Biotinidase Deficiency
A number sign (#) is used with this entry because biotinidase deficiency, a form of multiple carboxylase deficiency, is caused by homozygous or compound heterozygous mutation in the BTD gene (609019) on chromosome 3p25.
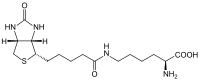
DescriptionMultiple carboxylase deficiency (MCD) is an autosomal recessive metabolic disorder characterized primarily by cutaneous and neurologic abnormalities. Symptoms result from the patient's inability to reutilize biotin, a necessary nutrient. Sweetman (1981) recognized that multiple carboxylase deficiency could be classified into early (see 253270) and late forms. The early form showed higher urinary excretion of 3-hydroxyisovaleric acid and 3-hydroxypropionic acid than the late form and was associated with normal plasma biotin concentrations. Sweetman (1981) proposed a defect in holocarboxylase synthetase and intestinal biotin absorption, respectively.
Some patients with biotinidase deficiency present in infancy (Baumgartner et al., 1985; Kalayci et al., 1994), and some individuals with this deficiency are asymptomatic (Wolf et al., 1997).
Clinical FeaturesGompertz et al. (1971) reported a patient with biotin-responsive beta-methylcrotonylglycinuria who had a deficiency of 3-methylcrotonyl-CoA carboxylase (Gompertz et al., 1973). On restudy of this patient, Sweetman et al. (1977) found that the patient was severely ketoacidotic, responded both clinically and biochemically to biotin, and excreted tiglylglycine, a metabolite of isoleucine that is excreted by patients with propionic acidemia due to propionyl-CoA carboxylase deficiency (606054). The deficiency of 2 mitochondrial carboxylases, both containing biotin, suggested that the fundamental defect was either in the transport of biotin or in the holocarboxylase synthetase that attaches biotin covalently to both carboxylases.
Charles et al. (1979) reported a presumed case of biotinidase deficiency in a 10-month-old boy who presented with dermatitis, alopecia, severe hypotonia, and developmental regression. Urinary organic acid analysis showed high levels of 3-hydroxyisovaleric acid, beta-methylcrotonylglycine, and 3-hydroxypropionic acid. Activities of propionyl CoA-carboxylase, beta-methylcrotonyl CoA-carboxylase, and pyruvate carboxylase in cultured fibroblasts were normal. Treatment with oral biotin resulted in a dramatic clinical improvement, and the authors postulated a defect in biotin absorption or transport. Lehnert et al. (1979) described a 10-week-old girl with hypotonia, recurrent seizures, and 3-methylcrotonylglycine and 3-hydroxyisovaleric acid in the urine. She also had small, but pathologic amounts of urinary propionic acid and methylcitric acid, suggesting a defect in the metabolism of biotin. Clinically and metabolically, the child responded to biotin. Bartlett et al. (1980) reported a child with a combined deficiency of propionyl-CoA carboxylase, 3-methlycrotonyl-CoA carboxylase, and pyruvate carboxylase. Cultured fibroblasts responded to administration of biotin. The primary defect was thought to involve either biotin metabolism or its intracellular transport.
Sander et al. (1980) reported a family with biotin-responsive MCD. Affected children presented with a skin rash, infections, acute intermittent ataxia, and lactic acidosis. Postmortem examination of 1 patient showed atrophy of the superior vermis of the cerebellum, similar to that seen in chronic alcoholism.
Wolf et al. (1983) reported 3 children with late-onset multiple carboxylase deficiency from 2 unrelated families. All patients had almost undetectable levels of biotinidase, whereas all 3 parents tested had an intermediate level. Wolf et al. (1983) suggested that the defect in the late-onset form of the disorder may not reside in intestinal absorption of biotin as had been suggested (Munnich et al., 1981; Thoene et al., 1982), but rather in biotinidase. Thoene and Wolf (1983) suggested that juvenile MCD probably results from impaired generation of free biotin from biotinyl residues of dietary protein. They noted that affected children are born with presumably normal stores of free biotin, but become deficient once dependent on dietary protein-bound biotin. This mechanism explained the clinical variability of the disorder and the relative delay in onset of symptoms compared to the neonatal onset in holocarboxylase synthetase deficiency.
