-
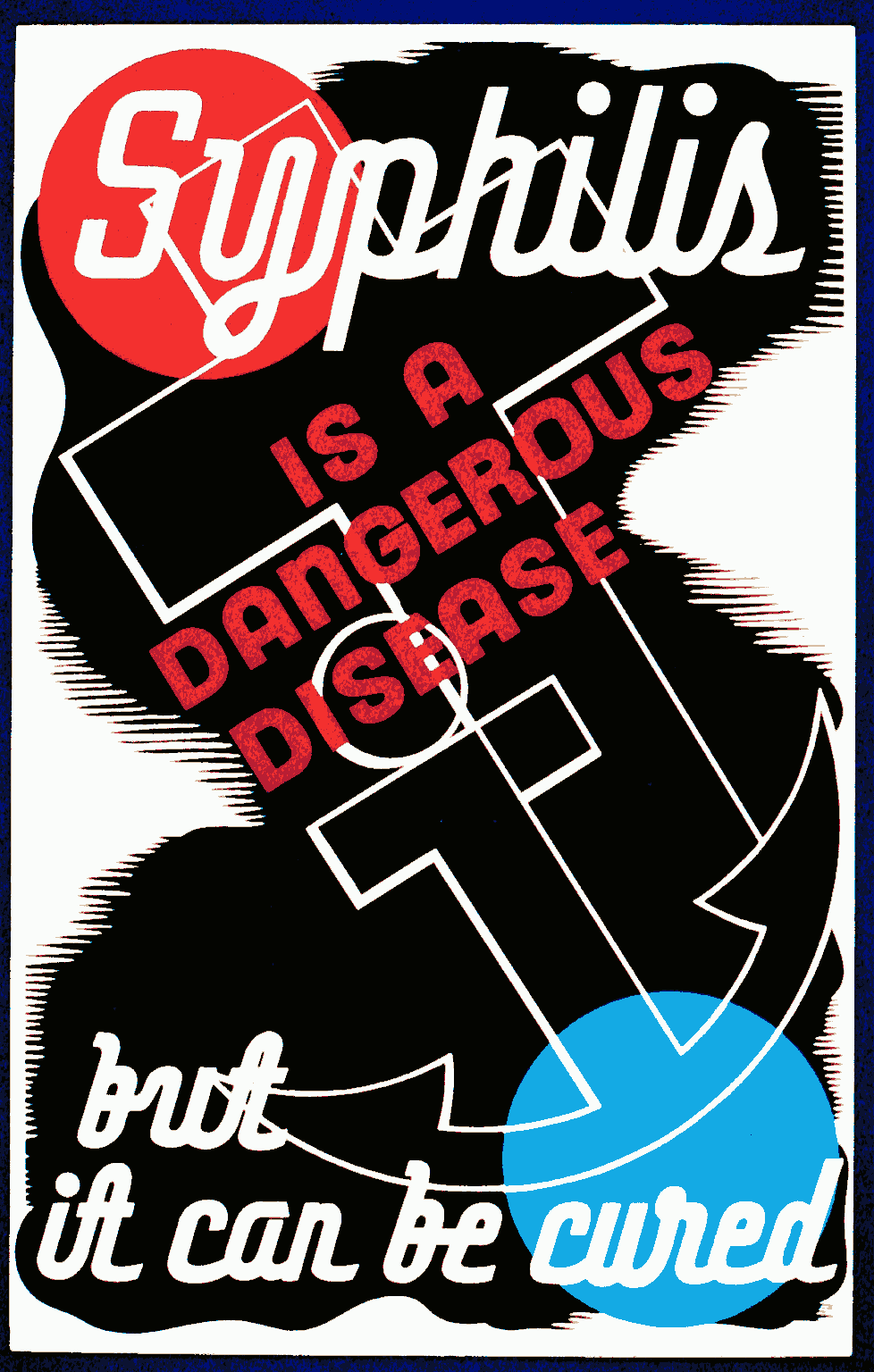
Sexually Transmitted Infection
Wikipedia
People with AIDS fall prey to opportunistic infections and die as a result. [56] When the disease was first discovered in the 1980s, those who had AIDS were not likely to live longer than a few years. ... Nora Wattie , OBE, Venereal Diseases Officer in Glasgow from 1929, encouraged contact tracing and volunteering for treatment, rather than the prevailing more judgemental view and published her own research on improving sex education and maternity care. [115] The first effective treatment for a sexually transmitted disease was salvarsan , a treatment for syphilis. ... This article incorporates public domain material from websites or documents of the Centers for Disease Control and Prevention . ^ a b Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. ... New York: McGraw-Hill Medical. ISBN 978-0-07-171672-7 . [ page needed ] ^ Kennedy CE, Yeh PT, Pandey S, Betran AP, Narasimhan M (July 2017). ... CreateSpace, Scotts Valley, CA, 2009. ISBN 1-4486-6472-1 [ page needed ] ^ Obiero J, Mwethera PG, Wiysonge CS (June 2012).SULT2A1, ZAP70, KLK3, IFNE, AGRP, PREP, PAEP, ARTN, PTPN22, CXCL8, IL1B, TLR4, EXTL3, ERVK-6, CCL27, TNFRSF1A, UBE2B, WAS, ARSH, MARCHF8, ANC, MESP2, ARID1A, EMB, ESPL1, SART3, SMC5, CPAT1, CADM1, NLRP3, MLST8, ERVW-1, LHPP, TLR9, CRLS1, SARS2, FBXW7, IMPACT, PLXNA3, DDX41, RRM2, TRIM21, DEFA5, HSPD1, HSPA4, HLA-A, GRB2, GPI, FCGRT, CUX1, SRY, CRP, CCR5, CD38, CAMP, CALR, B2M, IFNA1, IFNA13, IFNG, IL6, IL16, CXCL10, KIT, LRP1, MSMB, NDUFAB1, NHS, PNP, PKHD1, PMAIP1, RPS6KA3, APP, SARS1, ERVK-20
-
Late Talker
Wikipedia
Initially the most prominent types are nouns and eventually they move on to other word types such as verbs and adjectives . [16] Once a toddler has said his first word, he will begin to acquire new words at a rate of roughly one per week [17] Words will be related to things in the toddler's environment such as body parts, toys, clothes, etc. ... Around the 15-month mark toddlers will know six words on average, [18] and begin to notice and wonder about things that are a little outside of their environment. [16] Once they reach 18 months, they refer to themselves by their name and eventually start using the pronoun 'I'. [16] During this stage, they will also repeat parts of sentences they hear. [18] As they get close to 2 years, toddlers start putting two words together. [16] They begin to learn the use of "no" and ask adults to tell them the name of people and new objects. [18] On average, a 2-year-old will know 50 words [18] and will then begin to learn new words at a rate of approximately one per day. [17] From 2 to 3 years of age, their vocabulary grows rapidly. [18] At 30 months old they are expected to know around 200 words and by 3 they will be able to participate in very simple conversations. [18] Late talker's language emergence [ edit ] See also: Language delay Late language emergence (LLE) occurs when a toddler does not produce or comprehend language at the expected rate for their age. [2] About 13% of two-year-olds experience a delay in language emergence. [19] Late talkers differ from toddlers with language development disorders and disabilities in the sense that their only characteristic is that they experience limited expressive vocabulary for their age, as opposed to, lack of receptive language or cognitive abilities . [6] LLE can be an indicator of other kinds of disorders or disabilities. [20] If a late talker is not catching-up to typical talkers by the age of 4, they could have specific language impairment. [21] Expressive language screening between the ages of 18-35 months help determine if LLE is "secondary to autism spectrum disorder, intellectual disability, hearing impairment, receptive language delay, or demographic risk". [20] When compared to typical talkers, 24-month-old late talkers do not seem to struggle with verbs and their formation, which are an important part of one's grammatical development. [21] They struggle with nouns more than a typical talker and have difficulty combining words. [21] Late talkers perform lower than typical talkers in cognitive functioning and receptive language skills. [22] Signs and symptoms [ edit ] A toddler is at risk of being a late talker if: They produced abnormal babbling from 9 to 21 months of age. [23] [2] By 15 months they are not producing six or more words. [18] By 18 months they do not appear to comprehend more words than they can produce. [18] At 18 months old they're using less than 20 words and lack knowledge of different word-types. [9] At 24 months old, they're using less than 50 words and are not combining words from different word classes. [9] [1] After producing their first word, they demonstrate a lack of "complex syllable structures, lower percentage of consonants correct, and smaller consonant and vowel inventories". [2] They show a lack of comprehension and insist on communicating using gestures . [2] Between 2 and 3 years of age, they're using short sentences with very simple grammar. [2] Diagnosis [ edit ] LLE could be a sign of other types of language disorders or intellectual disabilities , [20] so there is a risk of misdiagnosing a child as just being a late talker. ... "A Focused language Stimulation Approach: First Vocabulary for Children With Specific Language Impairment". ... "Prespeech and early speech development of two late talkers". First Language . 9 (6): 207–223. doi : 10.1177/014272378900900607 .
