Cerebral Creatine Deficiency Syndrome 2
A number sign (#) is used with this entry because cerebral creatine deficiency syndrome-2 (CCDS2), also known as guanidinoacetate methyltransferase (GAMT) deficiency, is caused by homozygous or compound heterozygous mutation in the GAMT gene (601240) on chromosome 19p13.
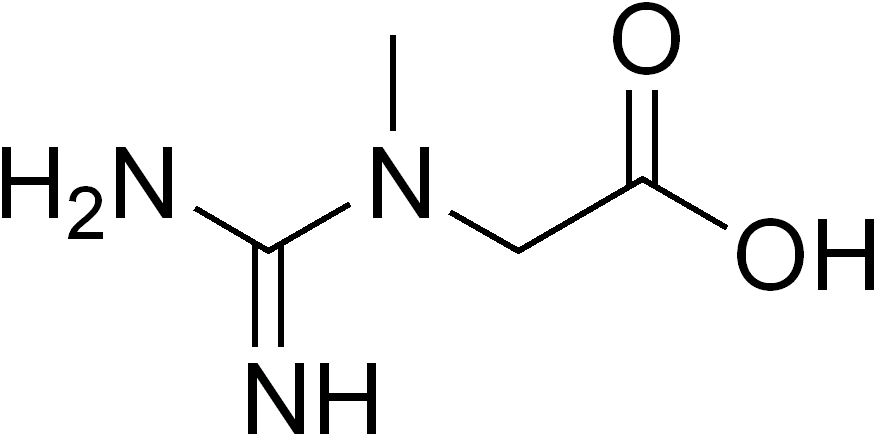
DescriptionGuanidinoacetate methyltransferase deficiency, an autosomal recessive inborn error of creatine synthesis, is characterized by developmental delay/regression, mental retardation, severe disturbance of expressive and cognitive speech, intractable seizures and movement disturbances, severe depletion of creatine/phosphocreatine in the brain, and accumulation of guanidinoacetic acid (GAA) in brain and body fluids (summary by Schulze, 2003).
For a general phenotypic description and a discussion of genetic heterogeneity of CCDS, see CCDS1 (300352).
Clinical FeaturesStockler et al. (1994) reported a 22-month-old male infant with muscular hypotonia, progressive extrapyramidal movement disorder, an extremely low excretion of creatine, deficiency of creatine and creatine phosphate, and simultaneous accumulation of guanidinoacetate in brain, as detected by in vivo proton and phosphorus magnetic resonance spectroscopy. The clinical symptoms and biochemical abnormalities improved significantly after oral administration of creatine monohydrate. The observations suggested an enzyme defect in creatine biosynthesis at the level of GAMT activity. Stockler et al. (1996) studied a second patient, aged 4 years, with similar biochemical and spectroscopic findings and severe developmental delay, muscular hypotonia, ataxia, and intractable seizures as the predominant clinical symptoms. Deficiency of GAMT in liver was demonstrated.
Schulze et al. (1997) reported findings in a female infant born of first-cousin Kurdish parents. She had psychomotor retardation at age 2.5 years. At 3 years she began to lose acquired skills. From 14 months she had intractable grand mal and absence seizures. This child also exhibited dyskinetic and dystonic involuntary movements and pyramidal signs including increased muscle tone of the lower limbs, increased deep tendon reflexes, and myoclonic jerks. MRI revealed marked myelination delay. Plasma creatinine was in the low normal range, and 24-hour creatinine excretion was markedly reduced. Urinary excretion of guanidinoacetic acid was greatly increased. In this infant, creatine therapy did not influence the course of epilepsy and its sequelae.
Caldeira Araujo et al. (2005) investigated 180 institutionalized patients with a severe mental handicap for urine and plasma uric acid and creatinine. Patients with an increased urinary uric acid/creatinine ratio and/or decreased creatinine were subjected to the analysis of guanidinoacetate. Four patients were identified with GAMT deficiency: 2 sisters, aged 26 and 29 years, respectively, and their 8-year-old male third cousin, and an isolated case in an unrelated family who was 19 years old at the time of report. A fifth patient had died before a biochemical diagnosis could be made. All patients had shown normal psychomotor development in the first year of life, after which they developed profound mental retardation. Three of 4 had convulsions and all 4 totally lacked the development of speech. Their GAMT activity in lymphoblasts was impaired. Caldeira Araujo et al. (2005) concluded that GAMT deficiency in adults is associated with severe mental retardation and absent or limited speech development; convulsions may be prominent.