Gaudry et al. (1983) confirmed biotinidase deficiency in a patient with multiple carboxylase deficiency and showed that the deficiency is present also in liver.
Fischer et al. (1982) reported a patient with MCD and impaired immunoregulatory functions due to defective prostaglandin E (PGE) monocyte production. Both PGE deficiency and immunoregulatory dysfunction responded to biotin administration. The authors suggested that the PGE deficiency resulted from impaired activity of acetyl-CoA carboxylase, which produces malonyl-CoA required for prostaglandin synthesis.
Wolf et al. (1985) reviewed the clinical presentation of 31 children with late-onset multiple carboxylase deficiency due to biotinidase deficiency. Symptoms usually appeared by about 3 months of age with seizures as the most frequent initial symptom. Other main features included hypotonia, ataxia, hearing loss, optic atrophy, skin rash, and alopecia. Metabolic abnormalities included ketolactic acidosis and organic aciduria. If untreated, symptoms became progressively worse, resulting in coma and death. Treatment with massive doses of biotin reversed the symptoms of alopecia, skin rash, ataxia, and developmental delay. See review of Sweetman and Nyhan (1986).
Baumgartner et al. (1985) observed that clinical and biochemical consequences of severe biotin deficiency occur within 12 days of birth. In affected patients with BTD deficiency, they found normal intestinal absorption of biotin and urinary loss of biotin and biocytin. Suormala et al. (1985) also found normal intestinal biotin absorption and increased urinary excretion of free biotin compared to controls. They concluded that renal loss of biotin was one of the factors contributing to the high biotin requirements in patients with BTD deficiency. Oral biotin supplementation resulted in increased activity of biotin-dependent carboxylases as early as 45 minutes.
Wolf et al. (1985) reported 2 patients with biotinidase deficiency who were identified among 81,243 newborns screened in the first year of a statewide screening program in Virginia. Both probands had mild neurologic symptoms at 2 and 4 months, respectively, and the 2 older sibs of 1 proband had more severe neurologic abnormalities, cutaneous findings, and developmental delay. None of the affected children had acute metabolic decompensation. Wastell et al. (1988) studied 10 patients with biotinidase deficiency. Clinical findings at presentation varied, with dermatologic signs (dermatitis and alopecia), neurologic abnormalities (seizures, hypotonia, and ataxia), and recurrent infections being the most common features, although none of these occurred in every case. Treatment with biotin resulted in pronounced, rapid clinical and biochemical improvement, but some patients had residual neurologic damage: neurosensory hearing loss, visual pathway defects, ataxia, and mental retardation.
Taitz et al. (1983) reported sensorineural deafness and severe myopia associated with a progressive retinal pigment epithelium dysplasia in a child with biotinidase deficiency, despite normal intelligence and neuromotor function. Thuy et al. (1986) reported a patient who first presented at age 5 years and had already developed sensorineural abnormalities of the optic and auditory nerves. The abnormalities did not resolve with treatment. Schulz et al. (1988) described bilateral basal ganglia calcifications in a 29-month-old girl with biotinidase deficiency who presented with ataxia.
Laryngeal stridor was a striking feature in cases of biotinidase deficiency reported by Giardini et al. (1981), Dionisi-Vici et al. (1988), and Tokatli et al. (1992). The patient of Tokatli et al. (1992) was a 30-month-old girl admitted with acute spastic laryngitis. At the ages of 10, 18, and 29 months, she had developed a noisy breathing pattern diagnosed as bronchitis that persisted for several weeks despite antibiotic therapy. At age 23 months, she developed erythematous cutaneous lesions involving the entire body, followed by seborrheic dermatitis of the scalp and sudden-onset alopecia. Laboratory analysis showed lactic acidosis and increased serum and urinary alanine. Normalization of both the respiratory symptoms and the metabolic abnormalities occurred within 2 hours of starting biotin therapy.
