-
Sanjad-Sakati Syndrome
Wikipedia
Sanjad and Nadia Awni Sakati . [ citation needed ] References [ edit ] ^ Sanjad, S (1988). "Congenital hypoparathyroidism with dysmorphic features: a new syndrome. ... Pediatric Research . 23 : 271A. ^ Sanjad, S. A.; Sakati, N. A.; Abu-Osba, Y. K.; Kaddoura, R.; Milner, R. ... PMID 2001103 . ^ Hershkovitz, E.; Shalitin, S.; Levy, J.; Leiberman, E.; Weinshtock, A.; Varsano, I.; Gorodischer, R. ... Retrieved 2015-08-25 . ^ Parvari, R., Hershkovitz, E., Grossman, N., Gorodischer, R., Loeys, B., Zecic, A., Mortier, G., Gregory, S., Sharony, R., Kambouris, M., Sakati, N., Meyer, B.
-
Tinea Imbricata
Wikipedia
International Journal of Dermatology . 43 (7): 506–10. doi : 10.1111/j.1365-4632.2004.02171.x . PMID 15230889 . ^ Serjeantson S, Lawrence G (January 1977). "Autosomal recessive inheritance of susceptibility to tinea imbricata". ... PMC 1048596 . PMID 7218274 . ^ Lim S. P. R., Smith A. G. (2003). "Tinea corporis in a renal transplant recipient mimicking the concentric rings of tinea imbricata". ... CS1 maint: multiple names: authors list ( link ) ^ Verma S, Hay RJ (2015). "Topical steroid-induced tinea pseudoimbricata: a striking form of tinea incognito". ... Tinea pseudoimbricata caused by M. gypseum associated to crusted scabies.An Bras Dermatol. 2010 Jul-Aug;85(4):558-9.[English, Portuguese] ^ Verma S (2017). "Tinea pseudoimbricata" .
-
Efemp2-Related Cutis Laxa
Gene_reviews
Variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. ... Genes of Interest in the Differential Diagnosis of EFEMP2 -Related Cutis Laxa (ARCL1B) View in own window Gene(s) Disorder MOI Clinical Findings Comment CL Emphysema ID GI & GU malformation Cardiovascular ALDH18A1 ARCL3A (OMIM 219150) AR + - +++ - - ARCL3A is not assoc w/cardiovascular & pulmonary involvement.
-
Thiourea Tasting
Omim
The compounds carry the chemical group N-C=S, which is responsible for their characteristic bitter taste (Bartoshuk et al., 1994; Drewnowski and Rock, 1995). ... Distinct phenotypes were associated with specific haplotypes, which demonstrated that the TAS2R38 gene has a direct influence on PTC taste sensitivity, and that sequence variants at different sites interact with each other within the encoded gene product.
-
Hyperparathyroidism 1
Omim
In the proband and 2 affected members of a family with familial isolated hyperparathyroidism, Cetani et al. (2004) identified heterozygosity for a germline in the donor splice site of intron 1 of the CDC73 gene (607393.0010). ... INHERITANCE - Autosomal dominant ENDOCRINE FEATURES - Primary hyperparathyroidism LABORATORY ABNORMALITIES - Hypercalcemia - Primary chief cell hyperplasia MOLECULAR BASIS - Caused by mutation in the homolog of S cerevisiae cell division cycle protein-73 gene (CDC73, 607393.0004 ) ▲ Close
-
Hyperkalemic Periodic Paralysis
Wikipedia
Mutations have been found on the cytoplasmic loops between the S4 and S5 helices of domains II, III and IV, which are the binding sites of the inactivation gate. [3] [4] The pathological mechanism of SCN4A mutations in hyperkalemic periodic paralysis is complex, but explains the autosomal dominant and hyperkalemia-related aspects of the disease. [5] In patients with mutations in SCN4A, not all copies of the channel inactivate following the action potential. ... PMID 1659668 . S2CID 4372717 . ^ Bendahhou S, Cummins TR, Kula RW, Fu YH, Ptácek LJ (April 2002).
