Rolandic Epilepsy
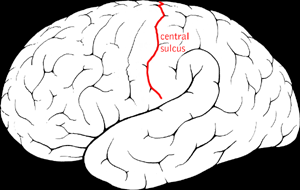
Rolandic epilepsy (RE) is a focal childhood epilepsy characterized by seizures consisting of unilateral facial sensory-motor symptoms, with electroencephalogram (EEG) showing sharp biphasic waves over the rolandic region. It is an age-related epilepsy, with excellent outcome.
Epidemiology
RE is the most common childhood epilepsy and accounts for 8-25% of all childhood epilepsies. Its incidence has been estimated to be approximately 1/5,000 in children within 15 years.
Clinical description
Onset is between 3 and 12 years, in otherwise normal children (peak of onset is 5-8 years). Seizures typically occur during sleep or drowsy states; they are brief with unilateral sensorimotor (such as numbness, tingling, drooling) that involves pharynx, tongue, face, lips and sometimes hand. Speech arrest often occurs, while comprehension is preserved. Seizures may alternate from one side to the other and may become generalized. Longer attacks can be followed by post-ictal hemiplegia. Some children may have selective neuropsychological impairment affecting language, attention, visuomotor skills and behavior. They usually do not outlast the period of active seizures. Seizure remission occurs within 2-4 years from the onset. The majority of patients have <10 seizures and 10-20% have a single seizure.
Etiology
Etiology of RE is still unknown. There is probably a genetic predisposition: an increased rate of RE, febrile seizures, and epilepsy-aphasia spectrum disorders were found among relatives. Pathogenesis seems to be related with the critical and vulnerable phase of brain maturation.
Diagnostic methods
Diagnosis of RE relies on the clinical features and on EEG findings that show slow, diphasic, high voltage, centrotemporal spikes, activated by sleep. Brain magnetic resonance imaging (MRI) is normal.
Differential diagnosis
Differential diagnosis includes other idiopathic focal childhood epilepsies (benign childhood occipital epilepsy, Panayiotopoulos type and Gastaut type. Other etiologies causing similar symptoms are excluded with brain MRI.
Genetic counseling
Autosomal dominant transmission has been reported in some cases.
Management and treatment
The majority of patients, who have a single or few seizures, do not require treatment. Differently, patients with frequent seizures (10-20%) may need treatment for a short time. In such cases, carbamazepine or valproate are preferred even if, in rare cases, carbamazepine may have a paradoxical effect.
Prognosis
Prognosis of RE is favorable since nearly 90% of patients remit before puberty. In rare cases (<1%), RE may evolve to atypical RE with linguistic, behavioral and neuropsychological deficits. An aggressive treatment with steroids, in these cases might change the evolution of the disease and a remission of neuropsychological deficits might be seen.