Hypoparathyroidism-Retardation-Dysmorphism Syndrome
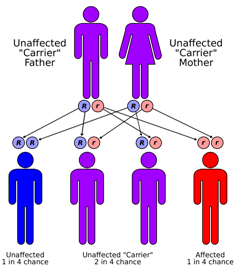
A number sign (#) is used with this entry because of evidence that hypoparathyroidism-retardation-dysmorphism syndrome (HRDS) is caused by homozygous or compound heterozygous mutation in the TBCE gene (604934) on chromosome 1q42.
Biallelic mutation in the TBCE gene can also cause Kenny-Caffey syndrome (KCS1; 244460) and progressive encephalopathy with amyotrophy and optic atrophy (PEAMO; 617207).
DescriptionHRDS is an autosomal recessive multisystem disorder characterized by intrauterine and postnatal growth retardation, infantile-onset hypoparathyroidism that can result in severe hypocalcemic seizures, dysmorphic facial features, and developmental delay (summary by Padidela et al., 2009 and Ratbi et al., 2015).
Clinical FeaturesCongenital hypoparathyroidism in association with growth and mental retardation and seizures has been reported from the Middle East in children of consanguineous parents (Sanjad et al. (1988), Richardson and Kirk, 1990; Sanjad et al., 1991; Kalam and Hafeez, 1992). The first report, an abstract, was by Sanjad et al. (1988). The syndrome is sometimes known as the Sanjad-Sakati syndrome. Richardson and Kirk (1990) described the cases of 4 boys and 4 girls with this syndrome who were the products of 7 consanguineous marriages, 2 of the patients being brothers. In the remaining 6 families, a further 4 children had affected sibs who had died in infancy. The height, weight, and head circumference scores in all 8 children were less than -2 SD from the mean for their ages. Children had identical facies with deep-set eyes, depressed nasal bridge with beaked nose, long philtrum, thin upper lip, micrognathia, and large, floppy earlobes. Medullary stenosis and other skeletal defects were found in 7 of 8 children. Reduced numbers of T-cell subsets were found in 4 of 4 tested. From Saudi Arabia, Sanjad et al. (1991) described 12 affected infants, 6 girls and 6 boys, who were seen over a 3-year period. All had severe intrauterine growth retardation and postnatal growth retardation. Symptoms had occurred in the newborn period in 9 of them. The hypocalcemia was associated with hyperphosphatemia and very low concentrations of immunoreactive parathyroid hormone. None of the babies suffered from congenital heart disease. Cell-mediated immunity, measured in 5 patients, was normal. The propositus of Richardson and Kirk (1990) was born in the United Kingdom of first-cousin parents from Qatar. The other children were described simply as being 'of Middle-Eastern origin.' Although some features suggested DiGeorge syndrome (188400) or the Kenny-Caffey syndrome (127000), the conclusion was that it indeed represents a separate entity.
Marsden et al. (1994) described an affected 5-year-old Saudi Arabian girl born of consanguineous parents. Parathyroid hormone was undetectable, although her renal response to the infused hormone was normal. Growth hormone levels remained subnormal following arginine and L-DOPA stimulation. After clonidine, the growth hormone level rose to 15 ng/ml at 120 min. Treatment with human growth hormone produced a marked increase in height and weight. Marsden et al. (1994) suggested that regulation of parathyroid hormone may be controlled by the hypothalamus.
Hershkovitz et al. (1995) described 6 children of Arab origin with the syndrome of congenital hypoparathyroidism, severe growth retardation, developmental delay, and dysmorphism (microcephaly, facial and dental anomalies, and small hands and feet). Bone age was markedly retarded. Neither immunologic nor chromosomal abnormalities were found. Serum levels of insulin-like growth factor-1 (147440) measured in 2 patients were abnormally low. In an addendum, Hershkovitz et al. (1995) stated that, during the preparation of the manuscript, another 2 patients were born, bringing to 3 the number of affected sibs in each of 2 families. Both of the newly born patients had low birth weight, dysmorphic features similar to those in the other patients, and asymptomatic hypocalcemia that appeared a few days after birth. Parental consanguinity was evident in 3 families. In the first 6 patients, 3 were female and 3 were male. It was thought that the disorder did not conform to described forms of familial hypoparathyroidism (146200 and 307700) or to DiGeorge syndrome (188400); however, the ethnicity and clinical features indicated that it is the same disorder as that reported from Saudi Arabia.
