compromise.
The congenital neuromuscular subtype presents in the newborn period with profound hypotonia, respiratory distress, dilated cardiomyopathy, and death in early infancy typically from cardiopulmonary compromise [Moses & Parvari 2002]. Li et al [2012] recently reported two unrelated infants with this subtype of GSD IV who were also small for gestational age. Both died between ages two and three months.
The hepatic subtype, the most common presentation of GSD IV, can be classified as either progressive (classic) or non-progressive.
- In the progressive hepatic subtype, children may appear normal at birth, but then rapidly deteriorate in the first few months of life with failure to thrive, hepatomegaly, and elevated liver enzymes. This stage is typically followed by progressive liver dysfunction and cirrhosis with hypoalbuminemia, prolonged partial thromboplastin time (PTT) and prothrombin time (PT), portal hypertension, ascites, and esophageal varices. Muscle tone, often normal at the time of diagnosis, progresses to generalized hypotonia within the first one to two years of life [Magoulas et al 2012]. Without liver transplantation, death from liver failure usually occurs by age five years [Chen 2001, Moses & Parvari 2002]. Dilated cardiomyopathy and progressive cardiac failure, reported to occur following orthotopic liver transplantation, have resulted in death [Sokal et al 1992, Rosenthal et al 1995].
- In the less common non-progressive hepatic subtype, presentation can be in childhood with hepatomegaly, liver dysfunction, myopathy, and hypotonia. These individuals tend to survive without evidence of progression of the liver disease [Moses & Parvari 2002]. They also may not show cardiac, skeletal muscle, or neurologic involvement. Liver enzymes are usually abnormal in childhood at the time of presentation, but subsequently may return to (and remain) normal [McConkie-Rosell et al 1996].
The childhood neuromuscular subtype of GSD IV is rare [Reusche et al 1992, Schröder et al 1993]. Individuals typically present in the second decade and may have mild-to-severe myopathy and dilated cardiomyopathy. The natural history is variable: some individuals have a mild disease course throughout life while others have a more severe, progressive course resulting in death in the third decade.
Genotype-Phenotype Correlations
Genotype-phenotype correlations remain unclear, but are emerging [Ziemssen et al 2000, Magoulas et al 2012].
- Individuals with the perinatal and congenital subtypes tend to have two null variants, including nonsense, frameshift, and splice site variants leading to premature truncation of the protein likely resulting in complete absence of glycogen branching enzyme (GBE) activity;
- Individuals with the classic hepatic subtype tend to be compound heterozygotes for a null and a missense variant.
These generalizations notwithstanding, considerable overlap exists both between and within the subtypes of GSD IV [Li et al 2010].
Nomenclature
Glycogen storage disease type IV was referred to as glycogenosis IV in early publications.
Prevalence
Glycogen storage disease type IV is rare, accounting for approximately 3% of the glycogen storage diseases [Chen 2001] for an overall incidence of approximately 1:600,000-1:800,000.
To date, more than 50 individuals with molecularly confirmed GSD IV have been reported [Fernandez et al 2010, Li et al 2010, Li et al 2012, Magoulas et al 2012, Mochel et al 2012, Ravenscroft et al 2013, Paradas at al 2014, Akman et al 2015, Sampaolo et al 2015, Bendroth-Asmussen et al 2016, Dainese et al 2016, Franco-Palacios et al 2016, Said et al 2016, Iijima et al 2018].
Differential Diagnosis
Perinatal and Congenital Neuromuscular Subtypes of GSD IV
The differential diagnosis of the perinatal and congenital neuromuscular subtypes of GSD IV includes the disorders summarized in Table 2a.
Table 2a.
Other Genes of Interest in the Differential Diagnosis of Perinatal and Congenital Neuromuscular Subtypes of GSD IV
| Gene(s) | Differential Diagnosis Disorder | MOI | Features of Differential Diagnosis Disorder | |
|---|---|---|---|---|
| Overlapping w/perinatal & congenital neuromuscular subtypes of GSD IV | Distinguishing from perinatal & congenital neuromuscular subtypes of GSD IV | |||
| SMN1 | Spinal muscular atrophy | AR |
|
|
| GAA | Pompe disease | AR |
| Hypertrophic cardiomyopathy rather than dilated cardiomyopathy |
| >10 genes 1 | Zellweger spectrum disorder | AR |
| Rhizomelic chondrodysplasia punctata & biochemical peroxisomal abnormalities |
| >40 genes 2 | Congenital disorders of glycosylation | AR (XL) |
|
|
AR = autosomal recessive; GSD = glycogen storage disease; MOI = mode of inheritance; XL = X-linked
- 1.
See Zellweger spectrum disorder.
- 2.
See OMIM Phenotypic Series: Congenital disorders of glycosylation, type I and Congenital disorders of glycosylation, type II.
Classic Hepatic Subtype of GSD IV
The differential diagnosis of the classic hepatic subtype of GSD IV includes other glycogen storage disorders and mitochondrial DNA depletion syndromes. Examples of these categories of disorders are described in Table 2b.
Table 2b.