-
Complications Of Pregnancy
Wikipedia
Treatment : Prophylactic treatment, e.g. with low molecular weight heparin may be indicated when there are additional risk factors for deep vein thrombosis. [16] v t e Absolute and relative incidence of venous thromboembolism (VTE) during pregnancy and the postpartum period Absolute incidence of first VTE per 10,000 person–years during pregnancy and the postpartum period Swedish data A Swedish data B English data Danish data Time period N Rate (95% CI) N Rate (95% CI) N Rate (95% CI) N Rate (95% CI) Outside pregnancy 1105 4.2 (4.0–4.4) 1015 3.8 (?) 1480 3.2 (3.0–3.3) 2895 3.6 (3.4–3.7) Antepartum 995 20.5 (19.2–21.8) 690 14.2 (13.2–15.3) 156 9.9 (8.5–11.6) 491 10.7 (9.7–11.6) Trimester 1 207 13.6 (11.8–15.5) 172 11.3 (9.7–13.1) 23 4.6 (3.1–7.0) 61 4.1 (3.2–5.2) Trimester 2 275 17.4 (15.4–19.6) 178 11.2 (9.7–13.0) 30 5.8 (4.1–8.3) 75 5.7 (4.6–7.2) Trimester 3 513 29.2 (26.8–31.9) 340 19.4 (17.4–21.6) 103 18.2 (15.0–22.1) 355 19.7 (17.7–21.9) Around delivery 115 154.6 (128.8–185.6) 79 106.1 (85.1–132.3) 34 142.8 (102.0–199.8) – Postpartum 649 42.3 (39.2–45.7) 509 33.1 (30.4–36.1) 135 27.4 (23.1–32.4) 218 17.5 (15.3–20.0) Early postpartum 584 75.4 (69.6–81.8) 460 59.3 (54.1–65.0) 177 46.8 (39.1–56.1) 199 30.4 (26.4–35.0) Late postpartum 65 8.5 (7.0–10.9) 49 6.4 (4.9–8.5) 18 7.3 (4.6–11.6) 319 3.2 (1.9–5.0) Incidence rate ratios (IRRs) of first VTE during pregnancy and the postpartum period Swedish data A Swedish data B English data Danish data Time period IRR* (95% CI) IRR* (95% CI) IRR (95% CI)† IRR (95% CI)† Outside pregnancy Reference (i.e., 1.00) Antepartum 5.08 (4.66–5.54) 3.80 (3.44–4.19) 3.10 (2.63–3.66) 2.95 (2.68–3.25) Trimester 1 3.42 (2.95–3.98) 3.04 (2.58–3.56) 1.46 (0.96–2.20) 1.12 (0.86–1.45) Trimester 2 4.31 (3.78–4.93) 3.01 (2.56–3.53) 1.82 (1.27–2.62) 1.58 (1.24–1.99) Trimester 3 7.14 (6.43–7.94) 5.12 (4.53–5.80) 5.69 (4.66–6.95) 5.48 (4.89–6.12) Around delivery 37.5 (30.9–44.45) 27.97 (22.24–35.17) 44.5 (31.68–62.54) – Postpartum 10.21 (9.27–11.25) 8.72 (7.83–9.70) 8.54 (7.16–10.19) 4.85 (4.21–5.57) Early postpartum 19.27 (16.53–20.21) 15.62 (14.00–17.45) 14.61 (12.10–17.67) 8.44 (7.27–9.75) Late postpartum 2.06 (1.60–2.64) 1.69 (1.26–2.25) 2.29 (1.44–3.65) 0.89 (0.53–1.39) Notes: Swedish data A = Using any code for VTE regardless of confirmation. Swedish data B = Using only algorithm-confirmed VTE. Early postpartum = First 6 weeks after delivery. Late postpartum = More than 6 weeks after delivery. * = Adjusted for age and calendar year. † = Unadjusted ratio calculated based on the data provided. ... If the pregnancy is very early, it may resolve on its own, or it can be treated with methotrexate , an abortifacient . [25] Miscarriage [ edit ] Miscarriage is the loss of a pregnancy prior to 20 weeks. [26] In the UK, miscarriage is defined as the loss of a pregnancy during the first 23 weeks. [27] Placental abruption [ edit ] Placental abruption is the separation of the placenta from the uterus. [7] Caused by : Various causes; risk factors include maternal hypertension , trauma , and drug use.
-
Female Genital Mutilation
Wikipedia
Reinfibulation can involve cutting the vagina again to restore the pinhole size of the first infibulation. This might be performed before marriage, and after childbirth, divorce and widowhood. ... The first publication to estimate FGM prevalence based on DHS data (in seven countries) was written by Dara Carr of Macro International in 1997. [70] Type of FGM Questions the women are asked during the surveys include: "Was the genital area just nicked/cut without removing any flesh? ... [x] Christian missionaries in Africa were among the first to object to FGM, [141] but Christian communities in Africa do practise it. ... Have him separate and steady her legs and whole body. Standing in front and taking hold of the clitoris with a broad-mouthed forceps in his left hand, the surgeon stretches it outward, while with the right hand, he cuts it off at the point next to the pincers of the forceps. ... Unexcised Kikuyu women ( irugu ) were outcasts. [171] Jomo Kenyatta , general secretary of the Kikuyu Central Association and later Kenya's first prime minister, wrote in 1938 that, for the Kikuyu, the institution of FGM was the " conditio sine qua non of the whole teaching of tribal law, religion and morality".
-
Food Intolerance
Wikipedia
The most effective dietary regimen is exclusively breastfeeding for at least 4–6 months or, in absence of breast milk, formulas with documented reduced allergenicity for at least the first 4 months, combined with avoidance of solid food and cow's milk for the first 4 months. [54] [55] Management [ edit ] Individuals can try minor changes of diet to exclude foods causing obvious reactions, and for many this may be adequate without the need for professional assistance. ... It takes around five days of total abstinence to unmask a food or chemical, during the first week on an elimination diet withdrawal symptoms can occur but it takes at least two weeks to remove residual traces. ... Using this approach the role played by dietary chemical factors in the pathogenesis of chronic idiopathic urticaria (CIU) was first established and set the stage for future DBPCT trials of such substances in food intolerance studies. [65] [66] In 1995 the European Academy of Allergology and Clinical Immunology suggested a classification on the basis of the responsible pathogenetic mechanism; according to this classification, non-toxic reactions can be divided into 'food allergies' when they recognize immunological mechanisms, and 'food intolerances' when there are no immunological implications.
-
Medial Knee Injuries
Wikipedia
Swelling is managed well with rest, ice, elevation, and compression wraps. [22] Protection can be performed using a hinged brace that stabilizes against varus and valgus stress but allows full flexion and extension. The brace should be worn for the first four to six weeks of rehabilitation , especially during physical exercise to prevent trauma to the healing ligament. ... After verifying the correct anatomic eyelet pin placement, a 7-mm reamer is used over the pin to drill a tunnel depth of 25 mm. [27] Moving to the femoral attachments of the ligaments, the first step is identifying the adductor magnus muscle tendon, and its corresponding attachment site, near the adductor tubercle. ... This soft-tissue attachment can be reproduced with a suture anchor [28] placed 12.2 mm distal to the medial joint line (average location), directly medial to the anterior arm of the semimembranosus tibial attachment. [27] Once this aspect of the sMCL is secured to the suture anchor, the knee is put through range of motion testing by the physician to determine the "safe zone" of knee motion which is used during the first post-operative day rehabilitation (below). [27] Rehabilitation [ edit ] Nonoperative Rehabilitation As mentioned in the Nonoperative Treatment section, the principles of rehabilitation are to control swelling , protect the knee (bracing), reactivate the quadriceps muscle, and restore range of motion . ... Non-weight bearing to touch-down weight bearing is recommended for the first 6 weeks, progressing to closed-kinetic-chain exercises thereafter.
-
Cannabinoid Hyperemesis Syndrome
Wikipedia
Nausea and vomiting resulting from cannabis use Cannabinoid hyperemesis syndrome (CHS) People with CHS often find some relief with hot showers [1] Specialty Toxicology Symptoms Nausea, vomiting, stomach pain [2] Complications Kidney failure , electrolyte problems , skin burns from hot water [1] Causes Long term cannabis use [2] Diagnostic method Based on the symptoms [1] Differential diagnosis Cyclical vomiting syndrome [1] Treatment Stopping cannabis, hot showers [2] Medication Capsaicin cream [1] Frequency 2.7 million per year (US) [1] Cannabinoid hyperemesis syndrome ( CHS ) is recurrent nausea , vomiting , and cramping abdominal pain due to cannabis use. [3] These symptoms may improve temporarily by taking a hot shower or bath. [1] Complications may include kidney failure , electrolyte problems , and skin burns from hot water. [1] At least two deaths have been associated with CHS. [1] [4] [5] Weekly cannabis use is generally required for the syndrome to occur. [1] The underlying mechanism is unclear, with several possibilities proposed. [1] Diagnosis is based on the symptoms. [1] The condition is typically present for some time before the diagnosis is made. [1] Another condition that may present similarly is cyclic vomiting syndrome . [1] Definitive treatment involves stopping use of cannabis. [1] Up to two weeks may be required to see a benefit. [1] Treatments during an episode of vomiting is generally supportive in nature. [1] There is tentative evidence for the use of capsaicin cream on the abdomen during an acute episode. [1] The number of people affected is unclear. [6] Of those who go to the emergency department in the United States with recurrent vomiting, about 6% have the condition. [1] The syndrome was first described in 2004, and simplified diagnostic criteria published in 2009. [7] [8] Contents 1 Signs and symptoms 1.1 Prodromal phase 1.2 Hyperemetic phase 1.3 Recovery phase 1.4 Complications 2 Pathogenesis 2.1 Cannabinoid buildup theory 2.2 Hypothalamic theory 2.3 TRPV1 theory 3 Diagnosis 3.1 Differential diagnosis 4 Treatment 5 Prognosis 6 Epidemiology 7 History 8 Society and culture 9 Research directions 10 References 11 External links Signs and symptoms [ edit ] The long-term and short-term effects of cannabis use are associated with behavioral effects leading to a wide variety of effects on the body systems and physiological states. [8] CHS is a paradoxical syndrome characterized by hyperemesis (persistent vomiting), as opposed to the better known antiemetic properties of cannabinoids. [9] Specifically, CHS takes the pattern of cyclical nausea, vomiting, and abdominal pain in the setting of chronic cannabinoid use. [9] The abdominal pain tends to be mild and diffused. [10] There are three phases of CHS: the prodromal phase, the hyperemetic phase, and the recovery phase. [11] Prodromal phase [ edit ] The prodromal phase is characterized by subsyndromal symptoms of CHS, including mild discomfort and nausea upon waking. ... Treatment is otherwise supportive and focuses on stopping cannabis use. [20] With the cessation of cannabinoid use, complete symptomatic relief can take between 7–10 days. [21] Proper patient education includes informing patients that their symptoms are due to their use of cannabis/cannabinoids, and that exposure to cannabinoids in the future are likely to cause their symptoms to return. [21] Clinical pharmacists can play a role in administering this education, as well as encouraging patients to seek the assistance of mental health providers. [11] Abstinence from cannabinoids currently remains the only definitive treatment. [3] Cognitive behavioral therapy and motivational enhancement therapy are evidence-based outpatient treatment options for patients with cannabis use disorder . [10] Symptomatic relief is noted with exposure to hot water (greater than 41 degrees C), which is mediated by TRPV –the capsaicin receptor. [21] Assessing for dehydration due to vomiting and hot showers is important as it can lead to acute kidney failure , and this is easily treated with IV fluids. [13] If dehydration is severe, hospitalization may be required. [10] Based on the mechanism of the effect, some clinicians have used topical capsaicin cream applied to the periumbilical area in the treatment of acute CHS. [21] The use of capsaicin as first-line treatment for CHS has been well tolerated, though the evidence for efficacy is limited. [21] The use of hot water showers in the emergency department setting has been advocated in situations where topical capsaicin cream is unavailable, though the same precautions to hot water use (dehydration, burn injury) are required. [21] The use of antipsychotics , such as haloperidol and olanzapine , have provided complete relief of symptoms in case-reports. [21] [22] The evidence for the use of benzodiazepines , such as lorazepam , [22] has shown mixed results. [21] Other drug treatments that have been tried, with unclear efficacy, include neurokinin-1 receptor antagonists , [10] first-generation antihistamines (e.g. diphenhydramine ), 5-HT 3 receptor antagonists (e.g. ondansetron ), and non-antipsychotic antidopaminergics (e.g. metoclopramide ). [21] Acetaminophen has shown some benefit in case reports for alleviating headaches associated with CHS. [11] Opioids can provide some relief of abdominal pain, but their use is discouraged due to the risk of worsening nausea and vomiting. [10] Prognosis [ edit ] Acute episodes of cannabinoid hyperemesis typically lasts for 24–48 hours and the problem often resolves with long term stopping of cannabis use. Improvement can take one to three months to occur. [11] Relapses are common, and this is thought to be possibly secondary to a lack of education as many people use or increase their use of cannabis due to their symptoms of nausea and vomiting. [10] Epidemiology [ edit ] The number of people affected is unclear as of 2015, [6] though one estimate puts the number at about 2.7 million people in the United States a year. [1] Among users smoking 20 or more days per month, about one-third might experience symptoms. [23] CHS has been reported more frequently in people that use cannabis daily (47.9% of patients) and greater than daily (23.7% of patients), compared to once weekly users (19.4% of patients) and less frequent users (2.4% of patients). [3] A significant increase in the incidence of CHS (and other marijuana-related visits to the emergency department) has been noted in U.S. states that have legalized marijuana , with the incidence of cyclic vomiting prominently doubling in the US state of Colorado after legalization. [21] As the use of marijuana continues to be legalized at the state level, the prevalence of CHS is expected to increase in the US. [3] A 2018 surveyed of 155 heavy cannabis users in hospital found 51 of them experienced CHS. [1] This ratio was used to estimate that in the United States, 2.7 million out of 8.3 million heavy cannabis users should be experiencing the syndrome. [1] The same study found that of those who go to the emergency department in the United States with recurrent vomiting, about 6% have the condition. [1] In 2018 a 17 year old died of the condition. [24] History [ edit ] Cannabinoid hyperemesis was first reported in the Adelaide Hills of South Australia in 2004. [7] The name cannabinoid hyperemesis syndrome was also coined at this time.