-
Invasive Candidiasis
Wikipedia
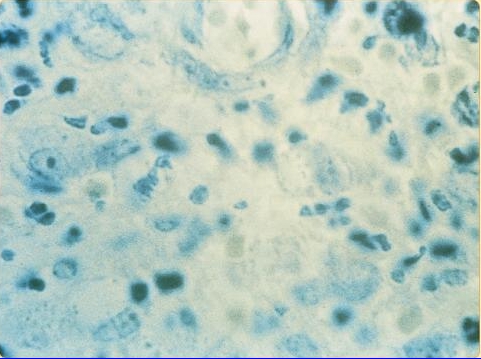
Emergent species [ edit ] Candida auris is an emerging multidrug-resistant yeast that can cause invasive candidiasis and is associated with high mortality. [6] It was first described in 2009. [6] Since then, C. auris infections, specifically fungemia, have been reported from South Korea, India, South Africa, Kuwait, Colombia, Venezuela, Pakistan, the United Kingdom and the United States. [6] The strains isolated in each region are genetically distinct, indicating that this species is emerging in different locations. [6] The reason for this pattern is unknown. [6] Risk factors [ edit ] Patients with the following conditions, treatments or situations are at increased risk for invasive candidiasis. [4] [2] [7] Critical illness Long-term intensive care unit stay Abdominal surgery (aggravated by anastomotic leakage or repeat laparotomies ) Immunosuppressive diseases Acute necrotizing pancreatitis Malignant hematologic disease Solid-organ transplantation Hematopoietic stem cell transplantation Solid- organ tumors Neonates (especially low birth weight and preterm infants) Broad-spectrum antibiotic treatment Central venous catheter Internal prosthetic device Total parenteral nutrition Hemodialysis Glucocorticoid use Chemotherapy Noninvasive Candida colonization (particularly if multifocal) Transmission [ edit ] Invasive candidiasis is a nosocomial infection with the majority of cases associated with hospital stays. [4] Diagnosis [ edit ] Because many Candida species are part of the human microbiota , their presence in the mouth, the vagina, sputum, urine, stool, or skin is not definitive evidence for invasive candidiasis. [2] Positive culture of Candida species from normally sterile sites, such as blood, cerebrospinal fluid , pericardium , pericardial fluid , or biopsied tissue , is definitive evidence of invasive candidiasis. [2] Diagnosis by culturing allows subsequent susceptibility testing of causative species. [8] [7] Sensitivity of blood culture is far from ideal, with a sensitivity reported to be between 21 and 71%. [7] Additionally, whereas blood culture can establish a diagnosis during fungemia , the blood may test negative for deep-seated infections because candida may have been successfully cleared from the blood. [7] Diagnosis of invasive candidiasis is supported by histopathologic evidence (for example, yeast cells or hyphae ) observed in specimens of affected tissues. [2] Additionally, elevated serum β-glucan can demonstrate invasive candidiasis while a negative test suggests a low likelihood of systemic infection. [9] [2] The emergence of multidrug-resistant C. auris as a cause of invasive candidiasis has necessitated additional testing in some settings. [6] C. auris -caused invasive candidiasis is associated with high mortality. [6] Many C. auris isolates have been found to be resistant to one or more of the three major antifungal classes (azoles, echinocandins, and polyenes) with some resistant to all three classes – severely limiting treatment options. [6] Biochemical-based tests currently used in many laboratories to identify fungi, including API 20C AUX and VITEK-2 , cannot differentiate C. auris from related species (for example, C. auris can be identified as C. haemulonii ). [6] Therefore, the Centers for Disease Control and Prevention recommends using a diagnostic method based on matrix-assisted laser desorption/ionization-time of flight mass spectrometry or a molecular method based on sequencing the D1-D2 region of the 28s rDNA to identify C. auris in settings where it may be present. [6] Prevention [ edit ] Preventive antifungal treatment is supported by studies, but only for specific high-risk groups in intensive care units with conditions that put them at high risk for the disease. [7] For example, one group would be patients recovering from abdominal surgery that may have gastrointestinal perforations or anastomotic leakage . [7] Antifungal prophylaxis can reduce the incidence of fungemia by approximately 50%, but has not been shown to improve survival. [7] A major challenge limiting the number of patients receiving prophylaxis to only those that can potentially benefit, thereby avoiding the creation of selective pressure that can lead to the emergence of resistance . [7] Treatment [ edit ] Antifungals are used for treatment with the specific type and dose depending on the patient's age, immune status, and specifics of the infection. ... Retrieved 2017-04-06 . ^ a b c d e f g h i j k l m n o p q r s Kullberg, Bart Jan; Arendrup, Maiken C. (2015-10-08).
-
Vaginal Cancer
Wikipedia
This article incorporates text from this source, which is in the public domain . ^ Shobeiri, S. Abbas; Rostaminia, Ghazaleh; White, Dena; Quiroz, Lieschen H.; Nihira, Mikio A. (2013-08-01). ... Retrieved 2017-12-13 . ^ "List of Classifications by cancer sites with sufficient or limited evidence in humans, Volumes 1 to 120 a" .
