Cerebral Creatine Deficiency Syndrome 1
A number sign (#) is used with this entry because cerebral creatine deficiency syndrome-1 (CCDS1) is caused by mutation in the creatine transporter gene (SLC6A8; 300036) on chromosome Xq28.
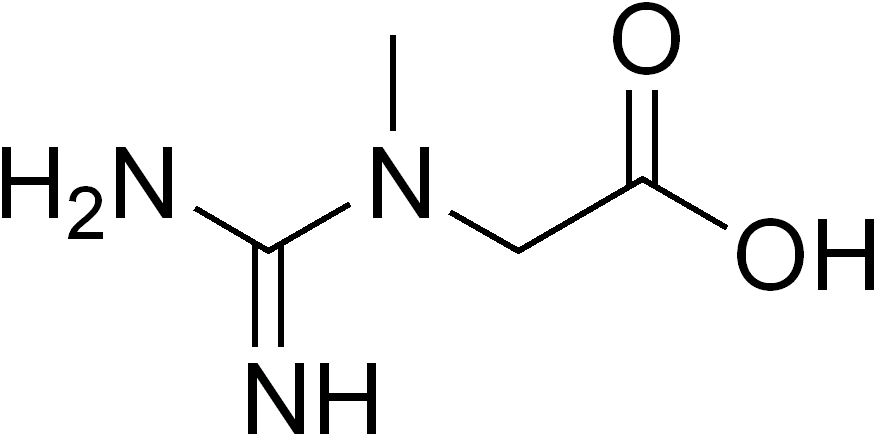
DescriptionCerebral creatine deficiency syndrome-1 is an X-linked disorder of creatine (Cr) transport characterized by mental retardation, severe speech delay, behavioral abnormalities, and seizures. It has a prevalence of 0.3 to 3.5% in males. Carrier females may show mild neuropsychologic impairment (summary by van de Kamp et al., 2011).
Genetic Heterogeneity of Cerebral Creatine Deficiency Syndrome
See also CCDS2 (612736), caused by mutation in the GAMT gene (601240) on chromosome 19p13, and CCDS3 (612718), caused by mutation in the AGAT gene (GATM; 602360) on chromosome 15q21.
Clinical FeaturesSalomons et al. (2001) reported a male patient with developmental delay and hypotonia. Proton magnetic resonance spectroscopic imaging (H-MRSI) of his brain revealed absence of the creatine signal. However, creatine in urine and plasma was increased, and guanidinoacetate (see 612718) levels were normal. Fibroblasts from the index patient were defective in creatine uptake. Three female relatives had mild biochemical abnormalities and learning disabilities.
Bizzi et al. (2002) reported a child with severe neurologic disturbances including seizures, behavioral problems, speech delay, and inability to engage in structured play, as well as creatine deficiency. H-MRSI showed absence of creatine in the whole brain, which was not corrected by creatine supplementation.
Hahn et al. (2002) described a family in which 5 males in a sibship of 10 had mental retardation with seizures. Head circumference was normal in all. Adult height (162.5-167.5 cm) was less than the adult height of the unaffected brother (175.5 cm). Midface hypoplasia was also described. Gastrointestinal disturbances in the form of chronic constipation, megacolon, gastric and duodenal ulcer disease, and bowel perforation were also observed. Two sisters had mild cognitive impairment, and one of them had chronic behavioral disturbances. Biochemical analyses confirmed a defect in creatine metabolism in this family. In affected males patients, the level of urinary creatine was substantially increased, and creatine uptake in fibroblasts was decreased.
Schiaffino et al. (2005) reported a patient with X-linked creatine deficiency confirmed by genetic analysis (300036.0006). The patient was first seen at age 21 months for failure to thrive, recurrent vomiting, and motor delay. His weight, length, and head circumference were all under the third percentile. Neurologic examination showed truncal hypotonia, impaired eye-hand coordination, and severe cognitive and language retardation. EEG showed slow, diffuse hypersynchronisms with abnormal multifocal spikes. Plasma creatine levels were consistently low, and biochemical studies on fibroblasts showed impaired creatine uptake. Schiaffino et al. (2005) noted that few patients with SLC6A8 deficiency had been described, precluding a definite clinical description. However, most affected males have mental retardation, seizures, and language impairment.
Kleefstra et al. (2005) described 2 brothers with X-linked creatine deficiency, in whom Rosenberg et al. (2004) had identified a missense mutation in the SLC6A8 gene (300036.0007). The older brother, born with severe mental retardation, was examined at age 70 and found to have myopathic facies with ptosis, external ophthalmoplegia, and open, hanging mouth. The younger brother had milder mental retardation and learned to read and write, but underwent regression at age 51 after the death of their father. In his fifties, he had urethral stenosis, chronic constipation, and ileus, and spontaneous luxations of several digits occurred. Neurologic examination at age 67 showed apparent medication-related Parkinsonism, upward gaze paresis, expressionless face, and hanging mouth and shoulders; comparison of photographs at age 57 and 64 revealed the striking progression of clinical features in the latter patient. Their sister, a carrier of the mutation, had short stature, learning difficulties, and developed severe constipation requiring surgical intervention in her fifties.