-
Allergy
Wikipedia
Many bacteria and viruses elicit a TH1 -mediated immune response, which down-regulates TH2 responses. The first proposed mechanism of action of the hygiene hypothesis was that insufficient stimulation of the TH1 arm of the immune system leads to an overactive TH2 arm, which in turn leads to allergic disease. [57] In other words, individuals living in too sterile an environment are not exposed to enough pathogens to keep the immune system busy. ... Studies have shown that various immunological and autoimmune diseases are much less common in the developing world than the industrialized world and that immigrants to the industrialized world from the developing world increasingly develop immunological disorders in relation to the length of time since arrival in the industrialized world. [59] Longitudinal studies in the third world demonstrate an increase in immunological disorders as a country grows more affluent and, it is presumed, cleaner. [60] The use of antibiotics in the first year of life has been linked to asthma and other allergic diseases. [61] The use of antibacterial cleaning products has also been associated with higher incidence of asthma , as has birth by Caesarean section rather than vaginal birth. [62] [63] Stress [ edit ] Chronic stress can aggravate allergic conditions. ... In the early stages of allergy, a type I hypersensitivity reaction against an allergen encountered for the first time and presented by a professional antigen-presenting cell causes a response in a type of immune cell called a T H 2 lymphocyte ; a subset of T cells that produce a cytokine called interleukin-4 (IL-4). ... Prevention [ edit ] Further information: Allergy prevention in children Giving peanut products early may decrease the risk allergies while only breastfeeding during at least the first few months of life may decrease the risk of dermatitis . [93] [94] There is no good evidence that a mother's diet during pregnancy or breastfeeding affects the risk. [93] Nor is there evidence that delayed introduction of certain foods is useful. [93] Early exposure to potential allergens may actually be protective. [6] Fish oil supplementation during pregnancy is associated with a lower risk. [94] Probiotic supplements during pregnancy or infancy may help to prevent atopic dermatitis . [95] [96] Management [ edit ] Management of allergies typically involves avoiding what triggers the allergy and medications to improve the symptoms. [7] Allergen immunotherapy may be useful for some types of allergies. [7] Medication [ edit ] Several medications may be used to block the action of allergic mediators, or to prevent activation of cells and degranulation processes. ... Archived from the original (PDF) on 27 June 2013. ^ Finn, DF; Walsh, JJ (September 2013). "Twenty-first century mast cell stabilizers" .CCL2, HLA-B, IL17A, IL4, PPBP, CCL8, CCL7, CCL4, CCL3, MAP2K6, PF4, IL16, MYLK, MTHFR, CXCL9, KNG1, ITGB2, IL18, CCL11, ABCF1, CCL19, CCL20, COMMD1, CLEC4A, CD274, CCR9, IL1R2, TNFRSF1B, TNFRSF1A, TNF, TGFB1, TAC1, SPP1, SELP, CX3CL1, CXCL5, CCL24, CCL17, CCR2, IL13, HLA-DRB4, ALB, CASP1, CD40LG, CCR1, CCR6, CSF2RA, CXCR2, DSG1, CXCR3, CXCL1, HLA-DQA1, HLA-DQB1, HLA-DRB1, CYP1A1, HLA-DRB5, IL2RB, IL6, IL6ST, IFNG, IL5RA, HP, IL1B, IL1R1, AKR1B1, CHD1, BBS1, ADA, ARID1B, FOXP3, CSTA, CCDC28B, MTOR, TGM5, TRPA1, HAVCR2, IL31, TLR4, CD14, TRPV1, JAK2, TLR2, CRHR1, SLC6A3, SFTPD, F2RL1, NOS1, GZMB, HTR2B, LMAN1
-
Influenza
Wikipedia
One possible explanation is that, because people are indoors more often during the winter, they are in close contact more often, and this promotes transmission from person to person. ... It was introduced into English in the mid-eighteenth century during a pan-European epidemic. [202] Archaic terms for influenza include epidemic catarrh , la grippe (from the French, first used by Molyneaux in 1694; also used in German), [203] sweating sickness , and Spanish fever (particularly for the 1918 flu pandemic strain). [204] Pandemics Further information: Influenza pandemic , Spanish flu , and Hong Kong flu The difference between the influenza mortality age distributions of the 1918 epidemic and normal epidemics. ... An overall lack of data up until 1500 precludes meaningful search for the influenza outbreaks in the more distant past. [206] Possibly the first influenza pandemic occurred around 6000 BC in China. [206] The symptoms of human influenza were clearly described by Hippocrates roughly 2,400 years ago. [207] [208] Although the virus seems to have caused epidemics throughout human history, historical data on influenza are difficult to interpret, because the symptoms can be similar to those of other respiratory diseases. [203] [209] The disease may have spread from Europe to the Americas as early as the European colonization of the Americas , since almost the entire indigenous population of the Antilles was killed by an epidemic resembling influenza that broke out in 1493, after the arrival of Christopher Columbus . [210] [211] The first convincing record of an influenza pandemic was a minor pandemic chronicled in 1510 , which began in East Asia before spreading to North Africa and then Europe. During this pandemic, influenza killed about 1% of its victims. [212] [213] The first pandemic of influenza to be reliably recorded as spreading worldwide was the 1557 influenza pandemic , [214] [215] [216] [217] in which a reoccurring wave likely killed Queen Mary I of England and the Archbishop of Canterbury within 12 hours of each other. [218] [219] One of the most well-chronicled pandemics of influenza in the 16th Century occurred in 1580, beginning in East Asia and spreading to Europe through Africa, Russia, and the Spanish and Ottoman Empires. ... As many as 25 million may have been killed in the first 25 weeks; in contrast, HIV/AIDS has killed 25 million in its first 25 years. [220] Later flu pandemics were not so devastating.DDX58, IFITM3, MX1, CXCL10, IRF7, LAMP3, CCL2, EIF2AK2, RSAD2, STAT1, ISG15, TNFSF10, IFIH1, PLSCR1, OAS2, IFIT5, ATF3, OAS1, IFI44L, TNFAIP6, APOL6, OASL, OAS3, DDX60, RTP4, HERC6, SLC22A8, IFI44, UBE2L6, ZCCHC2, SAMD9, XAF1, SERPING1, CCL8, SCO2, MX2, GBP1, PARP12, IFI6, HERC5, IFI27, IFIT3, XIST, TOR1B, IFI35, TRIM22, IFIT2, SIGLEC1, TDRD7, TREX1, IFIT1, LY6E, SFTPD, RAB39B, IL1B, IL2, IVNS1ABP, SARS2, ERVK-6, TNF, IFNG, IFNB1, IFNA13, IFNA1, PTPN11, IL10, ROBO3, PLAAT4, IL17A, SARS1, TLR4, IL6, HLA-A, PBRM1, TLR7, LINC01672, ERVK-32, TLR2, COPD, KRT31, CRP, ZMYND10, CD248, CPVL, TLR9, TLR3, VHLL, IRF3, HMOX1, CD40LG, MAPK1, LSAMP, IGHA1, IL22, ARIH1, CSF2, MAPK14, IL4, NLRP3, ACTB, PIK3CA, NR1I2, TRIM25, MED1, IL2RA, DOCK3, PPBP, ISG20, TMPRSS2, CASP1, ST14, IL33, GRN, PKD1, PEBP1, HLA-C, RNPC3, MYD88, NCR1, MAVS, DHX9, PRNP, MRC1, ACE2, GZMB, FOLH1, TRBV20OR9-2, MBL2, ICAM1, HSPA4, HCL2, RPS19, PIK3CG, IL27, POLDIP2, CCR5, CD28, GRAP2, CD80, CFTR, RNF19A, IL5, CRK, AHSA1, LOH19CR1, SRL, IL1A, CCR2, CXCL8, SARDH, PER2, AIMP2, IFNL1, ATN1, PIK3CD, IFNAR1, PIK3CB, EIF4G1, HLA-B, TLR5, PRDX2, CFH, HLA-DRB1, HMGB1, TNFRSF9, TXN, MYO1G, IL7R, ERVW-1, IL15, KRT32, NM, HCRT, EPHA3, NHS, EGFR, DHFR, ST6GAL1, CTLA4, RAB11A, CCL5, CD86, PLG, ANP32B, POTEF, CASP3, B3GAT1, CAP1, IL17D, C4BPA, PPARG, BST2, IRF9, ABCB6, ALB, CD274, PTGS2, SDS, CARD14, EPHB2, FPR2, MPO, SPINT1, CBLIF, CFAP97, GPI, SOD1, GABPA, XPO1, NFE2L2, COX2, MFAP1, FOXP3, IPO5, RELA, NS2, CMPK1, ICOS, PPIA, MMP9, SEC14L2, MPPE1, BRD4, LNPEP, LRIT1, TGFB1, NOS2, VTRNA1-1, STAT3, PAM, SEA, XCL1, GOLPH3, SERPINB6, LAMP1, LAMC2, MUC5AC, MUC1, SMS, MYDGF, NT5C2, PAGR1, RBM45, ANP32A, PRDM1, STING1, NR4A3, BCL2, AREG, EIF4A2, APRT, ESCO2, F2RL1, FGF2, MLANA, FN1, GAST, VTN, GALNS, GAPDH, RTL1, SLC9A6, CTAA1, TNFSF9, CD79A, HACD1, CDC42, IL18R1, SORBS1, TNFRSF18, MIR223, MBTPS1, NCR2, TNFSF13B, CLK1, IL32, CPT2, CD163, MIR155, MIR146A, RIPK3, ERVK-20, ABHD2, HLA-DQB1, TRAF6, DOT1L, TRAF3, MTCO2P12, ADAR, IFNA2, IFNAR2, IGF1, LINC02605, IL7, CXCR2, IL18, ILF3, ABO, ITGAE, ITGAM, SHCBP1, EBI3, TTR, TIRAP, LOC102724971, APCS, XCR1, BATF2, LOC102723407, ANXA1, UCK2, IL17F, SOCS3, MTSS2, ATG7, ZMPSTE24, RIDA, PRPF8, B3GNT3, FLVCR1, ATP2C1, RTN3, BET1, TRIM3, PPIE, DLL1, RBMS3, IL17C, CLEC10A, DISC1, TBK1, SLC35A1, IL37, NXF1, CFDP1, BAMBI, KHDRBS1, SLC27A4, IL24, TPPP, ADAMTS7, IRAK3, PADI4, CHP1, USP18, ARHGAP45, SRRM2, MORC3, ECD, P2RX2, SNRNP200, WDTC1, TRAM1, MPRIP, SIRT1, CLEC5A, BACE1, CXCR6, SLC27A5, PTPN22, CTCF, POLD3, PLK4, BACE2, CCL27, KLK5, LILRB1, MALT1, MCF2L, CPSF4, JTB, SUGT1, IL17RA, TMED2, CKAP4, SGK3, ABCA1, IL22RA1, CD207, MIR192, TICAM2, CCL4L1, PRSS57, LINC01194, MIR144, MIR15A, MIR184, MIR198, CYCSP51, MIR200C, MIR205, MIR206, MIR21, MIR29A, MIR29B1, MIR29B2, HLA-P, RAB7B, MIR30C1, NRSN1, TARS3, B4GALNT2, NMS, IL31RA, EGFLAM, ASZ1, TRIM69, MUC15, TREML4, TICAM1, DEFT1P, BCL6B, PTF1A, IFNL3, CLEC9A, BTBD8, MIR29C, MIR30C2, CTHRC1, ERVK-21, MFT2, MIR1260A, TMED7-TICAM2, PSMB8-AS1, P2RX5-TAX1BP3, ERVK-10, ERVK-9, ERVK-18, MIR744, ERVK-25, ERVK-24, MYMX, GATD3B, ERVK-19, CST12P, H3P24, EGOT, GGTLC4P, MIR31, MIR146B, MIR34A, MIR34C, DEFB103A, MIR328, ERVK-7, MIR451A, MIR485, MIR505, GGT2, ERVK-8, MIR483, GGTLC5P, H3P38, MIR449B, MUC5B, GGTLC3, IL22RA2, SLC46A1, GEMIN4, SMU1, UGT1A4, UGT1A1, UGT1A3, OTUD4, CASZ1, MARCHF1, NUDT11, PACC1, UGT1A5, ENAH, DEFB103B, LANCL2, CCL28, SPHK2, PNO1, SH3GLB2, UGT1A9, UGT1A6, CD177, BPIFA1, MBL3P, TMED5, TMED7, DYNC1LI1, LINC00328, VPS28, HSPA14, TLR8, UGT1A7, CRLF3, DDX41, ISYNA1, IL23A, DDIT4, UGT1A10, UGT1A8, CHPT1, AICDA, SCGB3A1, NLRC5, NDFIP1, NPL, ZBP1, UNC93B1, TLR10, TRIM56, PARP9, CHD6, DHDDS, GINS4, HOPX, MAK16, WNT3A, FRMD7, MCU, TRIM41, TARS2, NLRX1, GATAD2B, KLRG1, SEMA6A, ARHGAP21, SUGP1, HAMP, C6orf47, NLRC4, PRM3, HEATR6, DHX58, DMRTA1, TNMD, NOD2, CLEC7A, GORASP1, WNK1, WNK4, CALCOCO2, TARS1, DHRS2, ALYREF, GPT, CXCL1, CXCL2, GRP, PDIA3, GRSF1, GZMA, H1-2, HLA-DPB1, HMGCR, NR4A1, HNRNPK, HP, HPD, PRMT1, HES1, HSPA8, GPS1, CXCR3, GLRX, FUT2, EIF4E, EIF4G2, ENO1, ESR1, F2R, FCN2, FLT3LG, FYB1, GLDC, GAD1, GATA2, GATA3, GGT1, GH1, GLA, GLB1, HSPD1, TNC, IFNA6, EPCAM, KRT10, LAG3, LGALS9, LIF, LPO, BCAM, SH2D1A, SMAD3, KPNA4, MATN1, MAX, MBD1, MBP, MEFV, MAP3K5, MIF, KRT5, KPNA3, IFNGR1, ITGB2, IGHM, IL3, IL4R, CXCR1, IL13, INSR, IRF4, ITGB7, KPNA1, JAK3, KEL, KIR2DL1, KLK1, KLRB1, KLRC2, KLRD1, EIF4A1, S1PR1, DPEP1, CASP10, C3, C5, C5AR1, C6, CALCR, CAMK2B, CASP8, CAV1, BDNF, RUNX1T1, SERPINH1, CCK, CCND3, CCNT1, CD1A, CD2, CXCR5, BCR, CD14, ALK, ABL1, ACP3, AGA, JAG1, AHR, AKT1, ALDH2, ANXA2, BCL6, ANXA6, ANXA13, APC, BIRC3, XIAP, ARSF, BAG1, CD9, CD19, DYNC1LI2, CD55, CR2, CREB1, CREM, CSF3, CSF3R, CTNNB1, CYLD, DAP, CCR7, DDOST, DDX3X, DDX5, DEFA1, DEFB1, DLAT, DNM1, KLF6, CLCN7, CD27, CDK9, TNFRSF8, CD38, CD44, CD48, CD69, CD81, CDK1, CDKN1B, AP2M1, CDR1, CDSN, CEL, CENPF, CES1, AKR1C4, CISH, CXCL9, MIP, MPL, UGT1A, TIMP1, TNNI3, TOP1, TP53, HSP90B2P, TNFRSF4, TYR, KDM6A, TERT, UVRAG, VASP, VCP, VEGFA, VIM, BEST1, WAS, THBS1, TMBIM6, DNALI1, SNAI1, SRSF2, SRSF3, SFTPB, SGTA, ST3GAL3, SLC5A5, SLC20A1, SON, TCF7, SPR, ST13, STAT2, SYT1, TAP1, ABCA3, HNF1A, ZBTB25, CXCR4, SELL, CCL4L2, NTN1, GSTO1, AIM2, EIF2AK3, GAL3ST1, TECR, GOSR1, IKBKE, MAPKAPK2, SOCS5, NUP93, SPOCK2, TRIM14, SETDB1, BCAP31, TRIM28, TMPRSS11D, AURKB, RAB7A, PRPF18, DDX39B, PABPN1, IV, GATD3A, USP11, EPX, IFITM1, TP63, MYOM2, SOCS1, IL1RL2, SPHK1, HSPB3, CLDN2, P2RX6, PCSK7, SRSF1, SDC1, MSR1, PDR, PRDX1, SERPINE1, PAK1, PAX5, PDE7A, PDGFRB, PDPK1, PECAM1, PA2G4, PF4, ABCB1, PHB, PITX1, PKM, PKP2, PLS1, FURIN, P2RY2, POLR2A, CNOT4, COX1, MMUT, PPP1R12A, NAGA, NEU1, NFKBIB, NFKBIL1, NPY, P2RY1, NT5E, OSM, P2RX1, P2RX3, P2RX4, P2RX5, P2RX7, POLD1, POLR2B, CCL11, RPE65, PTK2, RAB5A, RAG1, RARA, RARB, DPF2, RNASE1, S100A8, PTEN, S100A11, SAA3P, SAFB, SAG, SATB1, CCL3, CCL4, PTGS1, PTBP1, POU1F1, MAP2K6, PPARA, PRD, PRKAA1, PRKAA2, PRKAB1, PRKCD, MAPK8, MAP2K7, PTAFR, PROC, PRSS8, PRTN3, PSMB8, PSMD2, PSMD4, PSMD10, H3P19
-
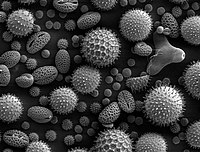
Allergic Rhinitis
Wikipedia
Human disease Allergic rhinitis Other names Hay fever, pollenosis Pollen grains from a variety of plants, enlarged 500 times and about 0.4 mm wide Specialty Allergy and immunology Symptoms Stuffy itchy nose, sneezing , red, itchy, and watery eyes, swelling around the eyes, itchy ears [1] Usual onset 20 to 40 years old [2] Causes Genetic and environmental factors [3] Risk factors Asthma , allergic conjunctivitis , atopic dermatitis [2] Diagnostic method Based on symptoms, skin prick test , blood tests for specific antibodies [4] Differential diagnosis Common cold [3] Prevention Exposure to animals early in life [3] Medication Nasal steroids , antihistamines such as diphenhydramine , cromolyn sodium , leukotriene receptor antagonists such as montelukast , allergen immunotherapy [5] [6] Frequency ~20% (Western countries) [2] [7] Allergic rhinitis , also known as hay fever , is a type of inflammation in the nose which occurs when the immune system overreacts to allergens in the air. [6] Signs and symptoms include a runny or stuffy nose, sneezing , red, itchy, and watery eyes, and swelling around the eyes. [1] The fluid from the nose is usually clear. [2] Symptom onset is often within minutes following allergen exposure and can affect sleep, and the ability to work or study. [2] [8] Some people may develop symptoms only during specific times of the year, often as a result of pollen exposure. [3] Many people with allergic rhinitis also have asthma , allergic conjunctivitis , or atopic dermatitis . [2] Allergic rhinitis is typically triggered by environmental allergens such as pollen, pet hair, dust, or mold. [3] Inherited genetics and environmental exposures contribute to the development of allergies. [3] Growing up on a farm and having multiple siblings decreases this risk. [2] The underlying mechanism involves IgE antibodies that attach to an allergen, and subsequently result in the release of inflammatory chemicals such as histamine from mast cells . [2] Diagnosis is typically based on a combination of symptoms and a skin prick test or blood tests for allergen-specific IgE antibodies. [4] These tests, however, can be falsely positive. [4] The symptoms of allergies resemble those of the common cold ; however, they often last for more than two weeks and typically do not include a fever . [3] Exposure to animals early in life might reduce the risk of developing these specific allergies. [3] Several different types of medications reduce allergic symptoms: including nasal steroids , antihistamines , such as diphenhydramine , cromolyn sodium , and leukotriene receptor antagonists such as montelukast . [5] Oftentimes, medications do not completely control symptoms, and they may also have side effects. [2] Exposing people to larger and larger amounts of allergen, known as allergen immunotherapy (AIT), is often effective. [6] The allergen can be given as an injection under the skin or as a tablet under the tongue. [6] Treatment typically lasts three to five years, after which benefits may be prolonged. [6] Allergic rhinitis is the type of allergy that affects the greatest number of people. [9] In Western countries, between 10 and 30% of people are affected in a given year. [2] [7] It is most common between the ages of twenty and forty. [2] The first accurate description is from the 10th-century physician Rhazes . [10] In 1859, Charles Blackley identified pollen as the cause. [11] In 1906, the mechanism was determined by Clemens von Pirquet . [9] The link with hay came about due to an early (and incorrect) theory that the symptoms were brought about by the smell of new hay. [12] [13] Contents 1 Signs and symptoms 2 Cause 3 Diagnosis 3.1 Classification 3.2 Local allergic rhinitis 4 Prevention 5 Treatment 5.1 Antihistamines 5.2 Steroids 5.3 Other 5.4 Allergen immunotherapy 5.5 Alternative medicine 6 Epidemiology 7 History 8 References 9 External links Signs and symptoms [ edit ] Illustration depicting inflammation associated with allergic rhinitis The characteristic symptoms of allergic rhinitis are: rhinorrhea (excess nasal secretion), itching , sneezing fits, and nasal congestion and obstruction. [14] Characteristic physical findings include conjunctival swelling and erythema , eyelid swelling with Dennie–Morgan folds , lower eyelid venous stasis (rings under the eyes