Protoporphyria, Erythropoietic, 1
A number sign (#) is used with this entry because erythropoietic protoporphyria-1 (EPP1) is caused by compound heterozygous or homozygous mutation in the gene encoding ferrochelatase (FECH; 612386) on chromosome 18q21. The disorder most often results from inheritance of a null FECH allele in trans with a low-expression FECH mutation (612386.0015) prevalent in some populations, resembling autosomal dominant inheritance with incomplete penetrance.
DescriptionErythropoietic protoporphyria-1 is an inborn error of porphyrin metabolism caused by decreased activity of the enzyme ferrochelatase, the terminal enzyme of the heme biosynthetic pathway, which catalyzes the insertion of iron into protoporphyrin to form heme. EPP is characterized clinically by photosensitivity to visible light commencing in childhood, and biochemically by elevated red cell protoporphyrin levels (Todd, 1994).
Genetic Heterogeneity of Erythropoietic Protoporphyria
Also see X-linked erythropoietic protoporphyria (XLEPP; 300752), caused by mutation in the ALAS2 gene (301300) on chromosome Xp11, and EPP2 (618015), caused by mutation in the CLPX gene (615611) on chromosome 15q22.
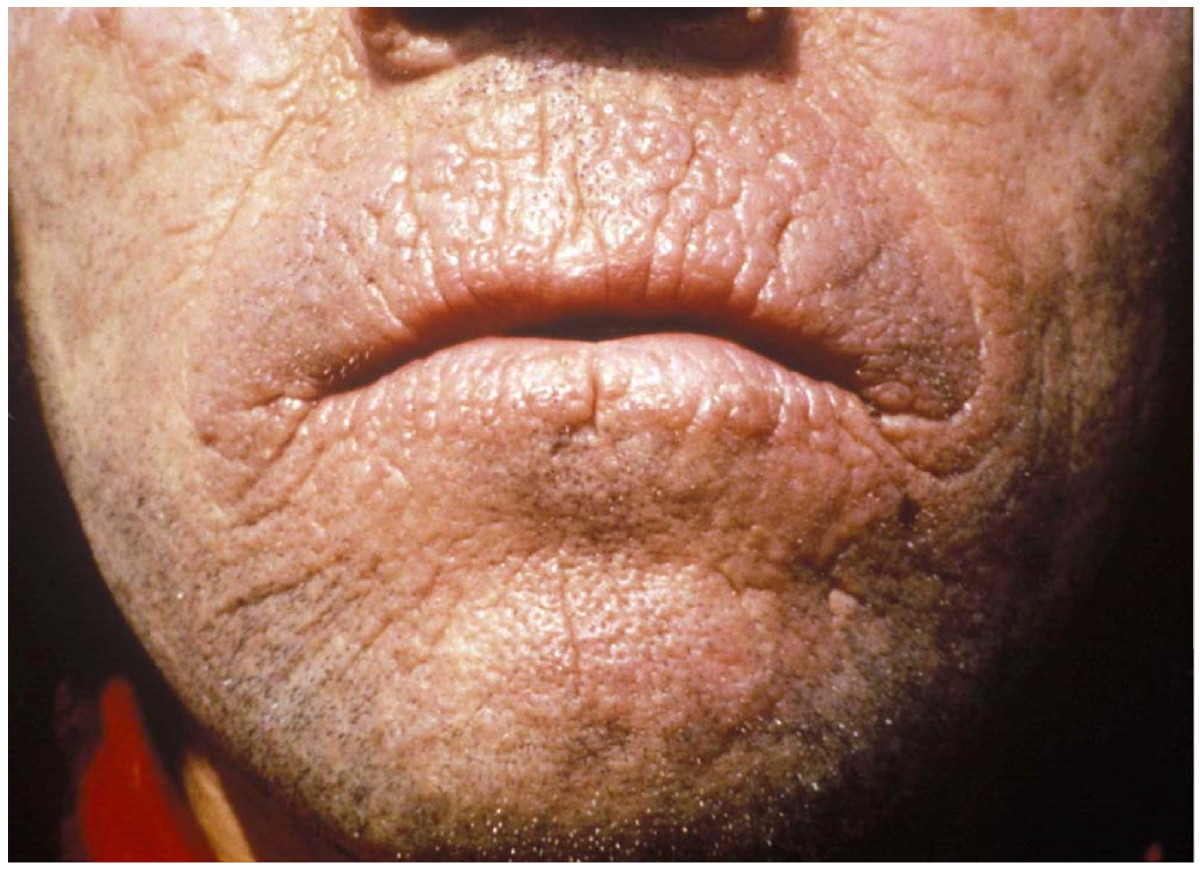
Clinical FeaturesLight-sensitive dermatitis commencing in childhood, usually before 10 years of age, is the presenting finding in erythropoietic protoporphyria (Peterka et al., 1965; DeLeo et al., 1976). Patients experience itching and burning, and develop erythema even after brief exposure to bright light. Chronic skin changes sometimes occur (Poh-Fitzpatrick, 1978). Herbert et al. (1991) described a second-degree burn of the light-exposed abdominal wall resulting from exposure during liver transplantation. The patient also had severe polyneuropathy with quadriparesis. Although most cases of EPP present in childhood, Henderson et al. (1995) reported a patient who presented at the age of 33 years and cited even older ages at presentation, namely 62 years (Fallon et al., 1989) and 69 years (Murphy et al., 1985).
Whereas most EPP patients experience only a painful photosensitivity, a small number develop liver complications, including fatal liver damage, due to the accumulation of excessive amounts of protoporphyrin in the liver (Bloomer et al., 1975; Cripps et al., 1977; Bloomer, 1979). Gallstones pigmented with protoporphyrin have been reported. Both of the British patients of Magnus et al. (1961) and one of the patients of Haeger-Aronsen (1963) were operated on for gallstones at a relatively young age.
