Isovaleric Acidemia
A rare, autosomal recessive, organic aciduria that is characterized by variable clinical presentation ranging from acute neonatal onset of metabolic decompensation to later onset of chronic, non-specific manifestations including failure to thrive and/or developmental delay. All patients are prone to intermittent, acute metabolic decompensation. During metabolic episodes, urine analysis demonstrates elevated isovaleric acid derivatives.
Epidemiology
Accurate data on the prevalence is not readily available. Best estimates come from newborn screening studies that estimate prevalence at birth between 1/50,000-150,000.
Clinical description
Patients present along a spectrum. Acute, neonatal presentation is characterized by onset in the first two weeks of life with vomiting, seizures, and lethargy, progressing to coma. Metabolic acidosis with an increased anion gap is apparent on laboratory evaluation. Hyperammonemia may occur. Later onset is relatively non-specific with failure to thrive and/or developmental delay. Patients who survived an early acute presentation are subsequently indistinguishable from those with the chronic phenotype. All patients are prone to intermittent acute episodes of decompensation with minor illnesses. Childhood onset metabolic acidosis is typically brought on by prolonged fasting, increased intake of protein-rich food or infections, and can be fatal if not treated immediately. The characteristic smell of isovaleric acid may be present, and is likened to sweaty feet/body sweat. Though severe developmental delay and neurologic sequelae are present in some patients, they are likely related to severe biochemical presentations.
Etiology
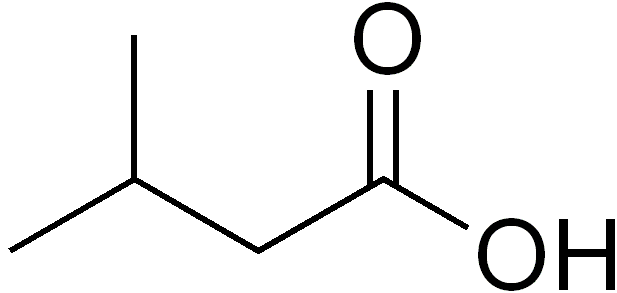
Isovaleric academia (IVA) is caused by mutations in the IVD gene (15q15.1) encoding the enzyme isovaleryl-CoA dehydrogenase (IVDH) resulting in accumulation of isovaleric acid and its derivatives. Asymptomatic patients with specific mutations have been reported, especially when identified through newborn screening.
Diagnostic methods
Where implemented, diagnosis is through newborn blood spot screening. Otherwise, in symptomatic individuals diagnosis is suspected based on the clinical presentation. Metabolite or molecular genetic testing confirms diagnosis. Characteristic urine metabolites includes elevated N‐isovalerylglycine, N‐isovalerylcarnitine and 3‐hydroxyisovaleric acid. Isovalerylcarnitine (''C5 carnitine'') is elevated in blood. The urine organic acids may normalize when a patient is well.
Differential diagnosis
In acutely decompensating patients, the differential diagnosis includes other organic acidemias (including lactic acidosis), urea cycle defects, and sepsis. On newborn screening, ''C5-carnitine'' may also indicated 2-methylbutyryl-CoA dehydrogenase deficiency; urine organic acids readily differential the two disorders as does molecular testing.
Antenatal diagnosis
Prenatal genetic testing is possible when the mutation of a proband has previously been determined.
Genetic counseling
The pattern of inheritance is autosomal recessive; genetic counseling is recommended for affected families. The risk of disease transmission at each pregnancy is 25% when the parents are proven or obligate carriers.
Management and treatment
Lifelong management is with a low protein diet. Children diagnosed with IVA should be referred to a metabolic dietician who can tailor the diet to support normal growth and development. Supplementing with artificial protein restricted in leucine may be required. L-carnitine and glycine may be prescribed to clear excess isovaleric acid. Emergency treatment in times of metabolic stress (including illness and fasting) is with an anabolic diet. Reducing, but not eliminating, natural protein in the diet for 12-24 hours may help, but only if additional other calories can be given to promote anabolism.
Prognosis
Prognosis for patients diagnosed by newborn screening is excellent with the potential for normal neurodevelopmental outcome with appropriate metabolic management. Patients who present symptomatically can have significant neurologic sequelae including neurodevelopmental delay, especially if acidosis and hyperammonemia are severe.