known as " allergic shiners "), swollen nasal turbinates , and middle ear effusion. [15] There can also be behavioral signs; in order to relieve the irritation or flow of mucus, people may wipe or rub their nose with the palm of their hand in an upward motion: an action known as the "nasal salute" or the " allergic salute ". ... These methods include not having pets, not having carpets or upholstered furniture in the home, and keeping the home dry. [33] Specific anti-allergy zippered covers on household items like pillows and mattresses have also proven to be effective in preventing dust mite allergies. [25] Interestingly, studies have shown that growing up on a farm and having many older brothers and sisters can decrease an individual's risk for developing allergic rhinitis. [2] Studies in young children have shown that there is higher risk of allergic rhinitis in those who have early exposure to foods or formula and/or heavy exposure to cigarette smoking within the first year of life. [34] [35] Treatment [ edit ] The goal of rhinitis treatment is to prevent or reduce the symptoms caused by the inflammation of affected tissues. ... There is not enough evidence of antihistamine efficacy as an add-on therapy with nasal steroids in the management of intermittent or persistent allergic rhinitis in children, so its adverse effects and additional costs must be considered. [36] Ophthalmic antihistamines (such as azelastine in eye drop form and ketotifen ) are used for conjunctivitis, while intranasal forms are used mainly for sneezing, rhinorrhea, and nasal pruritus. [37] Antihistamine drugs can have undesirable side-effects, the most notable one being drowsiness in the case of oral antihistamine tablets. First-generation antihistamine drugs such as diphenhydramine cause drowsiness, while second- and third-generation antihistamines such as cetirizine and loratadine are less likely to. [37] Pseudoephedrine is also indicated for vasomotor rhinitis. ... Subcutaneous immunotherapy is the most common form and has the largest body of evidence supporting its effectiveness. [44] Alternative medicine [ edit ] There are no forms of complementary or alternative medicine that are evidence-based for allergic rhinitis. [25] Therapeutic efficacy of alternative treatments such as acupuncture and homeopathy is not supported by available evidence. [45] [46] While some evidence shows that acupuncture is effective for rhinitis, specifically targeting the sphenopalatine ganglion acupoint, these trials are still limited. [47] Overall, the quality of evidence for complementary-alternative medicine is not strong enough to be recommended by the American Academy of Allergy, Asthma and Immunology . [25] [48] Epidemiology [ edit ] Allergic rhinitis is the type of allergy that affects the greatest number of people. [9] In Western countries, between 10 and 30 percent of people are affected in a given year. [2] It is most common between the ages of twenty and forty. [2] History [ edit ] The first accurate description is from the 10th century physician Rhazes . [10] Pollen was identified as the cause in 1859 by Charles Blackley . [11] In 1906 the mechanism was determined by Clemens von Pirquet . [9] The link with hay came about due to an early (and incorrect) theory that the symptoms were brought about by the smell of new hay. [12] [13] References [ edit ] ^ a b "Environmental Allergies: Symptoms" .IL13, HRH1, IL4R, ABO, TLR1, MS4A2, SPINK5, RORA, FLG, PLCL1, PLCG2, SPPL3, PVT1, ZPBP2, ABCA1, FOXP3, IL33, ATXN2, FCER1G, DAW1, SYCP2L, JAZF1, SULT1A1, LINC00486, NKAIN3, HLA-B, COX4I2, TSLP, FTO, SMAD3, ASXL2, LPP, BACH2, NFATC2, PRDM16, LAMA3, NFKB1, IL17A, COL2A1, MFSD13A, RBFOX1, IL10, IL7R, IL5, IL4, PGM3, IFNG, TTC6, CARMIL2, LINC00299, DNAH11, BSND, RERE, AQP2, RTF1, PLA2G7, CLEC16A, SIK3, TNF, CDK2AP1, ST8SIA2, RAD50, ACTR1A, IL1RL1, LINC02341, DYRK4, DCAF1, LINC02240, LINC01426, IL18R1, GATA3, LEP, IL1B, ADAM33, TLR4, IL18, RNASE3, ACE, IL6, CXCL8, IL9, ANKHD1, ANKHD1-EIF4EBP3, STK26, TGFB1, SPP1, MMP9, TLR7, ICAM1, POSTN, IL17D, MYDGF, CASP1, ALRH, IL27, CCL11, TNFSF4, SCGB1A1, CTLA4, IL37, F2RL1, CD14, IFNA13, IFNA1, IL22, ARHGEF5, TLR2, TLR8, ADIPOQ, STAT6, IL12B, SERPINE1, TLR3, VEGFA, CCL5, TIMELESS, NOTCH1, FOXJ1, IL31, ENPP3, BCL2L12, PTGDR2, PLAT, HAVCR1, TAP1, TIMD4, CCR3, NLRP3, MUC5AC, SLC52A1, NR1I2, ANO1, TAC1, NGF, PTGS2, TRPV1, TLR6, CPSF4, OMP, PTPN22, PIK3CD, VIP, PIK3CB, MRPL4, PIK3CA, RETREG1, CCL26, EMSY, BPIFA1, CCL7, CYSLTR1, PIK3CG, CCL17, CD274, MAPK1, IL25, CSF2, CD86, IL2RA, EPHB2, IL1A, ECSCR, HMGB1, MIR202, CD19, HIF1A, NRG1, CLC, EZH2, FCRL3, MIR146A, FCER1A, BDNF, BLK, TSPO, MIR143, MIR155, AGT, CHRM3, JAG1, HRH4, CRLF2, AGXT, ISG20, IRF4, CHI3L1, MATN2, ALB, CST1, SFTPA2, SOSTDC1, MIR149, PSIP1, PADI4, SIRT1, CIC, MIRLET7E, GSTK1, NPSR1, SEC14L2, MIR15A, MIR126, PRDM10, GJB6, EBI3, DEFB4B, TBPL1, POLR1C, C20orf181, CCR2, BMS1, DLEC1, ABCB6, POTEF, CALCRL, MIR21, MIR487B, GSTT2B, SFTPA1, MIR375, SEMA3A, NOD1, MIR30A, DLC1, NXF1, MIR133B, CHIA, CLEC4D, HDAC11, IL23A, ORMDL3, ORAI1, HAVCR2, FAM167A, FCRL5, DUOX1, TLR10, TLR9, LPAL2, TET1, DHX40, NOX1, FEV, TET2, ADIPOR2, P2RY12, GAS5, SDAD1, SIGIRR, IL21, IL17RB, OSGEP, EAF2, IL17F, SCGB3A2, MRGPRX2, PIK3AP1, IFNL1, IFNL2, COPD, SIGLEC7, ODF2L, IFNLR1, SLC5A8, SIT1, KLB, ICOS, DUOX2, NOX4, IL23R, CDC42EP5, HT, DOCK11, SLCO6A1, IL31RA, RBM45, ADIPOR1, PHF11, IRAK4, SOCS4, PCYT1B, ADAM17, SOCS6, HCLS1, GSTT1, GSTP1, GRP, NR3C1, GJB2, CBLIF, FN1, FLNC, FLNB, FOXO3, FCGR3A, FCGR2B, F10, ETS1, EGR1, EDA, ATN1, HARS1, HDAC1, IL32, HDC, IDO1, IL13RA2, IL12RB2, IL12RB1, CXCR2, CXCR1, IL3, IL2RB, IL1RN, IGHE, IFNB1, HNMT, HLA-G, HLA-DRB1, HLA-DQB1, HLA-DQA1, HLA-DPB1, DPP4, DNMT3A, DNMT1, DNAH9, PRDM1, BCL6, BCL2, FAS, APOA2, AMY1C, AMY1B, AMY1A, ALK, AKR1B1, AHR, ADRB2, PARP1, ADAM10, ADAM8, ACTB, ACACA, CALCA, CALCR, CAT, CLDN4, DMBT1, DEFB4A, DEFB1, DECR1, CYBB, CUX1, CTBS, CCR4, CD1C, CHIT1, CDKN2A, CD69, CD40, ENTPD1, CD80, CD28, JAK1, KCNK2, KLRC1, SRSF5, UCN, TYRP1, TYRO3, TNFRSF4, TWIST1, TRAF6, TNFRSF1B, TNFAIP3, TLR5, TIMP1, TGFBR2, TCF3, TAP2, AOC1, STAT3, STAT1, SOAT1, UGT8, USF2, VDR, KHSRP, HGS, SOCS3, IL1RL2, DYNLL1, SOCS1, USO1, TNFSF11, KLF11, VIM, EPX, GAN, ADAM12, CXCR4, WNT2B, VIPR2, VIPR1, SFTPD, CCL24, KNG1, CCL20, NFIA, NEU2, NEU1, MTNR1A, MTHFR, COX2, MMP7, SCGB2A2, SCGB2A1, MC1R, MBL2, SMAD2, LTC4S, LOX, LGALS3, LCK, LBR, NOS2, NPY, NT5E, PTGDR, CCL13, CCL2, S100A7, RORC, RNASE2, RGS1, RAG2, PRKCD, OSM, PPARG, PPARA, POMC, PLAU, SLC26A4, PBX2, SERPINB2, MTCO2P12
-
Air Embolism
Wikipedia
If they are shunted to the systemic circulation through a patent foramen ovale they can travel to and lodge in the brain where they can cause stroke , the coronary capillaries where they can cause myocardial ischaemia or other tissues, where the consequences are usually less critical. The first aid treatment is to administer oxygen at the highest practicable concentration, treat for shock and transport to a hospital where therapeutic recompression and hyperbaric oxygen therapy are the definitive treatment. ... Early treatment has greatest benefits, but it can be effective as late as 30 hours after the injury. [5] Treatment of divers [ edit ] Oxygen first aid treatment is useful for suspected gas embolism casualties or divers who have made fast ascents or missed decompression stops. [24] Most fully closed-circuit rebreathers can deliver sustained high concentrations of oxygen-rich breathing gas and could be used as an alternative to pure open-circuit oxygen resuscitators . ... D. Vann; J. J. Freiberger (2007). "First aid normobaric oxygen for the treatment of recreational diving injuries" . ... Episode 1/4, "Amazing Grace," Shadow Chasers . First aired November 28, 1985. External links [ edit ] Arterial Gas Embolism Classification D ICD - 10 : O88.0 , T79.0 ICD - 9-CM : 673.0 , 999.1 MeSH : D004618 DiseasesDB : 313 SNOMED CT : 271376002 External resources eMedicine : emerg/787 v t e Pathology of pregnancy , childbirth and the puerperium Pregnancy Pregnancy with abortive outcome Abortion Ectopic pregnancy Abdominal Cervical Interstitial Ovarian Heterotopic Embryo loss Fetal resorption Molar