Biochemical FeaturesThe essential biochemical abnormality in EPP is overproduction of protoporphyrin, as recognized in the original description by Magnus et al. (1961). The normal level of free erythrocyte protoporphyrin (FEP), of up to about 60 microg/dl red cells, may be increased in manifest cases to over 1,000 microg/dl. Fluorescence of a large proportion of red blood cells can also be observed by ultraviolet microscopy even when FEP is little or not increased. The excess porphyrin comes from both erythropoietic and hepatic tissue (Scholnick et al., 1971), leading to the suggestion of an alternative name, erythrohepatic porphyria.
Reduction in activity of ferrochelatase to 10 to 25% of normal levels has been demonstrated (Bonkowsky et al., 1975; Bloomer, 1980). This is unlike the dominantly inherited forms of porphyria (121300, 176000, 176100, 176200) in which 50% reduction of activity of the specific enzyme is observed (Romeo, 1977; Meyer and Schmid, 1978).
Went and Klasen (1984) found that the average hemoglobin concentration in EPP patients was 1.5 g/100 ml below that for their age- and sex-matched relatives.
PathogenesisOhgari et al. (2005) coexpressed human ferrochelatase carrying His- and HA-tags in a tandem fashion in Escherichia coli and found that ferrochelatase formed a homodimer. Homodimers of missense-mutated enzyme were produced in small amounts and showed very low activity. Heterodimers with wildtype and missense-mutated enzyme had reduced, but significant, enzymatic activity without a marked change of Km values for substrates. Heat treatment led to a rapid inactivation of the heterodimeric mutants, indicating instability. Ohgari et al. (2005) hypothesized that instability of the heterodimer containing normal and mutated ferrochelatase, as well as the low production levels due to the structural defect of the mutant protein, causes the weak enzymatic activity of ferrochelatase in EPP patients.
Clinical ManagementManagement includes avoidance of sunlight; skin protection by parenteral administration of beta-carotene has given equivocal results (Mathews-Roth et al., 1970; Corbett et al., 1977; Poh-Fitzpatrick, 1978). Liver disease may be ameliorated by treatment with cholestyramine (Bloomer, 1979).