Clark et al. (2006) reported 6 unrelated males with X-linked mental retardation associated with mutations in the SLC6A8 gene. Clinical features included increased urinary creatine:creatinine (Cr:Crn) ratio, microcephaly, long, narrow face, and prominent chin. Two patients were tall and thin, and 3 had short stature.
Battini et al. (2007) reported a 9.5-year-old Italian boy with moderate mental retardation and verbal dyspraxia associated with mutation in the SLC6A8 gene. He had delayed psychomotor development, hypotonia, seizures, and severe language deficit with oral-motor dyspraxia, irritability, and temper tantrums. Detailed language evaluation showed problems in picture naming and phonetics, whereas receptive vocabulary was less severely affected. Social interaction was good despite the severe expressive limitation.
Battini et al. (2011) reported a 6.5-year-old boy with X-linked creatine deficiency syndrome confirmed by genetic analysis. In infancy, he showed poor feeding, hypotonia, and delayed psychomotor development with walking and speaking his first words at age 3 years. Examination at age 5 years showed mild intellectual disability and comparatively severe language delay with mild oromotor dyspraxia and clumsiness. Social interaction was good. Detailed neuropsychologic studies showed a discrepancy between nonverbal and verbal skills, with mild impairment of social personal performance and eye-hand coordination and moderate impairment of speech and practical reasoning. Spontaneous language performance was markedly reduced. Biochemical analysis showed increased urinary Cr, increased Cr/Crn ratio, and undetectable uptake of Cr in fibroblasts, and magnetic resonance spectroscopy showed a reduced Cr peak in the brain. The patient's mother, who also carried the mutation, had a normal biochemical profile, but borderline intellectual functioning with difficulties in reading comprehension.
Comeaux et al. (2013) reported 22 patients with confirmed deleterious mutations in the SLC6A8 gene who had clinical information available. Clinical features included developmental delay (86%), seizures (27%), autistic features (18%), speech delay (27%), ataxia (14%), and choreoathetosis (9%). All 6 patients with MRS results had decreased or absent creatine peaks.
Van de Kamp et al. (2013) performed a retrospective analysis of 101 male patients from 85 families with X-linked creatine transporter deficiency confirmed by genetic analysis. Many of the patients had previously been reported. All patients presented in infancy or early childhood, most often due to delayed psychomotor development. All had intellectual disability of varying degrees, and 85% had behavioral problems. Speech development was especially delayed, but almost a third of patients could speak in sentences. Other features included seizures (59%), hypotonia (40%), spasticity (26%), gastrointestinal symptoms (35%), and ophthalmologic abnormalities (10%). Various facial dysmorphic features were present in 45%. MRI showed mild structural abnormalities in 53 of 76 patients studied, and MRS showed reduced creatine in all 66 patients for whom results were available. Urinary creatine was increased in 81 patients for whom results were available. A few patients studied had unexpectedly high creatine levels in CSF, suggesting that the brain is able to synthesize creatine and that the creatine deficiency is caused by a defect in the reuptake of creatine within neurons. Most patients had missense mutations or deletions of 1 amino acid in the SLC6A8 gene. A third of patients had a de novo mutation in the SLC6A8 gene. However, van de Kamp et al. (2013) suggested that a mother with an affected son with a de novo mutation may have a recurrence risk in further pregnancies due to the possibility of low level somatic or germline mosaicism.
Carrier Females
Van de Kamp et al. (2011) studied 8 unrelated female carriers of SLC6A8 mutations identified though affected male relatives. One woman had mental retardation, 1 required special education, 3 failed a year during elementary school, and 3 had no learning difficulties. IQ scores ranged from 48 to 96; 2 had scores in the mental retardation range, and 4 had scores in the borderline range. MRI showed mild cerebellar symptoms in 2, and constipation was reported in 2. Only 3 of 8 women had a mildly elevated urine creatine/creatinine ratio. H-MRSI studies showed decreased total creatine concentrations in the brain overall, but individual females had levels overlapping that of controls. X-inactivation studies in cultured fibroblasts showed severely skewed patterns in 2 woman, 1 favoring the mutant allele and 1 favoring the wildtype allele, but this may have been an artifact. Van de Kamp et al. (2011) concluded that carrier females may have mild symptoms of the disorder, and suggested that the most accurate diagnostic strategy in females should be molecular diagnosis, as biochemical changes may be subtle or not present.
