Granulomatous Disease, Chronic, Autosomal Recessive, Cytochrome B-Positive, Type Ii
A number sign (#) is used with this entry because autosomal recessive cytochrome b-positive chronic granulomatous disease (CGD) type II is caused by homozygous or compound heterozygous mutation in the NCF2 gene (608515), which encodes the p67-phox (phagocyte oxidase) protein, on chromosome 1q25.
A more common form of autosomal cytochrome b-positive chronic granulomatous disease, type I (233700), is caused by mutation in the NCF1 gene (608512), which encodes the p47-phox protein.
For a phenotypic description of chronic granulomatous disease, see the well-established X-linked recessive cytochrome b-negative form (CGD; 306400).
Clinical FeaturesNunoi et al. (1995) reported a Japanese patient with p67-deficient CGD confirmed by mutation in the NCF2 gene (608515.0001). He was a 19-year-old man whose first episode of infection was at age 3 when he had perianal abscess, liver abscess, severe lung abscess, pneumonia with Aspergillus infection, and severe spinal Aspergillus osteomyelitis. Recurrent infections occurred at ages 4, 6, 11, 15, and 19 years. His clinical course was worse than that of 4 other patients with p67-phox deficiency found in Japan. CGD was diagnosed by no reduction of nitroblue tetrazolium in neutrophils. Nunoi et al. (1995) stated that only 5 patients with p67-phox deficiency had been reported in the United States and Europe, whereas in Japan, although such CGD patients are also rare, they accounted for 7 of 90 CGD patients.
Patino et al. (1999) reported several girls with p67-phox-deficient CGD confirmed by mutations in the NCF2 gene (608515.0003-608515.0006). In an 8-year-old Hispanic girl, the diagnosis of CGD had been made at age 8 months when the patient presented with a right upper lobe pneumonia caused by Serratia marcescens. A 10-year-old girl, born of first-cousin parents native to Jordan, had recurrent abscesses caused by gram-negative bacteria in the first year of life. At the age of 5 years, she had developed inflammatory bowel disease. The diagnosis of CGD was made on the basis of absent NBT reduction and O2(-) production by her PMA-stimulated neutrophils. Deficiency of p67-phox was demonstrated by Western blot analysis. Her sister, aged 2 years, also showed the genetic defect but had not yet developed serious illness or required hospitalization. In a girl with p67-phox-deficient CGD who was 4 years old at the time of her death in Mexico, the diagnosis of CGD was suspected when she presented with skin abscesses containing Enterobacter and Klebsiella and confirmed by a negative NBT test and absent O2(-) production. In her last year of life she was treated successfully for Aspergillus fumigatus pneumonia; however, a few months later, she presented with a severe respiratory infection characterized by necrotizing granulomas and acid-fast bacteria.
DiagnosisPrenatal Diagnosis
Kenney et al. (1993) reported a 9-year-old girl with CGD due to deficiency of p67-phox who was homozygous for a RFLP disease marker in the NCF2 gene. Her phenotypically normal mother was also homozygous for the marker, whereas the father and 2 brothers were heterozygous. A fetus was shown to be heterozygous as well, showing that it had inherited at least 1 normal NCF2 gene from the father, predicting a normal phenotype. Cord blood samples at birth showed normal oxidative function.
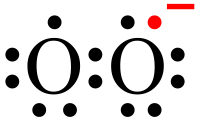
PathogenesisVolpp et al. (1988) raised a polyclonal antiserum that recognized the 47-kD and 67-kD proteins and showed that the neutrophils from patients with 2 different forms of autosomal CGD lacked either the 47- or the 67-kD protein. A deficiency of the 47-kD protein is more frequent than that of the 67-kD protein.
Clinical ManagementLiese et al. (2000) evaluated the effect of antibiotic and antifungal long-term prophylaxis on the prognosis of CGD in 39 patients with different subtypes, both X-linked and autosomal recessive. Antibiotic prophylaxis with TMP-SMX significantly decreased the incidence of severe infections in patients with complete loss of cytochrome b activity but had no significant effect in patients with the other subtypes. Eight of the patients with complete absence of cytochrome b activity were also given itraconazole, and none developed fungal infections over 15.5 patient-years, whereas patients of all subtypes who received only antibiotics showed an increase in severe fungal infections. The different subtypes were also analyzed for age at diagnosis, age at first infection, and long-term survival.
Molecular GeneticsClark et al. (1989) concluded that the autosomal form of CGD due to deficiency of NCF1 represents about 33% of all cases of CGD; the autosomal form due to deficiency of NCF2 represents about 5% of cases.
In a Japanese patient with p67-deficient CGD, Nunoi et al. (1995) identified a mutation in the NCF2 gene (608515.0001).