Johanson-Blizzard Syndrome
A number sign (#) is used with this entry because of evidence that Johanson-Blizzard syndrome (JBS) is caused by homozygous or compound heterozygous mutation in the UBR1 gene (605981) on chromosome 15q15.
DescriptionJohanson-Blizzard syndrome is an autosomal recessive disorder characterized by poor growth, mental retardation, and variable dysmorphic features, including aplasia or hypoplasia of the nasal alae, abnormal hair patterns or scalp defects, and oligodontia. Other features include hypothyroidism, sensorineural hearing loss, imperforate anus, and pancreatic exocrine insufficiency (summary by Al-Dosari et al., 2008).
Clinical FeaturesJohanson and Blizzard (1971) and Park et al. (1972) described this syndrome in 3 unrelated girls; features included aplasia or hypoplasia of the nasal alae, congenital deafness, hypothyroidism, postnatal growth retardation, malabsorption, mental retardation, midline ectodermal scalp defects, and absent permanent teeth. Park et al. (1972) described urogenital abnormalities, including double vagina and double uterus.
The male proband of Mardini et al. (1978) had aplasia of the alae nasi, scalp defects over the anterior and posterior fontanels, and imperforate anus. Affected brothers were reported by Day and Israel (1978). Flatz et al. (1979) described this disorder in 2 sisters. Daentl et al. (1979) reported a case in a male who died at the age of 8 years from complications of pancreatic exocrine insufficiency. Autopsy showed a small thyroid filled with colloid, almost complete replacement of the pancreas with fat, and abnormal gyral formation and cortical neuronal organization in the brain.
Motohashi et al. (1981) reported 2 families; in 1, 2 children (earlier reported by Day and Israel, 1978) were affected and in the second, in addition to the 13-month-old proband, 2 affected sibs had died perinatally. Moeschler and Lubinsky (1985) described affected brother and sister. Reichart et al. (1979) and Helin and Jodal (1981) also reported affected sibs. Normal or near-normal intelligence often seems the case.
In a review of JBS by Hurst and Baraitser (1989), it was indicated that 11 of 22 reported children had anorectal abnormalities, most often imperforate anus. Gould et al. (1989) described a family with 2 affected sibs and possibly a third who had died shortly after birth. One of the 2 sibs reported in detail (surprisingly, the sex was not given) died 3 days after birth, colostomy having been performed at age 36 hours for imperforate anus. Autopsy showed, in addition to hypoplasia of alae nasi and frontal and occipital scalp defects, pancreatic ducts and islets surrounded by connective tissue and a total absence of acini. Morphologic changes suggested dysplasia leading to developmental failure, although early acinar destruction could not be ruled out. The second sib, a male born 3 years later, also had the same facies and imperforate anus which was successfully treated surgically. He was treated for pancreatic insufficiency and hypothyroidism, and at age of 10 years performed satisfactorily in a school for the hearing impaired. In the case of the autopsied sib, the thyroid was grossly and microscopically normal with abundant scalloping of colloid.
Gershoni-Baruch et al. (1990) described 2 patients with JBS. They stated that the patients reported as cases of trypsinogen deficiency (see 614044) by Morris and Fisher (1967) and Townes (1969) had in fact JBS, as did a patient with the XXY Klinefelter syndrome reported by Grand et al. (1966), and 2 sibs with hypoplasia of the exocrine pancreas, 1 of whom had imperforate anus, reported by Lumb and Beautyman (1952). In all, they found 26 previously reported patients. They stated that imperforate anus had been reported in 9 patients with JBS; 6 were females and 4 had rectovaginal fistula.
Nagashima et al. (1993) described diabetes mellitus, first detected at age 11 years, in a girl with Johanson-Blizzard syndrome.
Vanlieferinghen et al. (2001) described a case of Johanson-Blizzard syndrome in a neonate. Clinical features included intrauterine growth retardation, aplasia of the nasal alae, midline scalp defect, total situs inversus, imperforate anus, malrotation of the small intestine, pancreatic insufficiency, deafness, and lethal congenital heart defects with dextrocardia. The features were confirmed at autopsy. Vanlieferinghen et al. (2003) described the prenatal ultrasonographic diagnosis of a recurrence of Johanson-Blizzard syndrome in a subsequent pregnancy in this family. The pregnancy was terminated at 21 weeks' gestation. The colon was dilated at 13 weeks. At 17 weeks, dilatation of the bowel was increased, the nose was very small, and the nasal alae were not visualized. Examination of the fetus showed a small beaked nose, midline occipital scalp defect, and monstrous abdominal distention with imperforate anus. Autopsy showed anorectal atresia with sigmoidovesical fistula. Bilateral ureteral dilatation with hydronephrosis and polycystic dysplasia of the kidneys were also present.
Elting et al. (2008) reported 2 unrelated girls with a mild form of Johanson-Blizzard syndrome, born of Turkish and Iranian consanguineous parents, respectively. In addition to the mild but classic features of the disorder, 1 girl had dilated cardiomyopathy, whereas the other had a small atrial septal defect. Neither had significant mental impairment. Molecular genetic analysis revealed that both girls had the same homozygous mutation in the UBR1 gene (605981.0004).