- Granuloma Inguinale Wikipedia
-
Pathological Lying
Wikipedia
L. L.; Patrick, C. J.; Lilienfeld, S. O. (2011). "Psychopathic Personality: Bridging the Gap Between Scientific Evidence and Public Policy" . ... Dependence Concepts Physical dependence Psychological dependence Withdrawal Disorders Drugs Alcoholism Amphetamine Barbiturate Benzodiazepine Caffeine Cannabis Cocaine Nicotine Opioid Non-drug stimuli Tanning dependence Treatment and management Detoxification Alcohol detoxification Drug detoxification Behavioral therapies Cognitive behavioral therapy Relapse prevention Contingency management Community reinforcement approach and family training Motivational enhancement therapy Motivational interviewing Motivational therapy Physical exercise Treatment programs Drug rehab Residential treatment center Heroin-assisted treatment Intensive outpatient program Methadone maintenance Smoking cessation Nicotine replacement therapy Tobacco cessation clinics in India Twelve-step program Support groups Addiction recovery groups List of twelve-step groups Harm reduction Category:Harm reduction Drug checking Reagent testing Low-threshold treatment programs Managed alcohol program Moderation Management Needle exchange program Responsible drug use Stimulant maintenance Supervised injection site Tobacco harm reduction See also Addiction medicine Allen Carr Category:Addiction Discrimination against drug addicts Dopamine dysregulation syndrome Cognitive control Inhibitory control Motivational salience Incentive salience Sober companion Category v t e Psychopathy Contexts In fiction In the workplace Characteristics Anti-social behaviour Bold Callous Diminished empathy Disinhibited Grandiose Impulsive Lack of guilt Manipulative Pathological lying Remorseless Shallow affect Superficially charming Related topics Antisocial personality disorder Conduct disorder Dark triad Flying monkeys History of psychopathy Juvenile delinquency Machiavellianism Macdonald triad Narcissism Psychopathic Personality Inventory Psychopathy Checklist Sadistic personality disorder Sexual sadism disorder Sociopathy Notable theorists Hervey M.
-
Drooling
Wikipedia
PMID 26212726 . ^ Weiss-Lambrou, R.; Tetreault, S.; Dudley, J. (1989). "The relationship between oral sensation and drooling in persons with cerebral palsy" . ... External links [ edit ] Classification D ICD - 10 : K11.7 ICD - 9-CM : 527.7 MeSH : D012798 DiseasesDB : 20764 External resources MedlinePlus : 003048 Look up drool in Wiktionary, the free dictionary. NIH site on drooling v t e Oral and maxillofacial pathology Lips Cheilitis Actinic Angular Plasma cell Cleft lip Congenital lip pit Eclabium Herpes labialis Macrocheilia Microcheilia Nasolabial cyst Sun poisoning Trumpeter's wart Tongue Ankyloglossia Black hairy tongue Caviar tongue Crenated tongue Cunnilingus tongue Fissured tongue Foliate papillitis Glossitis Geographic tongue Median rhomboid glossitis Transient lingual papillitis Glossoptosis Hypoglossia Lingual thyroid Macroglossia Microglossia Rhabdomyoma Palate Bednar's aphthae Cleft palate High-arched palate Palatal cysts of the newborn Inflammatory papillary hyperplasia Stomatitis nicotina Torus palatinus Oral mucosa – Lining of mouth Amalgam tattoo Angina bullosa haemorrhagica Behçet's disease Bohn's nodules Burning mouth syndrome Candidiasis Condyloma acuminatum Darier's disease Epulis fissuratum Erythema multiforme Erythroplakia Fibroma Giant-cell Focal epithelial hyperplasia Fordyce spots Hairy leukoplakia Hand, foot and mouth disease Hereditary benign intraepithelial dyskeratosis Herpangina Herpes zoster Intraoral dental sinus Leukoedema Leukoplakia Lichen planus Linea alba Lupus erythematosus Melanocytic nevus Melanocytic oral lesion Molluscum contagiosum Morsicatio buccarum Oral cancer Benign: Squamous cell papilloma Keratoacanthoma Malignant: Adenosquamous carcinoma Basaloid squamous carcinoma Mucosal melanoma Spindle cell carcinoma Squamous cell carcinoma Verrucous carcinoma Oral florid papillomatosis Oral melanosis Smoker's melanosis Pemphigoid Benign mucous membrane Pemphigus Plasmoacanthoma Stomatitis Aphthous Denture-related Herpetic Smokeless tobacco keratosis Submucous fibrosis Ulceration Riga–Fede disease Verruca vulgaris Verruciform xanthoma White sponge nevus Teeth ( pulp , dentin , enamel ) Amelogenesis imperfecta Ankylosis Anodontia Caries Early childhood caries Concrescence Failure of eruption of teeth