Isolated Oxycephaly
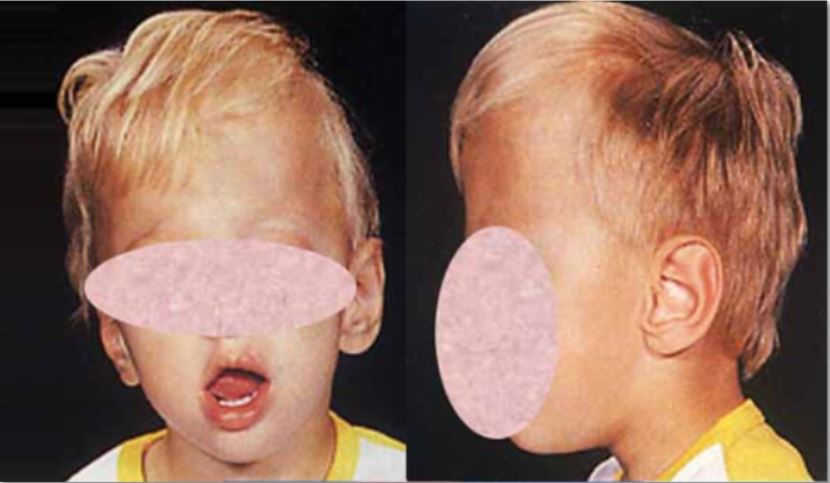
Isolated oxycephaly is a late-appearing form of nonsyndromic craniosynostosis characterized by premature fusion of both the coronal and sagittal sutures, and, in some cases, of the lambdoid sutures. Compensatory growth in the region of the anterior fontanel results in a pointed or cone-shaped skull.
Epidemiology
Prevalence is unknown.
Clinical description
The mean age at diagnosis is around six years. Elevated intracranial pressure is a common clinical feature (affecting more than 60% of the patients) leading to frequent ophthalmologic complications (papilledema) and moderate to severe intellectual deficit. Chiari type I malformation is commonly seen on MRI scans.
Etiology
Etiology is unknown.
Diagnostic methods
Diagnosis is based on clinical examination, X-rays and 3D CT scans of the skull. MRI exploration of the Chiari type I malformation and ophthalmologic examinations are also required for diagnosis.
Differential diagnosis
Oxycephaly may also be a feature of certain syndromes (Crouzon syndrome and Pfeiffer syndrome; see these terms). The syndromic and nonsyndromic forms can be distinguished by the absence of limb and/or facial anomalies in nonsyndromic forms.
Genetic counseling
Isolated oxycephaly is usually sporadic but familial cases have been reported.
Management and treatment
Cranial expansion surgery (fronto-orbital advancement) is essential for relieving intracranial pressure and stabilizing intellectual level. It should be performed during childhood, as soon as the clinical diagnosis has been established. In the absence of appropriate treatment, the intellectual deficit becomes significantly more profound. Papilledema, which is a consequence of increased intracranial pressure, usually disappears postoperatively. Following surgery, the intracranial pressure returns to normal and the intellectual deficit seems to stabilize in most cases. However, secondary surgery is more commonly required in oxycephaly patients than in those with single suture craniosynostosis.