DiagnosisThe biochemical test for CCDS1 is the urine creatine:creatinine ratio, which should be above 1.5 for a diagnosis of the disorder in males. Among 69 patients referred for SLC6A8 mutation testing, Comeaux et al. (2013) found that 45 had normal primary or secondary urine screens and did not meet the criteria for gene testing. Twelve of the 45 were females, whose ratios may have been uninformative due to random X-chromosome inactivation. Seven males and 2 females with increased ratios in the first screen had normal ratios in a second sample; none of these patients carried SLC6A8 mutations. The negative predictive value of this test in this study was 100%; all 45 patients with urine creatine:creatinine ratios below 1.5, regardless of gender, had no SLC6A8 mutations. Comeaux et al. (2013) emphasized that the urine creatine:creatinine ratio may be misleading because of diet and the possibility of creatine supplementation.
Clinical ManagementVan de Kamp et al. (2012) recorded the long-term follow-up and treatment of 9 boys between the ages of 8 months and 10 years with creatine transporter defect. The patients underwent repeated magnetic resonance spectroscopy (MRS) and neuropsychologic assessments during 4 to 6 years of combination treatment with creatine monohydrate, L-arginine, and glycine. Treatment did not lead to a significant increase in cerebral creatine content as observed with MRS. After an initial improvement in locomotor and personal-social IQ subscales, no lasting clinical improvement was recorded. Additionally, van de Kamp et al. (2012) noticed an age-related decline in IQ subscales in boys affected with creatine transporter defect.
Valayannopoulos et al. (2012) reported a series of 6 patients with severe creatine transporter deficiency, 4 males and 2 females. Clinical presentations included mild to severe mental retardation in all 6 patients, associated with psychiatric symptoms (autistic behavior, chronic hallucinatory psychosis) in 5 of 6, seizures in 2 of 6, and muscular symptoms in 2 of the 4 males. Diagnosis was confirmed by molecular analysis in all patients. All patients were treated successively according to the same protocol with creatine alone and then by creatine combined to its precursors L-glycine and L-arginine for 42 months. Valayannopoulos et al. (2012) reported benefit only in the muscular symptoms of the disease and no improvement in the cognitive and psychiatric manifestations. Treatment failed to modify brain creatine content in either male or female patients.
Dunbar et al. (2014) performed a systematic literature review (2001-2013) comprising 7 publications that described 25 patients with creatine transporter deficiency, and 3 additional patients treated at the authors' institution. Two patients received creatine-monohydrate supplementation; 7 received L-arginine; 2 received creatine-monohydrate and L-arginine; and 17 received a combination of creatine-monohydrate, L-arginine, and glycine. Median treatment duration was 34.6 months (range 3 months to 5 years). A total of 10 patients (36%) demonstrated response to treatment, manifested by either an increase in cerebral creatine or improved clinical parameters. Seven of the 28 patients had quantified pre- and posttreatment creatine, and it was significantly increased posttreatment. All of the patients with increased cerebral creatine also experienced clinical improvement. In addition, the majority of patients with clinical improvement had detectable cerebral creatine prior to treatment. Ninety percent of the patients who improved were initiated on treatment before 9 years of age. Dunbar et al. (2014) proposed systematic screening for creatine transporter deficiency in patients with intellectual disability, to allow early initiation of treatment with oral creatine, arginine, and/or glycine supplementation.
Molecular GeneticsIn a male patient with developmental delay and defective creatine uptake, Salomons et al. (2001) identified a hemizygous nonsense mutation in the SLC6A8 gene (300036.0001). Three mildly affected female relatives were heterozygous for the mutation.
In the child with severe neurologic deficits and creatine deficiency, Bizzi et al. (2002) identified a hemizygous 3-bp deletion in the SLC6A8 gene (300036.0003). The patient's mother was heterozygous for the mutation.
In the family described by Hahn et al. (2002), linkage to Xq28 was indicated by a lod score of 2.40 at zero recombination with 7 markers. Mutation analysis of candidate genes in that region revealed a splice site mutation in the SLC6A8 gene (300036.0002). Two sisters of the 5 affected males were heterozygous for the SLC6A8 mutation and exhibited mild mental retardation with behavior and learning problems.
Rosenberg et al. (2004) identified 2 different mutations in the SLC6A8 gene (300036.0004; 300036.0005) in affected members of 2 unrelated families with X-linked mental retardation.
Clark et al. (2006) identified 4 pathogenic (see, e.g., 300036.0010) and 2 potentially pathogenic mutations in the SLC6A8 gene in 6 of 478 unrelated males with X-linked mental retardation, yielding a frequency of approximately 1%. The authors stated that a total of 18 pathogenic mutations in the SLC6A8 gene had been reported, and suggested that urinary screening for an increased creatine:creatinine ratio could lead to focused mutation testing among appropriate patients.
Lion-Francois et al. (2006) identified 4 unrelated boys with severe mental retardation due to X-linked creatine deficiency. Four different mutations were identified in the SLC6A8 gene (see, e.g., 300036.0008; 300036.0009). Together with a fifth case of creatine deficiency due to mutation in the GAMT gene (612736), Lion-Francois et al. (2006) found that the prevalence of cerebral creatine deficiency syndromes was 2.7% in their study population of 188 mentally retarded children. The prevalence rose to 4.4% when only boys were considered.