Dens evaginatus Talon cusp Dentin dysplasia Dentin hypersensitivity Dentinogenesis imperfecta Dilaceration Discoloration Ectopic enamel Enamel hypocalcification Enamel hypoplasia Turner's hypoplasia Enamel pearl Fluorosis Fusion Gemination Hyperdontia Hypodontia Maxillary lateral incisor agenesis Impaction Wisdom tooth impaction Macrodontia Meth mouth Microdontia Odontogenic tumors Keratocystic odontogenic tumour Odontoma Dens in dente Open contact Premature eruption Neonatal teeth Pulp calcification Pulp stone Pulp canal obliteration Pulp necrosis Pulp polyp Pulpitis Regional odontodysplasia Resorption Shovel-shaped incisors Supernumerary root Taurodontism Trauma Avulsion Cracked tooth syndrome Vertical root fracture Occlusal Tooth loss Edentulism Tooth wear Abrasion Abfraction Acid erosion Attrition Periodontium ( gingiva , periodontal ligament , cementum , alveolus ) – Gums and tooth-supporting structures Cementicle Cementoblastoma Gigantiform Cementoma Eruption cyst Epulis Pyogenic granuloma Congenital epulis Gingival enlargement Gingival cyst of the adult Gingival cyst of the newborn Gingivitis Desquamative Granulomatous Plasma cell Hereditary gingival fibromatosis Hypercementosis Hypocementosis Linear gingival erythema Necrotizing periodontal diseases Acute necrotizing ulcerative gingivitis Pericoronitis Peri-implantitis Periodontal abscess Periodontal trauma Periodontitis Aggressive As a manifestation of systemic disease Chronic Perio-endo lesion Teething Periapical, mandibular and maxillary hard tissues – Bones of jaws Agnathia Alveolar osteitis Buccal exostosis Cherubism Idiopathic osteosclerosis Mandibular fracture Microgenia Micrognathia Intraosseous cysts Odontogenic : periapical Dentigerous Buccal bifurcation Lateral periodontal Globulomaxillary Calcifying odontogenic Glandular odontogenic Non-odontogenic: Nasopalatine duct Median mandibular Median palatal Traumatic bone Osteoma Osteomyelitis Osteonecrosis Bisphosphonate-associated Neuralgia-inducing cavitational osteonecrosis Osteoradionecrosis Osteoporotic bone marrow defect Paget's disease of bone Periapical abscess Phoenix abscess Periapical periodontitis Stafne defect Torus mandibularis Temporomandibular joints , muscles of mastication and malocclusions – Jaw joints, chewing muscles and bite abnormalities Bruxism Condylar resorption Mandibular dislocation Malocclusion Crossbite Open bite Overbite Overeruption Overjet Prognathia Retrognathia Scissor bite Maxillary hypoplasia Temporomandibular joint dysfunction Salivary glands Benign lymphoepithelial lesion Ectopic salivary gland tissue Frey's syndrome HIV salivary gland disease Necrotizing sialometaplasia Mucocele Ranula Pneumoparotitis Salivary duct stricture Salivary gland aplasia Salivary gland atresia Salivary gland diverticulum Salivary gland fistula Salivary gland hyperplasia Salivary gland hypoplasia Salivary gland neoplasms Benign: Basal cell adenoma Canalicular adenoma Ductal papilloma Monomorphic adenoma Myoepithelioma Oncocytoma Papillary cystadenoma lymphomatosum Pleomorphic adenoma Sebaceous adenoma Malignant: Acinic cell carcinoma Adenocarcinoma Adenoid cystic carcinoma Carcinoma ex pleomorphic adenoma Lymphoma Mucoepidermoid carcinoma Sclerosing polycystic adenosis Sialadenitis Parotitis Chronic sclerosing sialadenitis Sialectasis Sialocele Sialodochitis Sialosis Sialolithiasis Sjögren's syndrome Orofacial soft tissues – Soft tissues around the mouth Actinomycosis Angioedema Basal cell carcinoma Cutaneous sinus of dental origin Cystic hygroma Gnathophyma Ludwig's angina Macrostomia Melkersson–Rosenthal syndrome Microstomia Noma Oral Crohn's disease Orofacial granulomatosis Perioral dermatitis Pyostomatitis vegetans Other Eagle syndrome Hemifacial hypertrophy Facial hemiatrophy Oral manifestations of systemic diseaseTAC1, AGTR2, FRMPD4, ZBTB11, CNTNAP2, FTSJ1, AP4E1, VPS13A, SPART, IQSEC2, CNKSR2, AP4S1, IL1RAPL1, POLR3A, MID2, PDE10A, AP4B1, MTHFS, SLC9A6, IKZF1, ATP6AP2, CERT1, MED12, SRPX2, SETD5, VAC14, SLC9A7, USP27X, TUBB2B, ZNF81, ARX, PTCHD1, TANGO2, RAB39B, FOXP2, GPT2, GFM2, POLR3B, ALG13, UPF3B, IRF2BPL, CXorf56, BCORL1, ALS2, SLC12A5, KIF15, ZC4H2, ZEB2, KMT2B, ATP1A3, ACSL4, MECP2, HLA-B, HCFC1, GRIN2A, GNS, GDI1, GCH1, GABRG2, FOXG1, EIF2S3, GABBR2, DMD, DLG3, DLAT, COL2A1, CLCN4, CACNA1C, ATRX, ATP7B, ATP6V1A, MIPEP, MRE11, PAK3, PMP22, ARHGEF6, NRXN1, TRIP12, AP4M1, USP9X, ZNF41, ZNF711, UBE3A, TSPAN7, TH, TCF4, SYP, SLC16A2, SCN8A, RPS6KA3, QDPR, PTS, PTCH1, PRPS1, ST20-MTHFS