pregnancy Miscarriage Stillbirth Oedema , proteinuria and hypertensive disorders Gestational hypertension Pre-eclampsia HELLP syndrome Eclampsia Other, predominantly related to pregnancy Digestive system Acute fatty liver of pregnancy Gestational diabetes Hepatitis E Hyperemesis gravidarum Intrahepatic cholestasis of pregnancy Integumentary system / dermatoses of pregnancy Gestational pemphigoid Impetigo herpetiformis Intrahepatic cholestasis of pregnancy Linea nigra Prurigo gestationis Pruritic folliculitis of pregnancy Pruritic urticarial papules and plaques of pregnancy (PUPPP) Striae gravidarum Nervous system Chorea gravidarum Blood Gestational thrombocytopenia Pregnancy-induced hypercoagulability Maternal care related to the fetus and amniotic cavity amniotic fluid Oligohydramnios Polyhydramnios Braxton Hicks contractions chorion / amnion Amniotic band syndrome Chorioamnionitis Chorionic hematoma Monoamniotic twins Premature rupture of membranes Obstetrical bleeding Antepartum placenta Circumvallate placenta Monochorionic twins Placenta accreta Placenta praevia Placental abruption Twin-to-twin transfusion syndrome Labor Amniotic fluid embolism Cephalopelvic disproportion Dystocia Shoulder dystocia Fetal distress Locked twins Nuchal cord Obstetrical bleeding Postpartum Pain management during childbirth placenta Placenta accreta Preterm birth Postmature birth Umbilical cord prolapse Uterine inversion Uterine rupture Vasa praevia Puerperal Breastfeeding difficulties Low milk supply Cracked nipples Breast engorgement Childbirth-related posttraumatic stress disorder Diastasis symphysis pubis Postpartum bleeding Peripartum cardiomyopathy Postpartum depression Postpartum psychosis Postpartum thyroiditis Puerperal fever Puerperal mastitis Other Concomitant conditions Diabetes mellitus Systemic lupus erythematosus Thyroid disorders Maternal death Sexual activity during pregnancy Category v t e Trauma Principles Polytrauma Major trauma Traumatology Triage Resuscitation Trauma triad of death Assessment Clinical prediction rules Revised Trauma Score Injury Severity Score Abbreviated Injury Scale NACA score Investigations Diagnostic peritoneal lavage Focused assessment with sonography for trauma Management Principles Advanced trauma life support Trauma surgery Trauma center Trauma team Damage control surgery Early appropriate care Procedures Resuscitative thoracotomy Pathophysiology Injury MSK Bone fracture Joint dislocation Degloving Soft tissue injury Resp Flail chest Pneumothorax Hemothorax Diaphragmatic rupture Pulmonary contusion Cardio Internal bleeding Thoracic aorta injury Cardiac tamponade GI Blunt kidney trauma Ruptured spleen Neuro Penetrating head injury Traumatic brain injury Intracranial hemorrhage Mechanism Blast injury Blunt trauma Burn Penetrating trauma Crush injury Stab wound Ballistic trauma Electrocution Region Abdominal trauma Chest trauma Facial trauma Head injury Spinal cord injury Demographic Geriatric trauma Pediatric trauma Complications Posttraumatic stress disorder Wound healing Acute lung injury Crush syndrome Rhabdomyolysis Compartment syndrome Contracture Volkmann's contracture Embolism air fat Chronic traumatic encephalopathy Subcutaneous emphysema v t e Underwater diving Diving modes Atmospheric pressure diving Freediving Saturation diving Scuba diving Snorkeling Surface oriented diving Surface-supplied diving Unmanned diving Diving equipment Cleaning and disinfection of personal diving equipment Human factors in diving equipment design Basic equipment Diving mask Snorkel Swimfin Breathing gas Bailout gas Bottom gas Breathing air Decompression gas Emergency gas supply Heliox Nitrox Oxygen Travel gas Trimix Buoyancy and trim equipment Buoyancy compensator Power inflator Dump valve Diving weighting system Ankle weights Integrated weights Trim weights Weight belt Decompression equipment Decompression buoy Decompression cylinder Decompression trapeze Dive computer Diving shot Jersey upline Jonline Diving suit Atmospheric diving suit Dry suit Sladen suit Standard diving suit Rash vest Wetsuit Dive skins Hot-water suit Helmets and masks Anti-fog Diving helmet Free-flow helmet Lightweight demand helmet Orinasal mask Reclaim helmet Shallow water helmet Standard diving helmet Diving mask Band mask Full-face mask Half mask Instrumentation Bottom timer Depth gauge Dive computer Dive timer Diving watch Helium release valve Pneumofathometer Submersible pressure gauge Mobility equipment Diving bell Closed bell Wet bell Diving stage Swimfin Monofin PowerSwim Towboard Diver propulsion vehicle Advanced SEAL Delivery System Cosmos CE2F series Dry Combat Submersible Human torpedo Motorised Submersible Canoe Necker Nymph R-2 Mala-class swimmer delivery vehicle SEAL Delivery Vehicle Shallow Water Combat Submersible Siluro San Bartolomeo Wet Nellie Wet sub Safety equipment Alternative air source Octopus regulator Pony bottle Bolt snap Buddy line Dive light Diver's cutting tool Diver's knife Diver's telephone Through-water communications Diving bell Diving safety harness Emergency gas supply Bailout block Bailout bottle Lifeline Screw gate carabiner Emergency locator beacon Rescue tether Safety helmet Shark-proof cage Snoopy loop Navigation equipment Distance line Diving compass Dive reel Line marker Surface marker buoy Silt screw Underwater breathing apparatus Atmospheric diving suit Diving cylinder Burst disc Diving cylinder valve Diving helmet Reclaim helmet Diving regulator Mechanism of diving regulators Regulator malfunction Regulator freeze Single-hose regulator Twin-hose regulator Full face diving mask Open-circuit scuba Scuba set Bailout bottle Decompression cylinder Independent doubles Manifolded twin set Scuba manifold Pony bottle Scuba configuration Sidemount Sling cylinder Diving rebreathers Carbon dioxide scrubber Carleton CDBA CDLSE Cryogenic rebreather CUMA DSEA Dolphin Electro-galvanic oxygen sensor FROGS Halcyon PVR-BASC Halcyon RB80 IDA71 Interspiro DCSC KISS LAR-5 LAR-6 LAR-V LARU Porpoise Ray Siebe Gorman CDBA Siva Viper Surface-supplied diving equipment Air line Diver's umbilical Diving air compressor Gas panel Hookah Scuba replacement Sea Trek Snuba Standard diving dress Escape set Davis Submerged Escape Apparatus Momsen lung Steinke hood Submarine Escape Immersion Equipment Diving equipment manufacturers AP Diving Apeks Aqua Lung America Aqua Lung/La Spirotechnique Beuchat René Cavalero Cis-Lunar Cressi-Sub Dacor DESCO Dive Xtras Divex Diving Unlimited International Drägerwerk Fenzy Maurice Fernez Technisub Oscar Gugen Heinke HeinrichsWeikamp Johnson Outdoors Mares Morse Diving Nemrod Oceanic Worldwide Porpoise Sub Sea Systems Shearwater Research Siebe Gorman Submarine Products Suunto Diving support equipment Access equipment Boarding stirrup Diver lift Diving bell Diving ladder Diving platform (scuba) Diving stage Downline Jackstay Launch and recovery system Messenger line Moon pool Breathing gas handling Air filtration Activated carbon Hopcalite Molecular sieve Silica gel Booster pump Carbon dioxide scrubber Cascade filling system Diver's pump Diving air compressor Diving air filter Water separator High pressure breathing air compressor Low pressure breathing air compressor Gas blending Gas blending for scuba diving Gas panel Gas reclaim system Gas storage bank Gas storage quad Gas storage tube Helium analyzer Nitrox production Membrane gas separation Pressure swing adsorption Oxygen analyser Oxygen compatibility Decompression equipment Built-in breathing system Decompression tables Diving bell Bell cursor Closed bell Clump weight Launch and recovery system Wet bell Diving chamber Diving stage Recreational Dive Planner Saturation system Platforms Dive boat Canoe and kayak diving Combat Rubber Raiding Craft Liveaboard Subskimmer Diving support vessel HMS Challenger (K07) Underwater habitat Aquarius Reef Base Continental Shelf Station Two Helgoland Habitat Jules' Undersea Lodge Scott Carpenter Space Analog Station SEALAB Tektite habitat Remotely operated underwater vehicles 8A4-class ROUV ABISMO Atlantis ROV Team CURV Deep Drone Épaulard Global Explorer ROV Goldfish-class ROUV Kaikō ROV Kaşif ROUV Long-Term Mine