Primary Sclerosing Cholangitis
Primary sclerosing cholangitis (PSC) is a rare, slowly progressive liver disease characterized by inflammation and destruction of the intra- and/or extra-hepatic bile ducts that lead to cholestasis, liver fibrosis, liver cirrhosis and ultimately liver failure.
Epidemiology
The prevalence of PSC in Europe ranges from 1/446,000-1/6,170. A male preponderance is observed with a male to female ratio of approximately 2:1.
Clinical description
PSC can occur at any age with a peak incidence around 40 years of age. Symptoms and clinical findings are variable, depending on the stage of the disease. In early stages, unspecific manifestations such as fever, fatigue, pruritus, malaise, abdominal pain, and weight loss are reported, however about 40-50% of patients may be asymptomatic at time of diagnosis. Hepatomegaly, splenomegaly, jaundice, portal hypertension and, in more advanced cases, spider angiomata, ascites and muscle atrophy are observed. The disease course is also highly variable, but in the majority of cases, PSC is slowly progressive, leading to liver cirrhosis, liver failure and the need for liver transplantation over a period of 13-21 years following diagnosis. Several immune-mediated comorbidities are observed in PSC. The most common co-existing condition is inflammatory bowel disease, reported in up to 60-80% of patients of Northern European decent. Other immune-mediated conditions, such as autoimmune hepatitis, thyroid disease, type 1 diabetes mellitus, and celiac disease, are also observed with slightly increased frequencies in PSC patients. A proportion of PSC patients develop malignancies; mainly cholangiocarcinoma, but also increased risk of carcinoma of the large intestine in patients with concomitant IBD. Small-duct PSC is a PSC-variant manifesting with chronic cholestasis, biochemical and histological findings similar to those found in PSC, and a normal cholangiography.
Etiology
The precise etiology of PSC has not yet been established, but it is believed to be multifactorial. Genetic susceptibility factors are known to be involved, and a strong association to genetic variants within the HLA-region on chromosome 6 is observed. The disease is thought to be related to an abnormal immune response to a still unidentified environmental stimulus.
Diagnostic methods
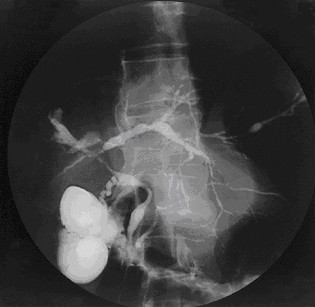
PSC is suspected based on clinical manifestations and altered liver function tests and diagnosis is confirmed through magnetic resonance cholangiopancreatography (MRCP) or endoscopic retrograde cholangiopancreatography (ERCP) showing bile duct changes with strictures and dilatations characteristic of the disease.
Differential diagnosis
Differential diagnoses include other hepatic diseases, such as autoimmune hepatitis and primary biliary cholangitis. Exclusion of multiple secondary causes leading to PSC-like bile duct changes, such as IgG4-associated sclerosing cholangitis, mast cell cholangiopathy, infections, biliary calculi or trauma, and other identifiable causes of insults to the biliary tree (leading to the ERCP or MRCP features seen in PSC) is mandatory to establish the diagnosis of PSC.
Management and treatment
Immunosuppressants and chelators are used to treat the symptoms and manage the complications, however, to date there are no medical therapies that cure or alter the disease course of PSC. Replacement therapy of fat-soluble vitamins A, D, E, and K is frequently necessary since patients frequently present deficiency of these vitamins. Liver transplantation is currently the only definitive treatment for patients with advanced disease and the majority of patients require a liver transplantation 13-21 years after diagnosis; either due to disease progression or disease complications, such as treatment-resistant bacterial cholangitis. Endoscopic dilatation, with or without stenting, of biliary strictures may be performed to relieve symptoms of biliary obstruction.
Prognosis
Prognosis after liver transplantation is generally good, however, in a proportion of patients PSC may recur in the transplanted liver, with recurrence rates varying from 10-37%.