-
Small Fiber Peripheral Neuropathy
Wikipedia
Furthermore, QST is limited by a patient's subjective experience of pain sensation. [11] Quantitative sudomotor axon reflex testing (QSART) measures sweating response at local body sites to evaluate the small nerve fibers that innervate sweat glands. [9] Skin biopsy [ edit ] A skin biopsy for the measurement of epidermal nerve fiber density is an increasingly common technique for the diagnosis of small fiber peripheral neuropathy. [9] Physicians can biopsy the skin with a 3-mm circular punch tool and immediately fix the specimen in 2% paraformaldehyde lysine-periodate or Zamboni's fixative. [12] Specimens are sent to a specialized laboratory for processing and analysis where the small nerve fibers are quantified by a neuropathologist to obtain a diagnostic result. [10] This skin punch biopsy measurement technique is called intraepidermal nerve fiber density (IENFD). [13] The following table describes the IENFD values in males and females of a 3 mm biopsy 10-cm above the lateral malleolus (above ankle outer side of leg). [13] Any value measured below the 0.05 Quantile IENFD values per age span, is considered a reliable positive diagnosis for Small Fiber Peripheral Neuropathy. [13] Intraepidermal nerve fiber density (IENFD) normative values for clinical use [13] Females Males Age in years 0.05 Quantile IENFD values per age span Median IENFD values per age span 0.05 Quantile IENFD values per age span Median IENFD values per age span 20–29 8.4 13.5 6.1 10.9 30–39 7.1 12.4 5.2 10.3 40–49 5.7 11.2 4.4 9.6 50–59 4.3 9.8 3.5 8.9 60–69 3.2 8.7 2.8 8.3 70–79 2.2 7.6 2.1 7.7 ≥80 1.6 6.7 1.7 7.2 Treatment [ edit ] Treatment is based on the underlying cause, if any. ... PMID 26872938 . ^ Levine, Todd D; Saperstein, David S (March 2015). "Routine use of punch biopsy to diagnose small fiber neuropathy in fibromyalgia patients" .
-
Bunion
Wikipedia
Deformity characterized by lateral deviation of the big toe Bunion Other names Hallux abducto valgus, hallux valgus, metatarsus primus varus [1] Specialty Orthopedics , Podiatry Symptoms Prominent, red, and painful joint at the base of the big toe [2] Complications Bursitis , arthritis [2] Usual onset Gradual [2] Causes Unclear [1] Risk factors Wearing overly tight shoes, high-heeled shoes , family history, rheumatoid arthritis [2] [3] Diagnostic method Based on symptoms, X-rays [2] Differential diagnosis Osteoarthritis , Freiberg's disease , hallux rigidus , Morton's neuroma [4] Treatment Proper shoes , orthotics , NSAIDs , surgery [2] Frequency ~23% of adults [1] A bunion , also known as hallux valgus , is a deformity of the joint connecting the big toe to the foot . [2] The big toe often bends towards the other toes and the joint becomes red and painful. [2] The onset of bunions is typically gradual. [2] Complications may include bursitis or arthritis . [2] The exact cause is unclear. [1] Proposed factors include wearing overly tight shoes , high-heeled shoes , family history, and rheumatoid arthritis . [2] [3] Diagnosis is generally based on symptoms and supported by X-rays . [2] A similar condition of the little toe is referred to as a bunionette . [2] Treatment may include proper shoes, orthotics , or NSAIDs . [2] If this is not effective for improving symptoms, surgery may be performed. [2] It affects about 23% of adults. [1] Females are affected more often than males. [2] Usual age of onset is between 20 and 50 years old. [1] The condition also becomes more common with age. [1] It was first clearly described in 1870. [1] Contents 1 Signs and symptoms 2 Cause 3 Pathophysiology 4 Diagnosis 5 Treatment 5.1 Orthotics 5.2 Surgery 6 References 7 External links Signs and symptoms [ edit ] Drawing of a bunion The big toe often bends towards the other toes and the joint becomes red and painful. [2] The onset of bunions is typically gradual. [2] Complications may include bursitis or arthritis . [2] Other symptoms may include irritation of the skin around the bunion, and blisters may form more easily at the site. Pain may be worse when walking Bunions can lead to difficulties finding properly fitting footwear and may force a person to buy a larger size shoe to accommodate the width of the bunion. ... ISBN 9783319603155 . ^ a b c d e f g h i j k l m n o p q r s t "Bunions" . OrthoInfo - AAOS . February 2016 .
