Schilder Disease
Schilder's disease is a progressive demyelinating disorder of the central nervous system.
Epidemiology
Less than 20 sporadic cases (predominantly males) have been reported so far.
Clinical description
The onset is usually in childhood (age 5-14 years). The disease often occurs shortly after an infectious illness and may manifest with headache, malaise and fever. Variable neurological abnormalities progressively develop and include personality changes, poor attention, dementia, aphasia, headache, vomiting, tremor, seizures, balance instability, incontinence, muscle weakness. Deafness, paralysis of eye movements, nystagmus, optic neuritis and optic atrophy are common. Malnutrition and cachexia are reported in the later chronic stages of illness. Schilder's disease is considered as a variant or borderline form of multiple sclerosis.
Etiology
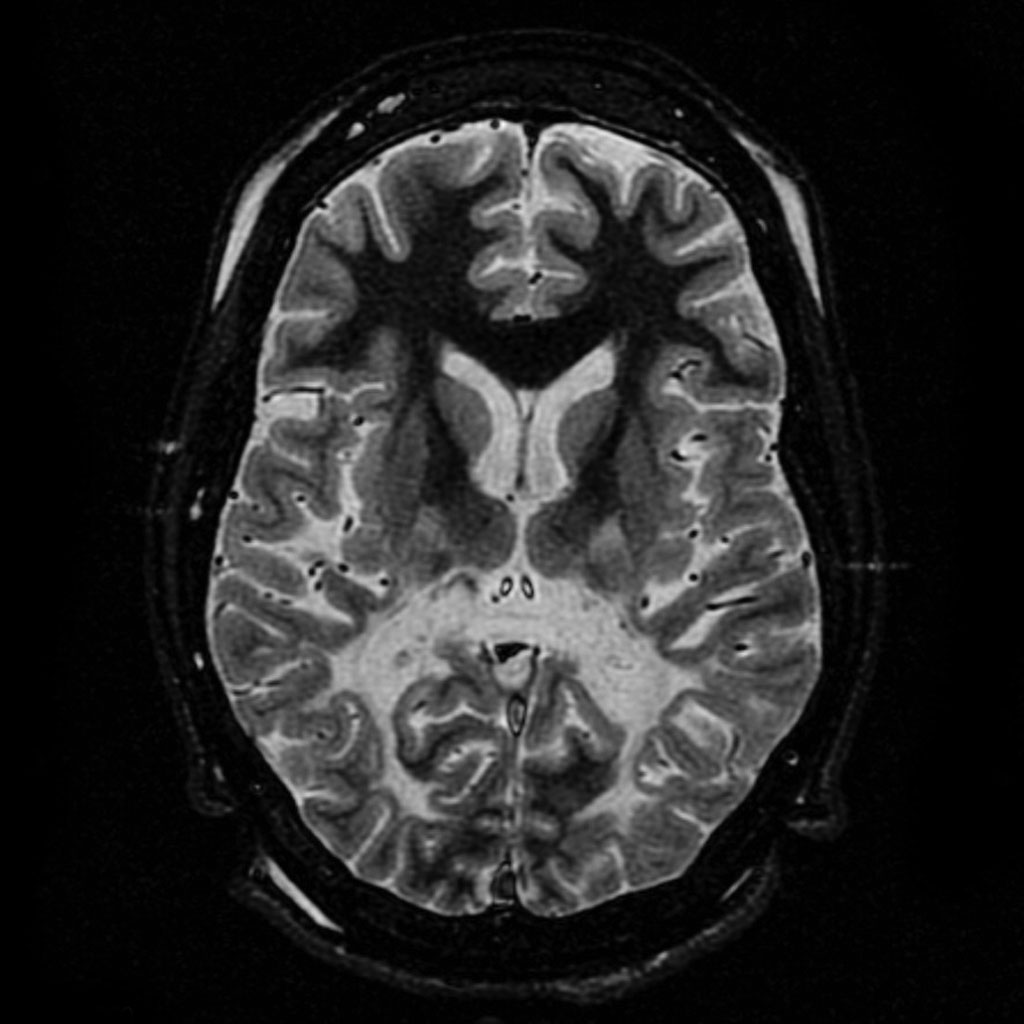
Pathologically, it is characterized by bilateral widespread demyelination of the brain hemispheres with varying degrees of axonal injury. Etiology remains unclear.
Diagnostic methods
Diagnosis is based on sequential neuroimaging (consistent with subacute or chronic myelinoclastic diffuse sclerosis) and electroencephalographic studies.
Differential diagnosis
Differential diagnosis includes a wide range of neurodegenerative disorders such as multiple sclerosis, acute disseminated encephalomyelitis, subacute sclerosing panencephalitis, progressive rubella panencephalitis, brucellosis, metachromatic leukoencephalopathy, Churg-Strauss disease, Wegener granulomatosis (see these terms). Schilder's disease often mimics intracranial neoplasm or abscess.
Management and treatment
Management is mainly symptomatic and supportive (physiotherapy, occupational therapy, nutritional support in the later stages). Corticosteroids have been shown effective in some patients. Additional treatments include beta-interferon and/or immunosuppressive drugs.
Prognosis
Prognosis of Schilder's disease is variable. The clinical course is usually progressive, but significant improvement and remissions have also been described. Survival has been reported to be less than ten years after the onset. Patients with a good response to corticosteroids and those with smaller lesions may have a better prognosis.