Reconnaissance System Mini Rover ROV OpenROV ROV KIEL 6000 ROV PHOCA Scorpio ROV Sea Dragon-class ROV Seabed tractor Seafox drone Seahorse ROUV SeaPerch SJT-class ROUV T1200 Trenching Unit VideoRay UROVs Safety equipment Diver down flag Diving shot Hyperbaric lifeboat Hyperbaric stretcher Jackstay Jonline Reserve gas supply General Diving spread Air spread Saturation spread Hot water system Sonar Underwater acoustic positioning system Underwater acoustic communication Freediving Activities Aquathlon Apnoea finswimming Freediving Haenyeo Pearl hunting Ama Snorkeling Spearfishing Underwater football Underwater hockey Underwater ice hockey Underwater rugby Underwater target shooting Competitions Nordic Deep Vertical Blue Disciplines Constant weight (CWT) Constant weight without fins (CNF) Dynamic apnea (DYN) Dynamic apnea without fins (DNF) Free immersion (FIM) No-limits apnea (NLT) Static apnea (STA) Skandalopetra diving Variable weight apnea (VWT) Variable weight apnea without fins Equipment Diving mask Diving suit Hawaiian sling Polespear Snorkel (swimming) Speargun Swimfins Monofin Water polo cap Freedivers Deborah Andollo Peppo Biscarini Sara Campbell Derya Can Göçen Goran Čolak Carlos Coste Robert Croft Mandy-Rae Cruickshank Yasemin Dalkılıç Leonardo D'Imporzano Flavia Eberhard Şahika Ercümen Emma Farrell Francisco Ferreras Pierre Frolla Flavia Eberhard Mehgan Heaney-Grier Elisabeth Kristoffersen Loïc Leferme Enzo Maiorca Jacques Mayol Audrey Mestre Karol Meyer Stéphane Mifsud Alexey Molchanov Natalia Molchanova Dave Mullins Patrick Musimu Guillaume Néry Herbert Nitsch Umberto Pelizzari Annelie Pompe Michal Risian Stig Severinsen Tom Sietas Aharon Solomons Martin Štěpánek Walter Steyn Tanya Streeter William Trubridge Devrim Cenk Ulusoy Danai Varveri Alessia Zecchini Nataliia Zharkova Hazards Barotrauma Drowning Freediving blackout Deep-water blackout Shallow-water blackout Hypercapnia Hypothermia Historical Ama Octopus wrestling Swimming at the 1900 Summer Olympics – Men's underwater swimming Organisations AIDA International Scuba Schools International Australian Underwater Federation British Freediving Association Confédération Mondiale des Activités Subaquatiques Fédération Française d'Études et de Sports Sous-Marins Performance Freediving International Professional diving Occupations Ama Commercial diver Commercial offshore diver Hazmat diver Divemaster Diving instructor Diving safety officer Diving superintendent Diving supervisor Haenyeo Media diver Police diver Public safety diver Scientific diver Underwater archaeologist Military diving Army engineer diver Clearance diver Frogman List of military diving units Royal Navy ships diver Special Boat Service United States military divers U.S. ... Vandenberg HMS Ghurka Glen Strathallan SAS Good Hope Gothenburg Herzogin Cecilie Hilma Hooker Hispania HMS Hood HMAS Hobart Igara James Eagan Layne Captain Keith Tibbetts King Cruiser SMS Kronprinz Kyarra HMS Laforey USAT Liberty Louis Sheid USS LST-507 SMS Markgraf Mikhail Lermontov HMS M2 Maine Maloja HMS Maori Marguerite SS Mauna Loa USAT Meigs Mendi USCGC Mohawk Mohegan RMS Moldavia HMS Montagu MV RMS Mulheim Nagato Oceana USS Oriskany Oslofjord P29 P31 Pedernales Persier HMAS Perth SAS Pietermaritzburg Piłsudski Pool Fisher HMS Port Napier Preußen President Coolidge PS Queen Victoria Radaas Rainbow Warrior RMS Rhone Rondo Rosehill Rotorua Royal Adelaide Royal Charter Rozi HMS Safari Salem Express USS Saratoga USS Scuffle HMS Scylla HMS Sidon USS Spiegel Grove Stanegarth Stanwood Stella HMAS Swan USS Tarpon Thesis Thistlegorm Toa Maru Torrey Canyon SAS Transvaal U-40 U-352 U-1195 Um El Faroud Varvassi Walter L M Russ Washingtonian (1913) HMNZS Wellington USS Yancey Yongala Zenobia Zealandia Zingara Cave diving sites Blauhöhle Chinhoyi Caves Devil's Throat at Punta Sur Engelbrecht Cave Fossil Cave Jordbrugrotta Piccaninnie Ponds Pluragrotta Pollatoomary Sistema Ox Bel Ha Sistema Sac Actun Sistema Dos Ojos Sistema Nohoch Nah Chich Freshwater dives Dutch Springs Ewens Ponds Little Blue Lake Training sites Capernwray Dive Centre Deepspot National Diving and Activity Centre Stoney Cove Open ocean diving Blue-water diving Black-water diving Diving safety Human factors in diving equipment design Human factors in diving safety Life-support system Safety-critical system Scuba diving fatalities Diving hazards List of diving hazards and precautions Environmental Current Delta-P Entanglement hazard Overhead Silt out Wave action Equipment Freeflow Use of breathing equipment in an underwater environment Failure of diving equipment other than breathing apparatus Single point of failure Physiological Cold shock response Decompression Nitrogen narcosis Oxygen toxicity Seasickness Uncontrolled decompression Diver behaviour and competence Lack of competence Overconfidence effect Panic Task loading Trait anxiety Willful violation Consequences Barotrauma Decompression sickness Drowning Hypothermia Hypoxia Hypercapnia Hyperthermia Diving procedures Ascending and descending Emergency ascent Boat diving Canoe and kayak diving Buddy diving buddy check Decompression Decompression practice Pyle stop Ratio decompression Dive briefing Dive log Dive planning Scuba gas planning Diver communications Diving hand signals Diving line signals Diver voice communications Diver rescue Diver training Doing It Right Drift diving Gas blending for scuba diving Night diving Solo diving Water safety Risk management Checklist Hazard identification and risk assessment Hazard analysis Job safety analysis Risk assessment Risk control Hierarchy of hazard controls Incident pit Lockout–tagout Permit To Work Redundancy Safety data sheet Situation awareness Diving team Bellman Chamber operator Diver medical technician Diver's attendant Diving supervisor Diving systems technician Gas man Life support technician Stand-by diver Equipment safety Breathing gas quality Testing and inspection of diving cylinders Hydrostatic test Sustained load cracking Diving regulator Breathing performance of regulators Occupational safety and health Approaches to safety Job safety analysis Risk assessment Toolbox talk Housekeeping Association of Diving Contractors International Code of practice Contingency plan Diving regulations Emergency procedure Emergency response plan Evacuation plan Hazardous Materials Identification System Hierarchy of hazard controls Administrative controls Engineering controls Hazard elimination Hazard substitution Personal protective equipment International Marine Contractors Association Occupational hazard Biological hazard Chemical hazard Physical hazard Psychosocial hazard Occupational hygiene Exposure assessment Occupational exposure limit Workplace health surveillance Safety culture Code of practice Diving safety officer Diving superintendent Health and safety representative Operations manual Safety meeting Standard operating procedure Diving medicine Diving disorders List of signs and symptoms of diving disorders Cramp Motion sickness Surfer's ear Pressure related Alternobaric vertigo Barostriction Barotrauma Air embolism Aerosinusitis Barodontalgia Dental barotrauma Pulmonary barotrauma Compression arthralgia Decompression illness Dysbarism Oxygen Freediving blackout Hyperoxia Hypoxia Oxygen toxicity Inert gases Avascular necrosis Decompression sickness Isobaric counterdiffusion Taravana Dysbaric osteonecrosis High-pressure nervous syndrome Hydrogen narcosis Nitrogen narcosis Carbon dioxide Hypercapnia Hypocapnia Breathing gas contaminants Carbon monoxide poisoning Immersion related Asphyxia Drowning Hypothermia Immersion diuresis Instinctive drowning response Laryngospasm Salt water aspiration syndrome Swimming-induced pulmonary edema Treatment Demand valve oxygen therapy First aid Hyperbaric medicine Hyperbaric treatment schedules In-water recompression Oxygen therapy Therapeutic recompression Personnel Diving Medical Examiner Diving Medical Practitioner Diving Medical Technician Hyperbaric nursing Screening Atrial septal defect Effects of drugs on fitness to dive Fitness to dive Psychological fitness to dive Research Researchers in diving physiology and medicine Arthur J.