- Slap Tear Wikipedia
-
Canine Leishmaniasis
Wikipedia
Barcelona, Spain ^ Ferroglio E, Maroli M, Gastaldo S, Mignone W, Rossi L (October 2005). ... External links [ edit ] Wikimedia Commons has media related to Canine leishmaniasis . The Canine Leishmaniasis Site by Vetstream Video of Leishmaniasis positive dog (<- link does not work) Treatment options (article in Italian) Overview of Canine Leishmaniasis US & Brazil 2002 US Department of Defense funded Canine Leishmaniasis Project Guidelines for practising veterinarians
-
Conductive Hearing Loss
Wikipedia
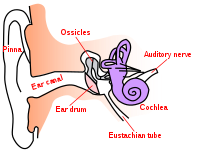
The following table compares sensorineural hearing loss to conductive: Criterion Sensorineural hearing loss Conductive hearing loss Anatomical site Inner ear , cranial nerve VIII, or central processing centers Middle ear (ossicular chain), tympanic membrane , or external ear Weber test Sound localizes to normal ear Sound localizes to affected ear (ear with conductive loss) Rinne test Positive Rinne; air conduction - bone conduction (both air and bone conduction are decreased equally, but the difference between them is unchanged). ... Retrieved 8 June 2013 . ^ a b Page 152 in: Rex S. Haberman (2004). Middle Ear and Mastoid Surgery .EYA1, NOG, GJB2, POU3F4, TCOF1, FGFR2, FRAS1, ANKH, ZBTB20, IFT172, IMPG2, TCTN3, DNAI1, STK36, OSTM1, SETD2, ANKRD11, SLC25A24, SCAPER, PTPN22, SOST, TBX22, DNAH1, SETD5, DNAAF2, ARMC4, CCDC40, PHIP, SDHAF2, DNAAF5, AHI1, HYDIN, RAB23, ZMYND10, NME8, TMEM216, POLR1D, GMNN, PRPF31, FSCN2, NIPBL, POMGNT1, CCNO, APC2, SF3B4, TOPORS, TSHZ1, NR2E3, KIAA0753, DHX38, HDAC4, IFT140, SEC24C, POLR1C, ADAMTS3, PIGL, ARHGAP29, MERTK, DEAF1, PRPF8, ARHGEF18, PRPF6, LRRC6, ARL2BP, GRIP1, CRB1, SPECC1L, IQSEC2, RAI1, KIF1B, SNRNP200, CNOT1, PRDM5, TXNL4A, GJB6, FANCI, KIZ, TMEM127, HGSNAT, CCBE1, GSC, RDH12, B3GLCT, AMER1, PIH1D3, ZNF513, DNAAF4, DNAAF1, TTC8, CCDC151, LRRC56, CCDC114, REEP6, C8orf37, JMJD1C, SPATA7, EYS, PCARE, CCDC103, CERKL, KIF7, DNAJB13, DNAAF3, RSPH4A, RSPH9, MCIDAS, FREM2, CCDC39, FAM149B1, STAC3, GAS2L2, DRC1, CDHR1, TMEM67, GRHL3, DNAI2, NSD1, SEMA4A, PRDM16, ELMO2, AGBL5, SLC7A14, CREB3L1, KIAA1549, SALL4, CFAP298, KLHL7, HDAC8, LONP1, CPLANE1, FAT4, ZNF408, DHDDS, ASXL3, TTC25, DNAL1, RSPH3, CDCA7, ARL6, FAM161A, SLITRK6, ZNF469, CFAP300, CCDC65, RSPH1, TSR2, RECQL4, ABCA4, EFTUD2, MDH2, FLNB, GABRD, GAS8, GATA1, GJA1, GP1BB, GUCA1B, IDH3A, IDH3B, IMPDH1, IRF6, LRP5, MAK, MAX, MEOX1, POR, KMT2A, MSX1, MYH3, NEK1, NEK2, NFIX, NOTCH2, NOTCH3, NRL, PAX1, PDE6A, PDE6D, PDE6G, PGM3, FLNA, FLII, FH, FGFR3, ACVR1, AHR, ALX3, ARL3, ARVCF, RERE, BBS2, BMP2, BMP4, CA4, CDH1, CHRNG, CNGB1, CNGA1, COL2A1, COL11A2, COMT, CRX, CTNND1, DHODH, DLG1, DLST, DLX4, DNAH5, EDNRA, ERF, EXT1, FBN1, FGF9, PRRX1, PDE6B, MASP1, UBB, BEST1, VHL, KDM6A, CLRN1, USH2A, UFD1, TWIST1, KMT2D, HIRA, TULP1, TUB, TRPS1, TFAP2A, NECTIN1, PCGF2, ALX1, MAP3K7, DNAH11, LRAT, PRPF3, PRPF4, SMC3, PROM1, TNFRSF11A, DCHS1, IFT88, TP63, KCNAB2, OFD1, SLC25A11, SMC1A, GDF5, TBX1, PRCD, SPAG1, RPE65, RAD21, RAP1A, RAP1B, RBP3, PRPH2, RET, RGR, RHO, RLBP1, ROM1, RP9, RP1, SNRPB, RPGR, RP2, RPS23, SDHA, SKI, SIX1, SDHD, SDHC, SDHB, SC5D, SAG, RREB1, TECTA, SDC2, DMP1, OTOGL, IDUA, SIX2, COL1A1, NT5E, HSPG2, GMDS, ANK1, ABR, ENPP1
-
Cholesterol Embolism
Wikipedia
Most commonly this causes skin symptoms (usually livedo reticularis ), gangrene of the extremities and sometimes kidney failure ; problems with other organs may arise, depending on the site at which the cholesterol crystals enter the bloodstream. [2] When the kidneys are involved, the disease is referred to as atheroembolic renal disease . [3] The diagnosis usually involves biopsy (removing a tissue sample) from an affected organ. ... PMID 11461954 . ^ Schwarcz TH; Eton D; Ellenby MI; Stelmack T; McMahon TT; Mulder S; Meyer JP; Eldrup-Jorgensen J; Durham JR (May 1990).
