Sjogren Syndrome
Description
Sjogren syndrome is an autoimmune disease that mainly affects the exocrine glands. It is clinically characterized by keratoconjunctivitis sicca and xerostomia (Goransson et al., 2006).
See 200400 for association of Sjogren syndrome with achalasia in sisters.
Clinical FeaturesLichtenfeld et al. (1976) noted familial occurrence. This probably represents the same sort of familial occurrence as is seen with systemic lupus erythematosus (SLE; 152700) and other autoimmune disorders. Moutsopoulos et al. (1979) used the term primary or secondary sicca syndrome depending, respectively, on whether or not the disorder was associated with another autoimmune disease. They found a strong association with HLA-Dw3 and HLA-Dw4.
Expression of HLA-DR antigen (see 142860) and intracellular adhesion molecule-1 (ICAM1; 147840) in human conjunctival epithelium is upregulated in patients with dry eyes associated with Sjogren syndrome. Tsubota et al. (1999) reported that this upregulation in Sjogren syndrome patients may be controlled by interferon-gamma (IFNG; 147570) through the activation of transcription factor NFKB (nuclear factor kappa-B; see 164011).
de Paiva et al. (2003) found that patients with keratitis sicca had irregular corneal surfaces when examined with computerized videokeratoscopy (CVK). The CVK regularity indices had both high sensitivity and specificity and had the potential to be used as objective diagnostic indices for dry eye, as well as a means to evaluate the severity of the disease.
In a study of 16 Italian patients with Vogt-Koyanagi-Harada syndrome (an autoimmune-mediated meningoencephalitis with panuveitis) and 16 controls with diffuse non-VKH uveitis, Pezzi et al. (2004) found that the incidence of keratoconjunctivitis sicca was higher in the patients with VKH syndrome than in the controls. Two patients satisfied the criteria for Sjogren syndrome and 2 others had scintigraphy indicative of salivary gland involvement. The authors concluded that an association between these 2 autoimmune disorders was suggested by the low incidence of VKH syndrome in Italy and might be related to HLA DR4.
Goransson et al. (2006) detected clinically significant peripheral neuropathy in 17 (27%) of 62 patients with primary Sjogren syndrome. Nerve conduction studies were abnormal in 34 (55%) patients; 19 (31%) had motor neuropathy, 8 (13%) had sensory neuropathy, and 7 (11%) had sensorimotor neuropathy. The predominant neuropathic process was demyelinating.
Mathews et al. (2015) reported the findings in a consecutive case series of 163 patients (149 women and 14 men) with primary Sjogren syndrome evaluated between 2007 and 2013. On initial presentation, men were a decade older (61 vs 50 years) and were less likely than women to have a prior diagnosis of the disorder. The majority of men (92%) reported dry eye upon presentation, although less chronic compared to women (5.9 vs 10.8 years). Men were more likely to present with serious ocular complications, including corneal melting/perforation, than women (43% vs 11%) and to have more extraglandular systemic complications such as vasculitis and interstitial nephritis (64% vs 40%). Men were also more likely to be negative for anti-SSA/Ro, anti-SSB/La, and antinuclear antibodies than women (36% vs 11%). Mathews et al. (2015) suggested that physicians should have a lower threshold to test for Sjogren syndrome in men.
Biochemical FeaturesPisella et al. (2000) reported that a significant increase of HLA-DR and ICAM1 expression by epithelial cells was consistently found in patients with keratoconjunctivitis sicca (Sjogren syndrome) compared with expression in normal eyes. These 2 markers were well correlated with each other and correlated inversely with tear break-up time and tear production as measured by the Schirmer test. The percentage of conjunctival goblet cells was significantly decreased in dry eye patients with a significant negative correlation with both HLA-DR and ICAM1 markers.
Clinical ManagementKunert et al. (2002) found that treatment of dry eyes due to Sjogren syndrome with cyclosporine A ophthalmic emulsion resulted in an increase in goblet cell numbers. The authors concluded that reducing ocular surface inflammation may have had a beneficial effect on the proliferative activity of the epithelium.
PathogenesisZoukhri and Kublin (2001) studied acetylcholine release and protein secretion from nerves of a mouse model of Sjogren syndrome. They concluded that activation of nerves of lacrimal and salivary glands infiltrated with lymphocytes does not increase acetylcholine release, which thus results in impaired secretion from these glands.