In 5 patients with erythropoietic protoporphyria, Harms et al. (2009) reported favorable results after treatment with afamelanotide, an alpha-melanocyte-stimulating hormone (see 176830) analog that induces epidermal melanin formation. Both tolerance to artificial light and melanin density increased significantly after 120 days.
The hypomorphic C allele of FECH uses a cryptic intron 3 acceptor site and results in reduction of FECH activity; when the C allele occurs with a severe FECH mutation on the other allele, overall FECH activity falls below a critical threshold and EPP results. Oustric et al. (2014) identified a sequence that, when targeted by an antisense oligonucleotide, prevented usage of the cryptic splice site between exons 3 and 4, resulting in the transcription of an unstable mRNA. In lymphoblastoid cell lines derived from symptomatic EPP subjects, transfection of this antisense oligonucleotide reduced the usage of the cryptic splice site and efficiently redirected the splicing of intron 3 toward the physiologic acceptor site, thereby increasing the amount of functional FECH mRNA. Oustric et al. (2014) found that administering the antisense oligonucleotide into developing human erythroblasts from an overtly EPP subject markedly increased production of wildtype FECH mRNA and reduced the accumulation of protoporphyrin IX (PPIX) to a level similar to that measured in asymptomatic EPP subjects.
InheritanceEPP can be caused by compound heterozygous or homozygous mutation in the FECH gene, and is most often caused by coinheritance of a mutation in the FECH gene in trans with a low-expression IVS3-48C mutation that is prevalent in some populations (Herrero et al., 2007).
Early studies indicated autosomal dominant inheritance of EPP, but noted that some persons who are obligatory carriers and have lifelong elevation of protoporphyrin levels may never develop photosensitivity (Donaldson et al., 1967; Reed et al., 1970; Hovding et al., 1971). Three generations were affected in the family studied by Lynch and Miedler (1965). Haeger-Aronsen (1963) found 5 cases in 3 generations of a Swedish family. In an exhaustive study in the Netherlands, Went and Klasen (1984) discovered 200 patients in 91 families. In 46 of these families, only a single patient was discovered. The presence of an occasional fluorescent red blood cell combined with normal protoporphyrin levels was observed in half of the children and sibs of patients and in 1 of their parents. Thus, this trait appeared to be autosomal recessive. However, the segregation ratio in sibships with at least 1 patient with EPP was 22.2% or 29.6%, depending on the type of correction made for bias of ascertainment; consequently, Went and Klasen (1984) concluded that EPP is a recessive. Deybach et al. (1986) observed a homozygote for erythropoietic protoporphyria.
Norris et al. (1990) likewise suggested that the inheritance is not that of a simple autosomal dominant and that inheritance of more than one gene may be required for disease expression.
Gouya et al. (1996) contributed to the understanding of the unusual inheritance in EPP. They identified a deletion of exon 10 (612386.0008) in a proband with a classic presentation and in his clinically asymptomatic brother and father. The proband had a history of skin photosensitivity without liver failure and 25% residual enzyme activity in lymphocytes. The asymptomatic brother and father had 50% enzyme activity. The mother was clinically normal and her enzyme activity was within the low normal range (79% of control activity). Using an intragenic dimorphism, 1520C/T, Gouya et al. (1996) showed that the mother was heterozygous CT, and that she had given a different chromosome to her asymptomatic son than to her affected son. Gouya et al. (1996) quantitated the mRNAs transcribed from each FECH allele of the mother by a primer extension assay and by a ribonuclease protection assay. The data supported the hypothesis that in this family the EPP phenotype resulted from the coinheritance of a 'low-output' normal FECH allele (isoallele) and a mutant EX10DEL allele. The site of the mutation in the low-output allele was not determined until Gouya et al. (2002) identified an intronic single-nucleotide polymorphism (SNP), IVS3-48T-C (612386.0015), that modulates the use of a constitutive aberrant acceptor splice site 63 bp upstream of the normal one. The aberrantly spliced mRNA is degraded by a nonsense-mediated decay mechanism (NMD), producing a decreased steady-state level of mRNA and the additional FECH enzyme deficiency necessary for EPP phenotypic expression. Thus, the incomplete penetrance of EPP was explained.