Padidela et al. (2009) reported 6 children from 4 unrelated Middle Eastern families with HRDS confirmed by genetic analysis. All were homozygous for the founder 12-bp deletion in the TBCE gene (604934.0001). Brain imaging of all children showed hypoplasia of the anterior pituitary, infundibulum, and corpus callosum, as well as decreased white matter volume, delayed myelination, and dilated lateral ventricles. Four of five children tested had low levels of growth hormone and subnormal cortisol responses to glucagon, and all 6 had low plasma IGF1 (147440). All 3 males had clinical features suggestive of hypogonadotropic hypogonadism, although testosterone responses to HCG were satisfactory. Padidela et al. (2009) suggested that TBCE may play a role in development of the anterior pituitary, corpus callosum, and white matter, in addition to the parathyroid glands.
Ratbi et al. (2015) reported a female infant, born of consanguineous Moroccan parents, with HRDS. She had intrauterine growth retardation, axial hypotonia, and developed seizures associated with hypocalcemia on the second day of life. Phosphate was increased and parathyroid hormone was severely decreased. Dysmorphic features included deep-set small eyes, depressed nasal bridge with a beaked nose, long philtrum, thin upper lip, micrognathia, and large floppy earlobes. She had no cardiac or skeletal manifestations and died at age 3 months from complications of hypoparathyroidism.
MappingParvari et al. (1998) used homozygosity and linkage disequilibrium to map the gene for this disorder, which they symbolized HRD for 'hypoparathyroidism with growth retardation, developmental delay, and dysmorphism,' to a 1-cM interval on 1q42-q43.
Kelly et al. (2000) reported linkage analysis in 3 consanguineous Saudi Arabian families with Sanjad-Sakati syndrome. A maximum lod score of 4.12 was obtained at D1S235, and analysis of flanking markers D1S1656 and D1S2678 suggested a candidate region of 1 cM. Kelly et al. (2000) noted that Kenny-Caffey syndrome type 1 (244460) maps to the same region and suggested that these were likely to be allelic disorders, if not the same condition.
Molecular GeneticsIn all patients of Middle Eastern descent with HRDS, Parvari et al. (2002) identified the same homozygous 12-bp deletion in the TBCE gene (604934.0001). Parvari et al. (2002) found that this homozygous deletion also caused autosomal recessive Kenny-Caffey syndrome.
In a female infant, born of consanguineous Moroccan parents, with HRDS, Ratbi et al. (2015) identified homozygosity for the 12-bp deletion (c.155_166del12) that was previously found only in patients of Middle Eastern descent. The findings were consistent with the history of Arab migration to Morocco with the expansion of Islam to North Africa in the 7th century.
Population GeneticsHershkovitz (1996) stated that the Bedouin in the Negev (southern part of Israel) came to that region 400 to 500 years ago from the western part of Arabia; thus, a relationship of the Israeli Arab patients to the Saudi patients is possible.
HeterogeneityCourtens et al. (2006) reported a girl with congenital hypoparathyroidism, seizures, mild developmental delay, macrocephaly, and facial dysmorphism compatible with HRD syndrome. The authors noted that the absence of severe developmental delay and microcephaly differentiated this patient from those previously reported with HRD. Mutation analysis revealed no mutations in the TBCE gene, and normal TBCE protein and alpha-tubulin immunostaining were observed in a lymphoblastoid cell line derived from the patient. A de novo microduplication on chromosome 4q35 was detected by microarray analyses, but could not be confirmed by additional studies. Courtens et al. (2006) concluded that a second gene locus for this disorder seems probable.