Fungal Sinusitis
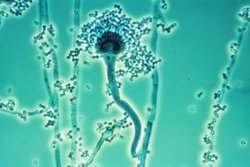
Fungal sinusitis is the inflammation of the lining mucosa of the paranasal sinuses due to fungal infection. It occurs in people with reduced immunity. The maxillary sinus is the most commonly involved. Fungi responsible for fungal sinusitis are Aspergillus fumigatus (90%), Aspergillus flavus, and Aspergillus niger. Fungal sinusitis occurs most commonly in middle-aged populations. Diabetes mellitus is the most common risk factor involved.
Types
The types of fungal sinusitis are based on invasive and non-invasive as follows:
- Invasive
- Acute fulminant
- Chronic invasive
- Granulomatous
- Non Invasive
- Saprophytic infection
- Sinus fungal ball
- Eosinophil related FRS including AFRS
Signs and symptoms
Individuals with the condition of fungal sinusitis mostly present with features that include facial pain and pain around the eyes, nasal congestion, rhinorrhea(running nose), headache, later there may be ophthalmoplegia (paralysis of ocular muscles).
Pathophysiology
The mechanism of fungal sinusitis depends on which form, such as:
- Acute fulminant form – the fungus invades into vessels causing thrombosis, necrosis with minimum inflammation
- Chronic invasive – fungal hyphae invades tissue leaving necrosis with minimal inflammation
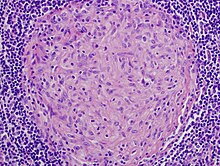
- Granulomatous form – invasive hyphae invades tissue with inflammation and non-caseating granuloma (with foreign bodies).
- Saprophytic infection – growth of fungus seen on mucous crusts within sinus cavity.
- Sinus fungal ball – sequestration of fungal hyphae as densely tangled, and has gritty matted appearance.
- Eosinophil related Allergic fungal sinusitis – though not completely understood, a possible mechanism sees the protein component of fungus elicits IgE mediated allergic mucosal inflammation.
Diagnosis
In terms of diagnosis, the clinical examination gives an idea about fungal sinusitis, as well as:

- Suggestive clinical features include - multiple recurrent episodes, persistent pathology, and absent ability to smell (the Eustachian tube may also be affected).
- X Ray - can be done if the diagnosis is not certain.
- CT – can document the presence of sinusitis, in the coronal views
- MRI – used to find the CNS spread (extent of the disease), to evaluate individuals who demonstrate signs of invasive fungal sinusitis
- Histology studies
Treatment
Treatment for fungal sinusitis can include surgical debridement; helps by slowing progression of disease thus allowing time for recovery additionally we see the options below:
- In cases where the fungus has invaded the sinus tissue, echinocandins, oral voriconazole, and I.V amphoterecin may be used
- For allergic fungal sinusitis, systemic corticosteroids like prednisolone, methylprednisolone are added for their anti-inflammatory effect, bronchodilators and expectorants help to clear secretions in the sinuses.
Epidemiology
Though it is widely held that fungal infections of the nose and paranasal sinuses are not common, most agree that their frequency has been increasing over past decades.
See also
- Granuloma