Gouya et al. (2006) stated that they knew of only 7 reported cases of autosomal recessive transmission of EPP. Most reports described the inheritance as autosomal dominant with incomplete penetrance. Gouya et al. (2006) studied a cohort of 173 white French EPP families and a group of 360 unrelated healthy subjects from 4 ethnic groups. They stated that the prevalence of the recessive and dominant autosomal forms of EPP were 4% and 95%, respectively. In 97.9% of dominant cases, the IVS3-48C allele was coinherited with the deleterious mutation in trans. Other authors have described this inheritance pattern as 'pseudodominant' (Morais et al., 2011).
Molecular GeneticsIn a patient with erythropoietic protoporphyria, Lamoril et al. (1991) found compound heterozygosity for 2 different mutations in the FECH gene (612386.0001-612386.0002).
Henriksson et al. (1996) found a novel mutation in each of 4 Finnish erythropoietic protoporphyria families: 2 deletions and 2 point mutations. All 4 mutations resulted in a decreased steady-state level of the allelic transcript, since none of the mutations could be demonstrated by direct sequencing of the amplified cDNAs synthesized from total RNA extracted from the patients' lymphoblast cell lines. Henriksson et al. (1996) commented that, because the assays of ferrochelatase activity and erythrocyte protoporphyrin identified asymptomatic patients poorly, the DNA-based demonstration of a mutation is the only reliable way to screen individuals for the disease-associated mutation.
Rufenacht et al. (1998) conducted a systematic mutation analysis of the FECH gene, following a procedure that combines the exon-by-exon denaturing gradient gel electrophoresis screening of FECH genomic DNA and direct sequencing. They characterized 20 different mutations, 15 of which were described for the first time, in 26 of 29 EPP patients of Swiss and French origin. All the EPP patients, including those with liver complications, were heterozygous for the mutations identified in the FECH gene. The deleterious effect of all missense mutations was assessed by bacterial expression of the respective FECH cDNAs generated by site-directed mutagenesis. Mutations leading to a null allele were a common feature among 3 EPP pedigrees with liver complications.
Bloomer et al. (1998) focused on the gene mutations responsible for protoporphyria in patients requiring liver transplantation, i.e., those with the most severe phenotype. Mutations of the FECH gene were examined in 8 unrelated patients. RNA was prepared from liver and/or lymphoblasts, and specific reverse transcriptase-nested polymerase chain reactions were amplified and FECH cDNAs sequenced. Products shorter than normal resulted from an exon 3 deletion in 3 patients (612386.0008 and 612386.0009), exon 10 deletion in 2 (612386.0010 and 612386.0011), exon 2 deletion in 1 (612386.0012), and deletion of 5 nucleotides in exon 5 in 1 (612386.0013). Sequence of normal-sized products revealed no other mutations. Western blot showed a reduced quantity of normal-sized FECH protein in protoporphyria liver compared to normal liver. Liver FECH activity was reduced more than could be explained by the decrease in FECH protein. The gene mutations found in the most severe phenotype of protoporphyria shared the property of causing a major structural alteration in the FECH protein. Bloomer et al. (1998) suggested that the liver probably contributes to the overproduction of protoporphyrin that results in its own damage, and that the overproduction may increase as liver damage progresses.
Gouya et al. (2002) showed that the mechanism for the low expression of FECH is the IVS3-48T-C transition (612386.0015). The presence of a C at position IVS3-48 was shown to cause 40% aberrantly spliced mRNA, compared with only 20% for the T allele. The reduced level of FECH was due to degradation of the aberrantly-spliced mRNA by the mechanism of nonsense-mediated mRNA decay. The C allele was present in 11% of French control individuals, and FECH activity in lymphocytes was significantly higher in individuals who were homozygous for T at the IVS3-48 position, compared with individuals who were heterozygous (C/T). Individuals who were homozygous for C showed the lowest FECH activity.
Wiman et al. (2003) were among the first to evaluate the FECH mutations and the low-expression allele in their 26 apparently unrelated Swedish families with EPP. They found that all individuals carrying a mutated allele and IVS3-48C in trans to each other were affected by overt EPP.