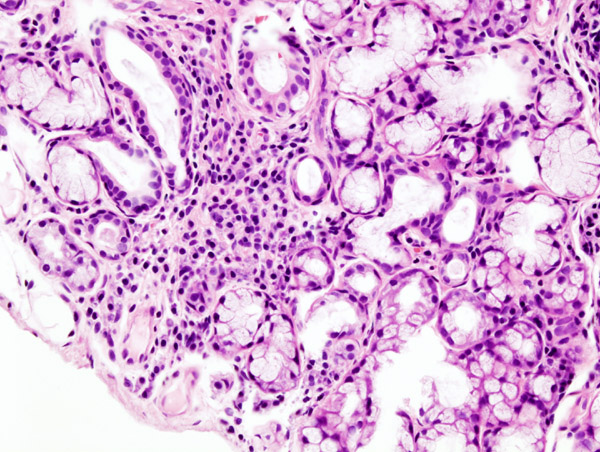
Tsubota et al. (2001) examined the distribution of aquaporin-5 (AQP5; 600442) in lacrimal gland biopsy specimens. Healthy controls and patients with either Mikulicz disease or non-Sjogren syndrome dry eye had the expected apical distribution of AQP5 in lacrimal acinar cells. Patients with Sjogren syndrome, however, had diffuse cytoplasmic staining for AQP5, with almost no labeling at the apical membrane. Tsubota et al. (2001) concluded that there is a selective defect in lacrimal gland AQP5 trafficking in Sjogren syndrome that might contribute to decreased lacrimation and dry eye in these patients.
Molecular GeneticsGottenberg et al. (2003) compared 149 patients fulfilling the American-European Consensus Group criteria for Sjogren syndrome to 222 controls and confirmed the association of Sjogren syndrome with HLA alleles DRB1*03 (see HLA-DRB1; 142857) and DQB1*02 (see HLA-DQB1; 604305). They found, however, that the association was restricted to patients with anti-SSA (see 109092 and 600063) and/or anti-SSB (see 109090) antibodies. The absence of a difference in disease severity between patients with anti-SSA and those with anti-SSA and anti-SSB antibodies, together with a high frequency of HLA-DRB1*03 in the latter group, suggested to the authors that HLA alleles predispose to autoantibody secretion but are not associated with clinical outcome.
Animal ModelThe nonobese diabetic (NOD) mouse, in which loss of salivary secretory function develops spontaneously, is not only the best model for spontaneous type 1 diabetes (222100), but also for Sjogren syndrome. ICA69 (147625) is expressed in salivary and lacrimal glands. In NOD mice, Winer et al. (2002) found that disruption of the Ica69 gene prevented lacrimal gland disease and greatly reduced salivary gland disease. These animals developed type 1 diabetes with slight delay but at much the same incidence as wildtype animals, assigning a facultative rather than obligate role to ICA69 in the development of diabetes.
Li et al. (2004) observed that Id3 (600277) -/- mice had difficulty maintaining fully opened eyelids beginning at 6 months and progressing with age. Histologic and electron microscopic analysis of mutant mice revealed lymphocytic infiltration in the lachrymal and salivary glands in the absence of infection, and the CD4 (186940) and CD8 (see 186910) T cells and B cells in the infiltrates expressed both Ifng and Il4 (147780). Id3 -/- mice showed reduced tear and saliva secretion, suggesting a disease similar to Sjogren syndrome. ELISA analysis detected both anti-SSA and anti-SSB autoantibodies in Id3 -/- mice after 1 year of age. Bone marrow transplant experiments showed that the phenotype was mediated by hemopoietic cells, and adoptive transfer analysis attributed a dominant role to Id3 -/- T lymphocytes. Elimination of T cells and neonatal thymectomy demonstrated that the tear and saliva secretion defect required sustained production of thymic T cells. Li et al. (2004) concluded that ID3-mediated T-cell development is connected to autoimmune disease, and they proposed that the Id3 -/- mouse is a model for primary Sjogren syndrome.
Oak et al. (2006) crossed mice with a floxed Pik3r1 (171833) allele and a null Pik3r2 (603157) allele with Lck (153390)-Cre transgenic mice to generate a strain in which class IA Pi3k expression and function were essentially abrogated in T cells beginning at the double-negative stage. Histopathologic analysis of these mice showed development of organ-specific autoimmunity resembling Sjogren syndrome. By 3 to 8 months of age, mutant mice developed corneal opacity and eye lesions due to irritation and constant scratching. Mutant mice showed marked lymphocytic infiltration of lacrimal glands and serum antinuclear and anti-Ssa antibodies, but no kidney pathology. Cd4-positive T cells, which were the predominant infiltrating cells in lacrimal glands of mutant mice, exhibited aberrant differentiation in vitro. Oak et al. (2006) concluded that impaired class IA PI3K signaling in T cells can lead to organ-specific autoimmunity, and they proposed that class IA Pi3k-deficient mice manifest the cardinal features of human primary Sjogren syndrome.