-
Tardbp-Related Amyotrophic Lateral Sclerosis
Gene_reviews
Pathogenic variants may include small intragenic deletions/insertions and missense, nonsense, and splice site variants; typically, exon or whole-gene deletions/duplications are not detected. ... However, bulbar onset appears to predominate in Asian individuals [Corcia et al 2012] and intra- and interfamilial variability in the site of onset is observed even with the same pathogenic variant (see Genotype-Phenotype Correlations). ... Within families, no genotype-phenotype correlations have been made with regard to site of onset, with both limb onset and bulbar onset being observed in the same family. Disparate sites of onset were seen in unrelated persons with the same pathogenic variant, including the following: p.Gly287Ser [Corrado et al 2009, Kabashi et al 2008], p.Gly294Val [Corrado et al 2009, Del Bo et al 2009], and p.Ala382Thr [Kabashi et al 2008]. ... The mimics of ALS from any cause are numerous and include: Multifocal motor neuropathy Cervical spondylosis Adult-onset spinal muscular atrophy (SMA) Kennedy disease (X-linked spinobulbar muscular atrophy [SBMA]) Acquired and hereditary motor neuropathies (see Charcot-Marie-Tooth Hereditary Neuropathy Overview) Late-onset GM2 gangliosidosis (see Hexosaminidase A Deficiency) Adult polyglucosan body disease The number of other genes associated with FALS (see Note) has been rapidly increasing and is tracked at the ALSoD site. Some examples: ALS1. SOD1 (encoding the protein superoxide dismutase) ALS4.
-
Lissencephaly
Wikipedia
Philadelphia: Elsevier Saunders. ^ a b c Fong KW, Ghai S, Toi A, Blaser S, Winsor EJ, Chitayat D (December 2004). ... PMID 15586369 . ^ Joseph LD, Kuruvilla S (2008). "Cytomegalovirus infection with lissencephaly" . ... Retrieved 20 May 2018 . ^ a b Liu, J. S.; Schubert, C. R.; Walsh, C. A. (2012). ... PMID 16387638 . S2CID 15362872 . ^ Nishikawa S, Goto S, Yamada K, Hamasaki T, Ushio Y (June 2003). ... European Journal of Radiology . 8 (2): 131–3. PMID 3383858 . ^ Ghai S, Fong KW, Toi A, Chitayat D, Pantazi S, Blaser S (2006).PAFAH1B1, NDE1, MACF1, TMTC3, TUBA1A, CTNNA2, LAMB1, ARX, DCX, TUBB2B, DAG1, ZIC1, CRADD, YWHAE, PEX13, ACTG1, MPDZ, TUBB3, STS, PHGDH, PSAT1, CDK5, SLC25A19, CTU2, EXOSC3, NBN, TUBA3E, KIAA1109, PEX26, HIC1, FTO, RELN, DISC1, TUBA1B, ACTB, CRK, VLDLR, TUBG1, RMDN3, SYBU, KIF2A, CD6, CAMKMT, NDEL1, KRIT1, CASP2, RMDN2, CAST, CALM3, WDR62, CALM2, CALM1, MECP2, CHCHD2, RMDN1, TUBGCP2, ADGRG1, KIAA0319, APC2, KATNB1, TSC2, TSC1, WDR47, NPC1, SMG6, TP53, STXBP1, STIL, DBNL, PTAFR, RNU4ATAC
-
Sydenham's Chorea
Wikipedia
S2CID 23605799 . ^ Dale RC, Merheb V, Pillai S, et al. (2012). "Antibodies to surface dopamine-2 receptor in autoimmune movement and psychiatric disorders" . ... External links [ edit ] Classification D ICD - 10 : I02 ICD - 9-CM : 392 MeSH : D002819 DiseasesDB : 29245 SNOMED CT : 46826000 External resources MedlinePlus : 001358 Patient UK : Sydenham's chorea v t e Cardiovascular disease (heart) Ischaemic Coronary disease Coronary artery disease (CAD) Coronary artery aneurysm Spontaneous coronary artery dissection (SCAD) Coronary thrombosis Coronary vasospasm Myocardial bridge Active ischemia Angina pectoris Prinzmetal's angina Stable angina Acute coronary syndrome Myocardial infarction Unstable angina Sequelae hours Hibernating myocardium Myocardial stunning days Myocardial rupture weeks Aneurysm of heart / Ventricular aneurysm Dressler syndrome Layers Pericardium Pericarditis