Pseudomyxoma Peritonei
Pseudomyxoma peritonei is characterized by disseminated intra-peritoneal mucinous tumors and mucinous ascites in the abdomen and pelvis.
Epidemiology
Annual incidence is estimated at 1/1,000,000 with female predominance.
Clinical description
The disease is usually diagnosed after the age of 40. In 30 to 50% of cases, patients present with progressive abdominal distension (so-called ``jelly belly''). Diagnosis may follow discovery of an ovarian mass in women or recent development of inguinal hernia, appendicitis or intestinal occlusion. Other less common signs include abdominal pain, weight loss, urinary symptoms, constipation, vomiting, and dyspnea.
Etiology
In 90% of cases, the primary lesion is an appendiceal mucinous tumor, but ovarian mucinous tumors have been reported (7%) and, more rarely, mucinous tumors of the colon, stomach, pancreas, and urachus.
Diagnostic methods
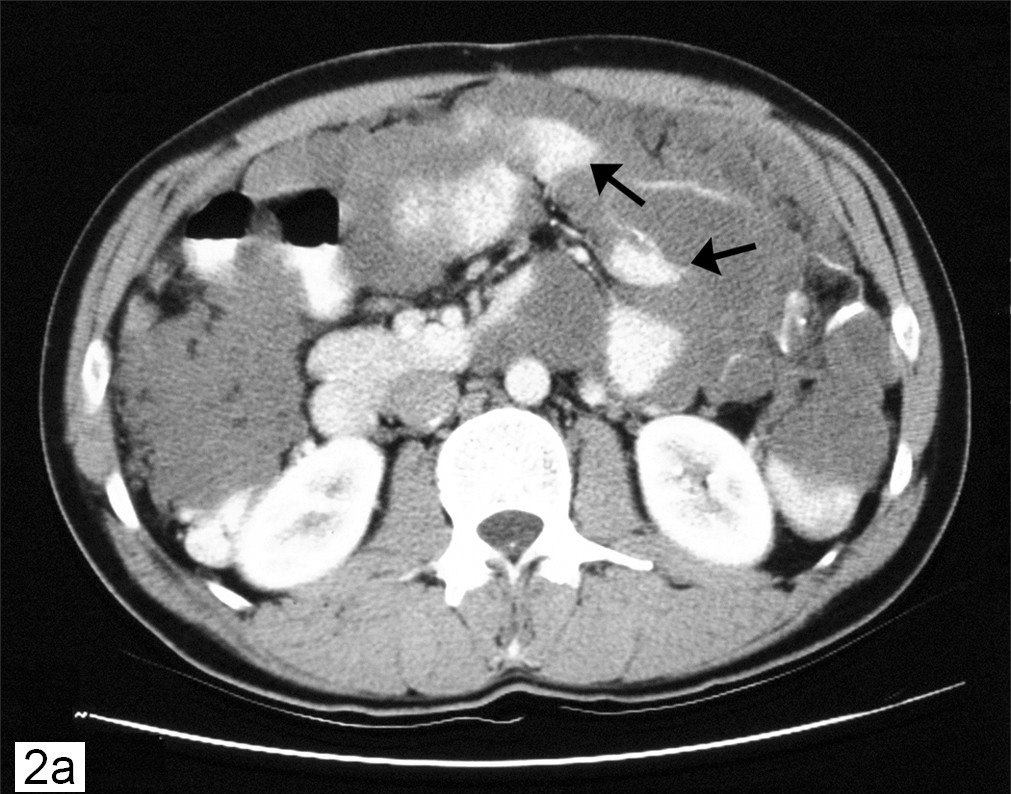
The diagnosis is based on chest-abdominal-pelvic computed tomography (CAP-CT) findings (revealing the characteristic compartmentalized distribution pattern of mucinous ascites) and on pathology (performed by two experts), while tumor markers (carcinoembryonic antigen and CA19-9) are relatively non-specific.
Differential diagnosis
The differential diagnosis includes secondary peritoneal carcinomatoses and other rare peritoneal tumors.
Management and treatment
Treatment strategies require a multidisciplinary approach and must be discussed by a panel of physicians in a specialized center. There are currently no validated recommendations on clinical management and no cytotoxic agents have been granted a European Marketing Authorization (MA) in this indication. Nonetheless, the best curative option appears to be complete cytoreductive surgery (visceral resections and peritonectomy procedures) combined with hyperthermic intraperitoneal chemotherapy (HIPEC) (off-label use), sometimes followed by intravenous chemotherapy (off-label use) which can only be considered in young patients with good general status.
Prognosis
Pseudomyxoma peritonei is slowly progressive but recurrence after complete tumor removal may occur. Following combined treatment (complete cytoreductive surgery and HIPEC), the 5-year survival rate reaches 70% for non-aggressive peritoneal pseudomyxoma in patients treated in a specialized center.