In a cross-sectional study of 223 EPP patients in the U.K., Holme et al. (2006) identified 6 EPP patients with palmar keratoderma; Holme et al. (2009) studied those 6 and 3 more such EPP patients and found that they represented a subtype of EPP characterized by seasonal palmar keratoderma, relatively low erythrocyte protoporphyrin concentrations, and recessive inheritance. None had evidence of liver dysfunction; 4 patients had neurologic abnormalities. The patients were compound heterozygous or homozygous for 9 different FECH mutations; prokaryotic expression predicted that FECH activities were 2.7% to 25% of normal (mean, 10.6%). Neither mutation type nor FECH activity provided an explanation for the unusual phenotype. Holme et al. (2009) concluded that palmar keratoderma is a clinical indicator of recessive EPP and represents a new subtype of EPP occurring in 38% of reported recessive EPP families, and suggested that patients with this phenotype may carry a lower risk of liver disease than other patients with recessive EPP.
Of 11 unrelated Spanish patients with EPP, Herrero et al. (2007) found that 10 were compound heterozygous for the low-expression IVS3-48C allele in trans with another mutation in FECH, and 1 was homozygous for a novel A185T missense mutation (612386.0016).
Population GeneticsMorais et al. (2011) stated that EPP has been reported worldwide, with a prevalence between 1 in 75,000 and 1 in 200,000.
Gouya et al. (2006) found that the frequency of the IVS3-48C allele (612386.0015) differed widely in the Japanese (43%), southeast Asian (31%), white French (11%), north African (2.7%), and black west African (less than 1%) populations. These differences could be related to the prevalence of EPP in these populations and may account for the absence of EPP in black subjects. Herrero et al. (2007) found that the frequency of the IVS3-48C allele among 180 nonporphyric Spanish individuals was 5.2%.
Gouya et al. (2006) found that the phylogenetic origin of the IVS3-48C haplotypes strongly suggested that the IVS3-48C allele arose from a single recent mutational event. Estimation of the age of the IVS3-48C allele from haplotype data in white and Asian populations yielded an estimated age 3 to 4 times younger in the Japanese than in the white population, and this difference may be attributable to differing demographic histories or to positive selection for the IVS3-48C allele in the Asian population. Haplotype analysis suggested that the mutation occurred after the population had moved out of Africa.
Animal ModelIn a mutagenesis experiment using ethylnitrosourea in mice, Tutois et al. (1991) recovered a viable autosomal recessive mutation (named fch, or ferrochelatase deficiency). Homozygotes (fch/fch) displayed hemolytic anemia, photosensitivity, cholestasis, and severe hepatic dysfunction. Protoporphyrin was found at high concentration in red cells, serum, and liver. Ferrochelatase activity in various tissues was 2.7 to 6.3% of normal. Heterozygotes were not anemic and had normal liver function. They were not sensitive to light exposure and ferrochelatase activity was about 50% of normal. Southern blot analysis using a ferrochelatase cDNA probe showed no gross deletion or rearrangement of the gene. Linkage studies failed to reveal the location of the gene. Boulechfar et al. (1993) demonstrated that the molecular defect in this mutant mouse consists of a T-to-A transversion at nucleotide 293 of the Fech cDNA, leading to a methionine-to-lysine substitution at position 98 in the protein (mutation M98K).
Bloomer et al. (1987) concluded that protoporphyria in cattle was probably the result of point mutation that causes a minor change in the structure of the ferrochelatase enzyme.
HistoryFrom an analysis of the findings in the 91 families, Went and Klasen (1984) advanced the hypothesis of a 3-allele system. Patients with EPP were hypothesized to be F+/F-; the fluorocyte-positive parent, they suggested, had a genotype of f/F+ and the fluorocyte-negative parent, f/F-. On this hypothesis, 6 genotypes can occur. The f/f genotype is normal. No indication was obtained as to the phenotype associated with F-/F-. In 1 instance, both spouses had fluorocytes. They had 13 children; none was affected and 11 had fluorocytes. Thus, the F+/F+ genotype may not lead to EPP.