Kalayci et al. (1994) described 2 patients with biotinidase deficiency who were diagnosed with infantile spasms at 1 month of age. They concluded that biotinidase deficiency may present early in the neonatal period without characteristic findings such as alopecia and seborrheic dermatitis.
Suormala et al. (1990) compared 13 infants with partial biotinidase deficiency, detected in neonatal screening in Switzerland, Germany, and Austria, with 4 patients with classic biotinidase deficiency. Residual enzyme activity was present in the 'partial' cases.
Wolf et al. (1997) reported 2 unrelated asymptomatic adults with biotinidase deficiency who were diagnosed only because their affected children were identified by newborn screening. One patient was a 32-year-old Caucasian man who had never had symptoms of the disorder and showed no physical or neurologic abnormalities. His diet was not unusually enriched with biotin-containing foods, he did not pursue a low-protein diet, and he did not take supplemental vitamins. His parents were consanguineous and he was related to his wife. The family of this man and his wife was of German ancestry and could be traced back to the 1750s to a common founding ancestor who lived in the same small rural community in northwestern Virginia where they lived. The second asymptomatic adult reported by Wolf et al. (1997) was a 36-year-old Caucasian woman who had had no symptoms of the disorder and no dietary restrictions or abnormalities. A 15-year-old daughter was also found to have profound biotinidase deficiency but no clinical symptoms of the disorder, with the possible exception of a skin rash that occurred a few months earlier, was described as 'hives,' and resolved spontaneously. The mother's parentage was French Canadian and consanguineous; her husband was of northern Irish background and not known to be related to her.
Biochemical FeaturesHart et al. (1992) studied the biochemical and immunologic characteristics of biotinidase in sera from 68 children with profound biotinidase deficiency (defined as less than 10% of mean normal activity) who had been identified symptomatically and by newborn screening. Patients could be classified into at least 9 distinct biochemical phenotypes, on the basis of the presence or absence of crossreacting material (CRM) to biotinidase, the number of isoelectric focusing isoforms, and the distribution frequency of the isoforms. No relationship was found between either the age at onset or the severity of symptoms and the isoform patterns or CRM status of the symptomatic children.
Clinical ManagementSuormala et al. (1990) suggested treatment with biotin for all patients with residual activities below 10%.
Molecular GeneticsIn 10 of 25 patients with biotinidase deficiency, Pomponio et al. (1995) identified an allele with a 7-bp deletion and a 3-bp insertion in the BTD gene (609019.0001). In 37 symptomatic children (30 index cases and 7 sibs) with profound biotinidase deficiency, Pomponio et al. (1997) identified 21 mutations in the BTD gene. The 2 most common mutations were the del7/ins3 mutation and R538C (609019.0003); these 2 mutations were found in 31 of 60 alleles (52%), whereas the remainder of the alleles were accounted for by the 19 other unique mutations.
In 2 unrelated asymptomatic adults with biotinidase deficiency who were diagnosed because their children were identified by newborn screening, Wolf et al. (1997) identified 2 different homozygous mutations in the BTD gene (609019.0005; 609019.0006). Wolf et al. (1997) concluded that epigenetic factors may protect some enzyme-deficient individuals from developing symptoms.
Pomponio et al. (2000) identified mutations in the BTD gene (609019.0001; 609019.0009-609019.0011) in Turkish children with biotinidase deficiency identified both clinically and by newborn screening.
Genotype/Phenotype CorrelationsSivri et al. (2007) reported 20 Turkish patients with biotinidase deficiency. All except 1 were born of consanguineous parents. Variable hearing loss was present in 11 (55%) children. There were no significant differences in mean age of onset of symptoms, age of diagnosis, or time from onset to diagnosis between those with hearing loss and those with normal hearing. However, all symptomatic children with hearing loss were homozygous for null mutations in the BTD gene, whereas symptomatic children without hearing loss were all homozygous for missense mutations resulting in some residual protein function. Most notably, 3 symptom-free children, who had been ascertained and treated soon after birth because an older sib was affected, had normal hearing despite being homozygous for a null mutation. Combined with previous data, Sivri et al. (2007) concluded that homozygosity or compound heterozygosity for null mutations increases the risk that a symptomatic patient with biotinidase deficiency will have hearing loss, and noted that early treatment is beneficial.