Acute Chronic / Constrictive Pericardial effusion Cardiac tamponade Hemopericardium Myocardium Myocarditis Chagas disease Cardiomyopathy Dilated Alcoholic Hypertrophic Tachycardia-induced Restrictive Loeffler endocarditis Cardiac amyloidosis Endocardial fibroelastosis Arrhythmogenic right ventricular dysplasia Endocardium / valves Endocarditis infective endocarditis Subacute bacterial endocarditis non-infective endocarditis Libman–Sacks endocarditis Nonbacterial thrombotic endocarditis Valves mitral regurgitation prolapse stenosis aortic stenosis insufficiency tricuspid stenosis insufficiency pulmonary stenosis insufficiency Conduction / arrhythmia Bradycardia Sinus bradycardia Sick sinus syndrome Heart block : Sinoatrial AV 1° 2° 3° Intraventricular Bundle branch block Right Left Left anterior fascicle Left posterior fascicle Bifascicular Trifascicular Adams–Stokes syndrome Tachycardia ( paroxysmal and sinus ) Supraventricular Atrial Multifocal Junctional AV nodal reentrant Junctional ectopic Ventricular Accelerated idioventricular rhythm Catecholaminergic polymorphic Torsades de pointes Premature contraction Atrial Junctional Ventricular Pre-excitation syndrome Lown–Ganong–Levine Wolff–Parkinson–White Flutter / fibrillation Atrial flutter Ventricular flutter Atrial fibrillation Familial Ventricular fibrillation Pacemaker Ectopic pacemaker / Ectopic beat Multifocal atrial tachycardia Pacemaker syndrome Parasystole Wandering atrial pacemaker Long QT syndrome Andersen–Tawil Jervell and Lange-Nielsen Romano–Ward Cardiac arrest Sudden cardiac death Asystole Pulseless electrical activity Sinoatrial arrest Other / ungrouped hexaxial reference system Right axis deviation Left axis deviation QT Short QT syndrome T T wave alternans ST Osborn wave ST elevation ST depression Strain pattern Cardiomegaly Ventricular hypertrophy Left Right / Cor pulmonale Atrial enlargement Left Right Athletic heart syndrome Other Cardiac fibrosis Heart failure Diastolic heart failure Cardiac asthma Rheumatic fever v t e Firmicutes (low- G+C ) Infectious diseases Bacterial diseases : G+ Bacilli Lactobacillales ( Cat- ) Streptococcus α optochin susceptible S. pneumoniae Pneumococcal infection optochin resistant Viridans streptococci : S. mitis S. mutans S. oralis S. sanguinis S. sobrinus S. anginosus group β A bacitracin susceptible: S. pyogenes Group A streptococcal infection Streptococcal pharyngitis Scarlet fever Erysipelas Rheumatic fever B bacitracin resistant, CAMP test +: S. agalactiae Group B streptococcal infection ungrouped Streptococcus iniae Cutaneous Streptococcus iniae infection γ D BEA +: Streptococcus bovis Enterococcus BEA +: Enterococcus faecalis Urinary tract infection Enterococcus faecium Bacillales ( Cat+ ) Staphylococcus Cg+ S. aureus Staphylococcal scalded skin syndrome Toxic shock syndrome MRSA Cg- novobiocin susceptible S. epidermidis novobiocin resistant S. saprophyticus Bacillus Bacillus anthracis Anthrax Bacillus cereus Food poisoning Listeria Listeria monocytogenes Listeriosis Clostridia Clostridium ( spore -forming) motile: Clostridium difficile Pseudomembranous colitis Clostridium botulinum Botulism Clostridium tetani Tetanus nonmotile: Clostridium perfringens Gas gangrene Clostridial necrotizing enteritis Finegoldia (non-spore forming) Finegoldia magna Mollicutes Mycoplasmataceae Ureaplasma urealyticum Ureaplasma infection Mycoplasma genitalium Mycoplasma pneumoniae Mycoplasma pneumonia Anaeroplasmatales Erysipelothrix rhusiopathiae Erysipeloid