DiagnosisSchulze et al. (1997) noted that the finding of low CSF creatine and creatinine constitutes a reliable diagnostic method for GAMT deficiency. Magnetic resonance spectroscopy of brain is diagnostic in that it reveals creatine depletion and guanidinoacetate phosphate accumulation.
Verhoeven et al. (2000) reported that creatinine in plasma from 2 GAMT-deficient patients appeared normal when measured by the Jaffe method but was decreased when measured enzymatically or by HPLC. The apparently normal levels of creatinine as measured by the Jaffe method were not caused by guanidinoacetate. In urine, the Jaffe method and the enzymatic method gave similar results, indicating that in urine no false elevations of creatinine can be expected. As the Jaffe method is still widely used for routine plasma creatinine measurements, Verhoeven et al. (2000) concluded that it is important to know that it cannot be used to exclude GAMT deficiency.
GAMT-deficient patients have elevated plasma guanidinoacetate (GAA). Among 33 patients referred for genetic testing for mutations in the GAMT gene who had biochemical data available, Comeaux et al. (2013) found that 16 had normal GAA plasma levels and were not sequenced for GAMT mutations. Abnormal results were found in 17 patients: 8 carried mutations and 9 were negative for mutations. Four of the 9 who were negative for mutations were found to have normal GAA levels on repeat testing, and the other 5 had only nonspecific marginally increased GAA. The findings indicated that plasma GAA levels as a biomarker has 100% specificity for GAMT mutations (no individuals with normal GAA had mutations), but low sensitivity (marginally high GAA does not necessarily indicate GAMT mutations).
Clinical ManagementIn a physician-based survey of 48 patients from 38 families with CCDS2, Stockler-Ipsiroglu et al. (2014) evaluated the effectiveness of treatment of the disorder with various combinations/dosages of creatine-monohydrate, L-ornithine, sodium benzoate, and protein/arginine-restricted diets. Forty-four patients, all treated after 9 months of age, including 2 who had never received treatment, had developmental delay or intellectual disability. Thirty-five patients had seizures, and 13 had a movement disorder. Therapy was associated with improvement or stabilization of symptoms in all symptomatic cases. The 4 patients treated before age 9 months had normal or almost normal developmental outcomes. Reduction of plasma guanidinoacetate levels appeared to improve long-term outcomes. Stockler-Ipsiroglu et al. (2014) provided consensus recommendations for the diagnosis, treatment, and monitoring of patients with CCDS2.
Molecular GeneticsIn 2 patients with GAMT deficiency, Stockler et al. (1996) identified mutations in the GAMT gene; one patient was homozygous and the other was compound heterozygous (see 601240.0001 and 601240.0002).
In 3 family members and an isolated patient with GAMT deficiency, Caldeira Araujo et al. (2005) identified homozygous mutations in the GAMT gene (601240.0003-601240.0004, respectively).
In a North African patient with GAMT deficiency and severe mental retardation, born of consanguineous parents, Lion-Francois et al. (2006) identified a homozygous missense mutation in the GAMT gene (601240.0005). The patient had delayed onset of walking, seizures, and autistic features.
Animal ModelSchmidt et al. (2004) generated a knockout mouse model for GAMT deficiency by gene targeting in embryonic stem cells. Gamt -/- mice had markedly increased guanidinoacetate and reduced creatine and creatinine levels in brain, serum, and urine, similar to human GAMT patients. In vivo 31P magnetic resonance spectroscopy showed high levels of PGAA and reduced levels of creatine phosphate in heart, skeletal muscle, and brain. GAMT deficiency was associated with increased neonatal mortality, muscular hypotonia, decreased male fertility, and a non-leptin-mediated lifelong reduction in body weight due to reduced body fat mass.