Merrf
MERRF (Myoclonic Epilepsy with Ragged Red Fibers) syndrome is a mitochondrial encephalomyopathy characterized by myoclonic seizures.
Epidemiology
The prevalence in the general population of Europe has been estimated at 0.9 in 100 000, but the disease seems to be more common in the USA.
Clinical description
Patients usually present during adolescence or early adulthood with myoclonic epilepsy, sometimes with neurosensory deafness, optic atrophy, short stature or peripheral neuropathy. A few cases have been associated with lipomatosis, cardiomyopathy, pigmentary retinopathy, ophthalmoparesis and/or pyramidal signs. The disease is progressive with worsening of the epilepsy and onset of additional symptoms including ataxia, deafness, muscle weakness, and dementia. Magnetic resonance imaging of the brain may show cortical atrophy, basal ganglia calcifications and leucodystrophy. Clinical manifestations may vary greatly between patients from the same family and between families.
Etiology
MERRF syndrome is caused by mutations in the mitochondrial DNA. Over 80% of individuals with MERRF syndrome carry the 8344A>G mutation in the lysine transfer RNA (tRNA Lys) gene (MTTK). Other mutations have been found in other transfer RNA genes or in the MTND5 gene. They may be associated with MERRF/MELAS overlap syndrome, in which affected individuals also suffer from stroke-like episodes.
Diagnostic methods
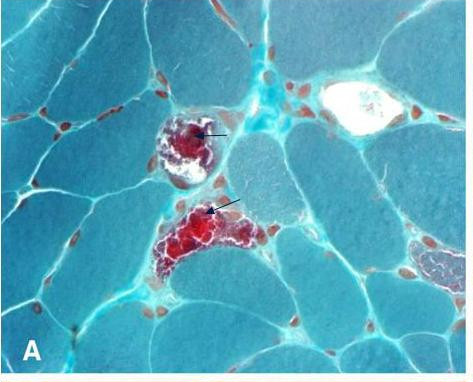
The diagnosis of MERRF syndrome relies on the demonstration of abnormal lactate accumulation in blood or, more often, in the cerebrospinal fluid, and on the muscle biopsy, which reveals the presence of cytochrome c oxidase negative muscle fibers and ragged red fibers. Biochemical analysis of muscle often shows cytochrome c oxidase deficiency or combined respiratory chain defect. Heteroplasmy (i.e. coexistence of the mutant form with a residual population of wild type mitochondrial DNA) should be taken into account during identification of the causal. The proportion of the mutation may differ considerably between tissues. However, in MERRF syndrome, this proportion is most often very high (above 90%) in every tissue and the mutation may therefore be investigated in blood.
Antenatal diagnosis
The possibility of heterogeneous proportions of the mutation between tissues theoretically hampers prenatal diagnosis.
Genetic counseling
The heteroplasmy makes genetic counseling very arduous in MERRF syndrome. Mitochondrial DNA mutations are transmitted through maternal inheritance. An affected man cannot transmit the disease. The mutation will be transmitted along the maternal lineage but its proportion is essentially unpredictable. Although higher proportions of the mutation in the blood of the mother result in a higher risk of having a child with severe phenotype, there are many examples of extreme segregation of the mutation from mother to child, which prevent efficient genetic counseling at an individual level.
Management and treatment
As with other mitochondrial encephalomyopathies, there is no specific treatment for MERRF syndrome. Seizures can be treated with conventional anticonvulsant therapies but valporic acid should be administered with care and in association with L-carnitine. In the absence of proper clinical trials, it is difficult to evaluate the effect of proposed supportive treatment such as coenzyme Q10 and its analogue idebenone, carnitine, etc.
Prognosis
The prognosis for patients with MERRF syndrome is globally poor because of the progressive nature of the disease. However, the severity varies greatly and some patients, mainly those with non-cerebral presenting symptoms, may have a prolonged survival with relatively little handicap.