Other Genes of Interest in the Differential Diagnosis of the Classic Hepatic Subtype of GSD IV
| Gene | Differential Diagnosis Disorder | MOI | Features of Differential Diagnosis Disorder | |
|---|---|---|---|---|
| Overlapping w/classic hepatic subtype of GSD IV | Distinguishing from classic hepatic subtype of GSD IV | |||
| AGL | GSD III | AR |
|
|
| DGUOK | Deoxyguanosine kinase deficiency | AR |
|
|
| MPV17 | MPV17-related mtDNA maintenance defect | AR |
|
|
AR = autosomal recessive; GSD = glycogen storage disease; MOI = mode of inheritance; mtDNA = mitochondrial DNA
Childhood Neuromuscular Subtype of GSD IV
The differential diagnosis of the childhood neuromuscular subtype of GSD IV includes mitochondrial myopathies and the disorders summarized in Table 2c.
Table 2c.
Other Genes of Interest in the Differential Diagnosis of the Childhood Neuromuscular Subtype of GSD IV
| Gene(s) | Differential Diagnosis Disorder | MOI | Features of Differential Diagnosis Disorder | |
|---|---|---|---|---|
| Overlapping w/childhood neuromuscular subtype of GSD IV | Distinguishing from childhood neuromuscular subtype of GSD IV | |||
| DMD | Duchenne muscular dystrophy | XL |
|
|
| >30 genes 1 | Limb-girdle muscular dystrophy | AR AD |
| Winged scapula |
| Mitochondrial DNA | Mitochondrial myopathies (Kearns-Sayre, MERRF) | Mat |
|
|
AD = autosomal dominant; AR = autosomal recessive; GSD = glycogen storage disease; Mat = maternal; MOI = mode of inheritance; XL = X-linked
- 1.
See Chu & Moran [2018] and OMIM Phenotypic Series: Muscular dystrophy, limb-girdle, autosomal recessive and Muscular dystrophy, limb-girdle, autosomal dominant.
Management
Evaluations Following Initial Diagnosis
To establish the extent of disease and needs in an individual diagnosed with glycogen storage disease type IV (GSD IV), the evaluations summarized in Table 3 (if not performed as part of the evaluation that led to the diagnosis) are recommended.
Table 3.
Recommended Evaluations Following Initial Diagnosis in Individuals with Glycogen Storage Disease Type IV
| System/Concern | Evaluation | Comment |
|---|---|---|
| Hepatic | Liver function studies incl albumin, transaminases, & coagulation profile | |
| Cardiac | Referral to cardiologist for baseline echocardiogram & electrocardiogram | To assess for cardiomyopathy |
| Development | Neurodevelopmental evaluation | |
| Neurologic | Referral to neurologist for comprehensive examination & baseline assessment of skeletal muscle involvement | To monitor disease progression |
| Other | Consultation w/clinical geneticist &/or genetic counselor |
Treatment of Manifestations
Management should involve a multidisciplinary team including specialists in hepatology, neurology, nutrition, medical or biochemical genetics, and child development.
Hepatic Manifestations
Liver transplantation is the only treatment option for individuals with the progressive hepatic subtype of GSD IV who develop liver failure. Of the 20 individuals with GSD IV who have received a liver transplant to date, two required a second liver transplant and six died: four from sepsis, one from hepatic artery thrombosis, and one from cardiomyopathy. The prognosis in persons with GSD IV who undergo liver transplantation is poor because of the significant risk for morbidity and mortality, which is in part attributed to the extrahepatic manifestations of GSD type IV, especially cardiomyopathy [Davis & Weinstein 2008, Magoulas et al 2012, Troisi et al 2014, Choi et al 2018].
Selecting appropriate candidates for liver transplantation can be complex. Histologic, molecular, or clinical predictors of disease progression are likely to be useful in stratifying patients prior to liver transplantation [Davis & Weinstein 2008]. Factors such as glycogen branching enzyme (GBE) activity may not be the best predictor of outcome since the level of GBE activity in different tissues can vary by disease subtype and severity.
Neurologic Manifestations
Children with skeletal myopathy and/or hypotonia who experience motor developmental delay warrant developmental evaluation and physical therapy as needed.
Cardiac Manifestations
For those with cardiomyopathy, care by a cardiologist is warranted. Individuals with severe cardiomyopathy secondary to glycogenosis may be candidates for cardiac transplantation [Ewert et al 1999]; however, consideration of potential contraindications to cardiac transplantation, including myopathy, liver failure, and cachexia, is essential before pursuing this treatment option.
Prevention of Secondary Complications
Nutritional deficiencies (e.g., of fat-soluble vitamins) can be prevented by ensuring adequate dietary intake based on frequent assessments by and recommendations of a dietitian experienced in managing children with liver disease.
Bleeding due to coagulopathy can occur especially with surgical procedures; therefore, it is recommended that a coagulation profile be assessed before surgical procedures and fresh frozen plasma be given preoperatively as needed.
Surveillance
No clinical guidelines for surveillance are available.
Table 4.
Recommended Surveillance for Individuals with Glycogen Storage Disease Type IV
| System/Concern | Evaluation | Frequency |
|---|---|---|
| Hepatic |
| Frequency according to severity |
| Cardiac | Echocardiogram | If cardiomyopathy was not seen on echocardiogram at diagnosis, repeat echocardiogram every 3 mos in infancy, every 6 mos in early childhood, & annually thereafter. |
| Neurologic | Neurologic assessment | Frequency according to severity |
| Gastrointestinal |