Al-Dosari et al. (2008) reported a male infant, born of consanguineous Saudi Arabian parents, with JBS. He showed intrauterine growth retardation and was noted to have imperforate anus, aplasia of the alae nasi, long philtrum, downturned mouth corners, upslanting palpebral fissures, and an unusual hair pattern on the scalp. He also had hypothyroidism, 2 cafe-au-lait spots, sensorineural hearing loss, and hepatomegaly with hyperbilirubinemia and elevated liver enzymes. Liver biopsy showed giant cell hepatocytes, cholestasis, and decreased number of bile ducts. The liver disease progressed to advanced fibrosis with portal hypertension. The patient did not have pancreatic insufficiency. Family history revealed 3 prior abortions in the mother. Al-Dosari et al. (2008) noted that liver involvement had not previously been reported in this disorder, but could not rule out that it was unrelated. However, genetic analysis excluded a mutation in the MRD3 gene (ABCB4; 171060) as a cause of the liver failure. Liver sections from Ubr1-null mice did not differ from those of wildtype mice.
InheritanceThe possibility of X-linked dominance lethal in the male was raised by Konigsmark and Gorlin (1976) since most patients had been female and the syndrome may have been observed in an XXY male. Autosomal recessive inheritance appeared to have been clinched, however, by the inbred Saudi Arabian pedigree with 3 affected members (1 male and 2 females) reported by Mardini et al. (1978). Parental consanguinity was reported also by Schussheim et al. (1976).
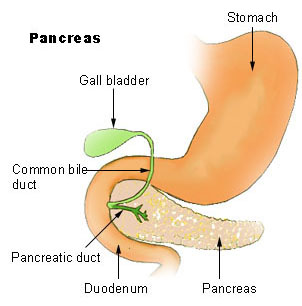
PathogenesisUsing antibody to UBR1 (605981) and either immunofluorescence microscopy with pancreatic tissue sections or immunoblotting with extracts from cells in culture, Zenker et al. (2005) observed no UBR1 protein in individuals with JBS from different families. By contrast, UBR1 was readily detectable in control pancreas, where it was present largely in the cytosol of acinar cells. Control immunostaining for trypsinogen (276000) as a specific marker for acinar cells showed no substantial differences between pancreas from controls and individuals with JBS, indicating that there was no primary defect of zymogen synthesis in JBS.
Zenker et al. (2005) examined the pancreatic pathology and cell biology in autopsy specimens from 2 fetuses (21 and 34 weeks' gestation, respectively) and also in a newborn baby with JBS. The pancreas of individuals with JBS showed acinar tissue loss that increased with gestational age and was accompanied by inflammatory infiltrates, most prominent in the near-term fetus. Using the TUNEL assay for apoptotic cells, they found no evidence of increased apoptosis in acinar cells of individuals with JBS. Taken together, these findings suggested that the main pancreatic defect in individuals with JBS is not perturbed acinar development in early embryogenesis, but rather gradual destruction of previously formed acinar cells in maturing fetuses, a process that resembles pancreatitis of intrauterine onset.
MappingTo identify the locus mutated in JBS, Zenker et al. (2005) performed a genomewide linkage scan using a panel of microsatellite markers with an average distance of 10 cM in 7 kindreds with the disorder. They identified a region of homozygosity on 15q shared by individuals originating from all consanguineous families. They further analyzed this region by typing additional microsatellite markers from the draft human genome sequence and refined the candidate region to a 7.5-cM interval. The maximum 2-point lod score was 4.8 for theta = 0.0 at D15S968.
Molecular GeneticsZenker et al. (2005) prioritized genes within the JBS candidate region on chromosome 15q for mutational screening on the basis of putative function and expression data but identified no obvious candidate. By high-throughput sequencing of DNA from individuals with JBS, they eventually detected mutations in the UBR1 gene (e.g., 605981.0001-605981.0003). In affected individuals from 12 of 13 families included in the study, the variations likely to be causal mutations were identified in both alleles of UBR1, whereas in 1 family, only the paternally inherited mutation was found. Most disease-associated UBR1 alleles (12 of 14) were mutations that predicted premature translational stop codons. Two missense mutations in UBR1 caused substitutions of residues that are conserved among UBR1 proteins of different species.
In a male infant with JBS, who was born of consanguineous Saudi Arabian parents, Al-Dosari et al. (2008) identified a homozygous splice site mutation in the UBR1 gene (605981.0005).
HistoryTownes (1969) reported a 3.5-year-old female with generalized anasarca, hypoproteinemia, and congestive heart failure. A combined proteolytic and lipolytic defect was found. Activities of trypsin, chymotrypsin, carboxypeptidase, and lipase were completely absent. Activation studies proved negative. Striking improvement accompanied feeding of protein hydrolysate (Townes, 1972). The child also had an imperforate anus, a point of interest because a patient with trypsinogen deficiency also had imperforate anus.