Population GeneticsNewborn Screening
Newborn screening for biotinidase deficiency identifies children with profound biotinidase deficiency (less than 10% of mean normal serum activity) and those with partial biotinidase deficiency (10 to 30% of mean normal serum activity). Children with partial biotinidase deficiency who are not treated with biotin do not exhibit symptoms unless they are stressed by prolonged infection (Swango et al., 1998). Wolf et al. (1985) described a simple, rapid, semiquantitative colorimetric method that could be done on whole blood spotted on filter paper as for PKU (261600) testing.
In northeastern Italy, Burlina et al. (1988) incorporated screening of biotinidase deficiency into a neonatal mass screening program. During a 6-month period, 1 affected infant was identified among 24,300 newborns, which the authors noted was as common as other well-known metabolic disorders for which mass screening was available.
On the basis of the screening of 163,000 newborn filter-paper blood samples for serum biotinidase deficiency, Dunkel et al. (1989) identified 3 with complete deficiency, representing an incidence of 18.4 cases per million live births, and 12 with partial deficiency. The complete deficiency cases represented homozygotes and the partial deficiency cases heterozygotes. The number of heterozygotes found by screening was much less than predicted, probably because the screening test detected only outliers. Biotinidase deficiency was found to be more common in French Canadians than in other ethnic groups in Quebec; however, no evidence of regional clustering or founder effect was detected.
Weissbecker et al. (1991) explored 3 statistical methods for identifying heterozygotes on the basis of serum biotinidase activity. By the preferred method, frequency of heterozygotes in an adult French population was estimated to be 0.012, which was similar to that estimated from the results of neonatal screening.
Kennedy et al. (1989) reported the results of a neonatal screening program for biotinidase deficiency in Scotland. Of 102,393 infants screened from 1985 to 1987, no positive cases were found. Minns and Kirk (1994) reported that, after discontinuation of the pilot study, 3 cases of biotinidase deficiency had been diagnosed in Scotland.
Norrgard et al. (1999) compared the mutations in a group of 59 children with profound biotinidase deficiency who were identified by newborn screening in the United States with those in 33 children ascertained by exhibiting symptoms. Of the 40 total mutations identified among the 2 populations, 4 mutations comprised 59% of the disease alleles studied. Two of these mutations occurred in both populations, but in the symptomatic group at a significantly greater frequency. The other 2 common mutations occurred only in the newborn screening group. Because 2 common mutations did not occur in the symptomatic population, Norrgard et al. (1999) considered it possible that individuals with these mutations either developed mild or no symptoms if left untreated. However, biotin treatment was still recommended.
Hymes et al. (2001) reported that 61 mutations in 3 of the 4 exons of the BTD gene and 1 mutation in an intron had been described as the cause of profound BTD deficiency. Two mutations, del7/ins3 and R538C, were present in 52% or 31 of 60 alleles found in symptomatic patients. Three other mutations accounted for 52% of alleles detected by newborn screening in the United States.
Muhl et al. (2001) identified 21 patients with profound and 13 unrelated patients with partial biotinidase deficiency from 30 unrelated families during a 12-year nationwide newborn screening in nearly 1 million newborns in Austria. By DGGE analysis and sequencing, they detected 59 of the 60 (98%) expected mutant alleles. A total of 13 different mutations were identified, with 4 common mutations comprising 78% of the BTD alleles. Of 13 children with partial biotinidase deficiency, the D444H mutation (609019.0005) was found in 12, usually with a mutation causing profound deficiency in the other allele. Only 2 patients homozygous for a frameshift mutation had no measurable residual enzyme activity, and both patients developed clinical symptoms before biotin supplementation. The authors concluded that mutation analysis could not predict whether or not an untreated patient will develop symptoms; however, they found it essential to differentiate biochemically between patients with lower or higher than 1% residual biotinidase activity.