Glycogen Storage Disease
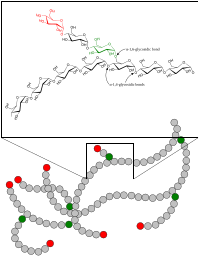
A glycogen storage disease (GSD, also glycogenosis and dextrinosis) is a metabolic disorder caused by enzyme deficiencies affecting either glycogen synthesis, glycogen breakdown or glycolysis (glucose breakdown), typically in muscles and/or liver cells.
GSD has two classes of cause: genetic and acquired. Genetic GSD is caused by any inborn error of metabolism (genetically defective enzymes) involved in these processes. In livestock, acquired GSD is caused by intoxication with the alkaloid castanospermine.
Types
| Type (Eponym) |
Enzyme deficiency (Gene) |
Incidence (births) | Hypo- glycemia? |
Hepato- megaly? |
Hyperlip- idemia? |
Muscle symptoms | Development/ prognosis | Other symptoms |
|---|---|---|---|---|---|---|---|---|
| GSD 0 | Glycogen synthase (GYS2) |
? | Yes | No | No | Occasional muscle cramping | Growth failure in some cases | |
| GSD I / GSD 1 (von Gierke's disease) |
Glucose-6-phosphatase (G6PC / SLC37A4) |
1 in 50,000 – 100,000 | Yes | Yes | Yes | None | Growth failure | Lactic acidosis, hyperuricemia |
| GSD II / GSD 2 (Pompe disease ) |
Acid alpha-glucosidase (GAA) |
1 in 13,000. | No | Yes | No | Muscle weakness | Progressive proximal skeletal muscle weakness with varied timeline to threshold of functional limitation (early childhood to adulthood). Approximately 15% of the Pompe population is classified as infantile Pompe which is typically deadly within the first year if untreated. | Heart failure (infantile), respiratory difficulty (due to muscle weakness) |
| GSD III / GSD 3 (Cori's disease or Forbes' disease) |
Glycogen debranching enzyme (AGL) |
1 in 100,000 | Yes | Yes | Yes | Myopathy | ||
| GSD IV / GSD 4 (Andersen disease) |
Glycogen branching enzyme (GBE1) |
1 in 500,000 | No | Yes, also cirrhosis |
No | Myopathy and dilated cardiomyopathy | Failure to thrive, death at age ~5 years | |
| GSD V / GSD 5 (McArdle disease) |
Muscle glycogen phosphorylase (PYGM) |
1 in 100,000 – 500,000 | No | No | No | Exercise-induced cramps, Rhabdomyolysis | Renal failure by myoglobinuria, second wind phenomenon | |
| GSD VI / GSD 6 (Hers' disease) |
Liver glycogen phosphorylase (PYGL) Muscle phosphoglycerate mutase (PGAM2) |
1 in 65,000 – 85,000 | Yes | Yes | Yes | None | initially benign, developmental delay follows. | |
| GSD VII / GSD 7 (Tarui's disease) |
Muscle phosphofructokinase (PFKM) |
1 in 1,000,000 | No | No | No | Exercise-induced muscle cramps and weakness | developmental delay | In some haemolytic anaemia |
| GSD IX / GSD 9 | Phosphorylase kinase (PHKA2 / PHKB / PHKG2 / PHKA1) |
? | Yes | Yes | Yes | None | Delayed motor development, Developmental delay | |
| GSD X / GSD 10 | Phosphoglycerate mutase
(PGAM2) |
? | ? | ? | ? | Exercise-induced muscle cramps and weakness | Myoglobinuria | |
| GSD XI / GSD 11 | Muscle lactate dehydrogenase (LDHA) |
? | ? | ? | ? | |||
| Fanconi-Bickel syndrome formerly GSD XI / GSD 11, no longer considered a GSD |
Glucose transporter (GLUT2) |
? | Yes | Yes | No | None | ||
| GSD XII / GSD 12 (Aldolase A deficiency) |
Aldolase A (ALDOA) |
? | No | In some | No | Exercise intolerance, cramps. In some Rhabdomyolysis. | Hemolytic anemia and other symptoms | |
| GSD XIII / GSD 13 | β-enolase (ENO3) |
? | No | ? | No | Exercise intolerance, cramps | Increasing intensity of myalgias over decades | Serum CK: Episodic elevations; Reduced with rest |
| GSD XV / GSD 15 | Glycogenin-1 (GYG1) |
Rare | No | No | No | Muscle atropy | Slowly progressive weakness over decades | None |
Remarks:
- Some GSDs have different forms, e.g. infantile, juvenile, adult (late-onset).
- Some GSDs have different subtypes, e.g. GSD1a / GSD1b, GSD9A1 / GSD9A2 / GSD9B / GSD9C / GSD9D.
- GSD type 0: Although glycogen synthase deficiency does not result in storage of extra glycogen in the liver, it is often classified with the GSDs as type 0 because it is another defect of glycogen storage and can cause similar problems.
- GSD type VIII (GSD 8): In the past it was considered a distinct condition, however it is now classified with GSD type VI or GSD IXa1; it has been described as X-linked recessive inherited.
- GSD type XI (GSD 11): Fanconi-Bickel syndrome, hepatorenal glycogenosis with renal Fanconi syndrome, no longer considered a glycogen storage disease.
- GSD type XIV (GSD 14): Now classed as Congenital disorder of glycosylation type 1 (CDG1T), affects the phosphoglucomutase enzyme (gene PGM1).
- Lafora disease is considered a complex neurodegenerative disease and also a glycogen metabolism disorder.
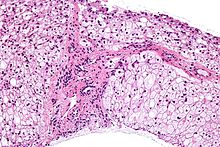
Diagnosis
Treatment
Treatment is dependent on the type of glycogen storage disease. GSD I is typically treated with frequent small meals of carbohydrates and cornstarch, called modified cornstarch therapy, to prevent low blood sugar, while other treatments may include allopurinol and human granulocyte colony stimulating factor.
Epidemiology
Overall, according to a study in British Columbia, approximately 2.3 children per 100,000 births (1 in 43,000) have some form of glycogen storage disease. In the United States, they are estimated to occur in 1 per 20,000–25,000 births. Dutch incidence rate is estimated to be 1 per 40,000 births. While a Mexican incidence showed 6.78:1000 male newborns.