-
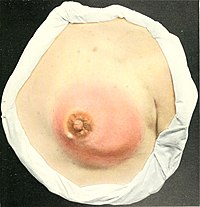
Mastitis
Wikipedia
Mastitis Other names Mammitis A drawing of mastitis from the early 1900s Pronunciation / m æ s t ˈ aɪ t ɪ s / Specialty Gynecology Symptoms Localized breast pain and redness, fever [1] Complications Abscess [2] Usual onset Rapid [1] Diagnostic method Based on symptoms [2] Differential diagnosis Plugged milk duct, [3] breast engorgement , [4] breast cancer (rare) [1] Prevention Frequent breastfeeding with good technique [2] Treatment Antibiotics ( cephalexin ), ibuprofen [2] [1] Frequency 10% of breastfeeding women [2] Mastitis is inflammation of the breast or udder , usually associated with breastfeeding . [1] [5] [6] Symptoms typically include local pain and redness. [1] There is often an associated fever and general soreness. [1] Onset is typically fairly rapid and usually occurs within the first few months of delivery. [1] Complications can include abscess formation. [2] Risk factors include poor latch , cracked nipples , use of a breast pump , and weaning . [1] The bacteria most commonly involved are Staphylococcus and Streptococci . [1] Diagnosis is typically based on symptoms. [2] Ultrasound may be useful for detecting a potential abscess. [1] Prevention is by proper breastfeeding techniques. [2] When infection is present, antibiotics such as cephalexin may be recommended. [2] Breastfeeding should typically be continued, as emptying the breast is important for healing. [2] [1] Tentative evidence supports benefits from probiotics . [1] About 10% of breastfeeding women are affected. [2] Contents 1 Signs and symptoms 1.1 Breast abscess 2 Causes 2.1 Risk factors 2.2 Infection 3 Types 3.1 Pregnancy related 3.2 Non pregnancy related 4 Diagnosis 4.1 Differential diagnosis 5 Treatment 5.1 Antibiotics 5.2 Breast abscess 6 Prognosis 7 Epidemiology 8 Terminology 8.1 Etymology and pronunciation 9 Other animals 10 References 11 External links Signs and symptoms [ edit ] Mastitis localized on the underside of the breast, with a large area of inflammation. ... Some women may also experience flu -like symptoms such as: Aches Shivering and chills Feeling anxious or stressed Fatigue [9] Contact should be made with a health care provider with special breastfeeding competence as soon as the patient recognizes the combination of signs and symptoms. Most of the women first experience the flu-like symptoms and just after they may notice a sore red area on the breast. ... Most mothers who develop mastitis usually do so within the first few weeks after delivery. Most breast infections occur within the first or second month after delivery or at the time of weaning . [20] However, in rare cases it affects women who are not breastfeeding. [52] Terminology [ edit ] Popular usage of the term mastitis varies by geographic region.CXCR2, TLR4, TLR2, SLC9A6, IL6, TNF, IFNG, NLRP3, IL1B, TGFB1, PTX3, ANGPTL2, LYZ, CXCL8, PLA2G1B, MIR223, MIR15A, SCD, RPS6KA3, RASGRP1, SAG, RGS6, MAP4K4, SET, CXCL12, DGAT1, CAVIN2, YWHAZ, TP53, TNFRSF1B, CCL4, CD163, A2M, SPINK5, PHB2, DEFB103A, MIR182, MIR155, MIR142, MIR122, PLB1, CYP2R1, ZC3H12A, PAGR1, SIL1, SIGIRR, DEFB103B, CRLS1, SIRT7, ANGPTL3, TNFRSF21, PLA2G2D, AMACR, UFL1, RASA1, PLG, PPBP, FGF2, HMGB3, HMGB1, NR3C1, B4GALT1, GALNS, GABPA, GAST, MTOR, FGF12, SLC26A2, HSPA5, DOCK3, CYP24A1, CYP1A1, CSF3, CRP, COL1A1, CD14, CFB, ALCAM, HMOX1, ICAM1, MED1, LTF, PPARG, ABO, PKD1, PEBP1, NHS, NFE2L2, NCF4, RNR1, MPO, LRP5, IL1A, LPO, LPL, JAK2, ITIH4, ITGAM, IRAK2, IL17A, IL6R, IL2, SFTPA1
-
Mucolipidosis Iii Alpha/beta
Omim
In Freiburg, Germany, Schinz and Furtwaengler (1928) described a sibship of 11, the offspring of a first-cousin marriage, in which a man then 29 years old and 3 of his sisters were identically affected by a disorder in which a striking feature was stiff joints. ... The authors stated that this was the first example of the disease presenting in an adult patient.
-
C. Difficile Infection
Mayo_clinic
However, they may occur as soon as the first day or up to three months later. ... If you aren't hungry, you may need a liquid diet at first. After your diarrhea clears up, you may have temporary difficulty digesting milk and milk-based products.
-
Thyrotoxic Myopathy
Wikipedia
Extensive clinical tests are performed first to determine if there is a neuromuscular disorder and then to determine which disorder it is. ... This can be accomplished three ways including using medication, radiation, and surgery. [ citation needed ] The first choice involves using medications to alleviate the symptoms and reverse the damage by blocking the production of thyroxine from the thyroid gland.
-
Membranous Glomerulonephritis
Wikipedia
Given spontaneous remission is common, international guidelines recommend a period of watchful waiting before considering immunosuppressive treatment. [16] Likelihood of achieving spontaneous remission is much higher if anti-proteinuric therapy with ace inhibitors or angiotensin II receptor blockers is commenced. Recommended first line immunsosuppressive therapy often includes: cyclophosphamide alternating with a corticosteroid , [17] also known as the Ponticelli regime. ... The twin aims of treating membranous nephropathy are first to induce a remission of the nephrotic syndrome and second to prevent the development of end-stage kidney failure.C3, HLA-DQA1, ALB, HLA-DRB1, APOA1, GAA, NPHS1, LRP2, NQO1, CDKN1B, NPHS2, CFH, APOE, PTPRU, IL1B, MAP3K5, PLG, ABCA1, PTGER3, LRPAP1, SPARC, TBXAS1, MMP9, A2M, CD40, RHOA, C7, TSBP1, TSBP1-AS1, PPT2-EGFL8, SFTA2, THSD7A, PSORS1C1, PLB1, MUCL3, PLA2G1B, EGFL8, POU5F1, PRKCD, PPT2, IGAN1, RNF5, BTNL2, FOXP3, TCF19, PLA2R1, YWHAZ, EHMT2, PRRC2A, GPANK1, STK19, HLA-DQA2, SLC7A7, EHMT2-AS1, HLA-DMB, CYP21A2, HLA-B, ACTN4, MS4A1, KRT20, RBM45, MBL2, TRPC6, TNF, TGFB1, HLA-A, PLA2G2A, SERPINE1, XIST, F5, TNFRSF12A, MTHFR, HPSE, VEGFA, PLA2G6, SYNPO, POMC, IFNG, ACTB, AGT, MIR217, IL6, CST3, CNTN1, MIR130A, NES, TNFSF13B, CP, P3H4, MIR186, ANP32B, CIB1, C5AR1, MIR193A, CCR6, DNM1L, KEAP1, CCN2, PTER, USP2, POTEF, CTH, SNURF, PER2, CTLA4, HELT, MLYCD, CIC, CLCN5, CXCR5, KLHDC8B, NLRP3, CHRDL1, BRSK1, APOH, RABEP2, PDLIM2, CD69, NPNT, ACE2, PDGFC, CD5L, NEAT1, LINC01193, TNFSF11, CDC42BPG, TLR9, FIS1, CLU, MBL3P, KLF15, DIANPH, CABIN1, TNFSF13, HLA-DQB1, APOL1, MIF, FN1, PITX1, PECAM1, GABPA, NOTCH1, NOS3, NFE2L2, NEFH, MYC, MUC1, MTNR1A, MPO, GLS, GNAO1, UBL4A, SMAD7, STMN1, JAK3, CXCL10, IL4, IL2, HLA-DMA, IKBKB, IGHA1, IFI27, HSPG2, HRAS, HLA-DRB3, EXT2, PPBP, PRKCA, EXT1, FOSL1, CTSL, CYP3A5, ACE, HLA-DQB2, VCL, UCHL1, UBE2V1, TLR4, THY1, TGFB2, DNMT1, EGFR, TAP1, STAT4, EIF4A2, SNRPN, SMN2, SMN1, CXCL12, SDC2, CCL2, EIF4E, REN, EIF4G1, PSMB8, ENO1, PRKCB
-
Thought Insertion
Wikipedia
Thought insertion, along with thought broadcasting , thought withdrawal , thought blocking and other first rank symptoms , is a primary symptom and should not be confused with the delusional explanation given by the respondent. ... Neurology [ edit ] Identifying brain regions associated with thought insertion has proven difficult. First, it is difficult to find subjects who experience thought insertion frequently.
-
Diastasis Recti
Wikipedia
Additional causes can be attributed to excessive abdominal exercises after the first trimester of pregnancy. [4] Strength training of all the core muscles, including the abdominis recti muscle, may or may not reduce the size of the gap in pregnant or postpartum women. ... After delivery - Typically the separation of the abdominal muscles will lessen in the mother within the first 8 weeks after childbirth; however, the connective tissue remains stretched for many.
-
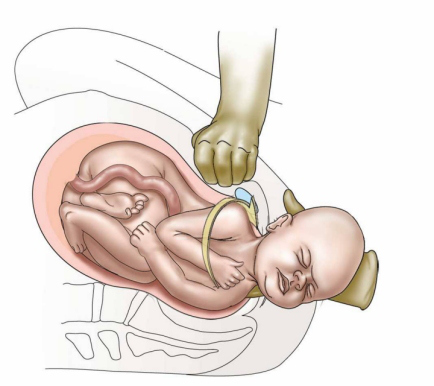
Shoulder Dystocia
Wikipedia
The ventral roots (motor pathway) are most prone to injury. [ citation needed ] The cause of injury to the baby is debated, [ citation needed ] but a probable mechanism is manual stretching of the nerves, which in itself can cause injury. [ citation needed ] Excess tension may physically tear the nerve roots out from the neonatal spinal column, resulting in total dysfunction. [ citation needed ] Possible complications include: Neonatal complications: Klumpke paralysis Erb's palsy Hypoxia Death Cerebral palsy Maternal complications: [5] Postpartum bleeding (11%) Perineal lacerations that extend into the anal sphincter Pubic symphysis separation Neuropathy of lateral femoral cutaneous nerve Uterine rupture Risk factors [ edit ] About 16% of deliveries where shoulder dystocia occurs have conventional risk factors. [ citation needed ] These include diabetes , [6] fetal macrosomia , and maternal obesity . [7] [8] Risk factors: [9] Age >35 Short in stature Small or abnormal pelvis More than 42 weeks gestation Estimated fetal weight >4,500 g Maternal diabetes (2–4 fold increase in risk) Factors which increase the risk/are warning signs: [ citation needed ] Need for oxytocics Prolonged first or second stage of labour Turtle sign (head bobbing in the second stage) Failure to restitute No shoulder rotation or descent Instrumental delivery For women with a previous shoulder dystocia, the risk of recurrence is at least 10%. [5] Management [ edit ] The steps to treating a shoulder dystocia are outlined by the mnemonic ALARMER: [10] A sk for help. [2] This involves asking for the help of an obstetrician, anesthesia, and for pediatrics for subsequent resuscitation of the infant that may be needed if the methods below fail; L eg hyperflexion and abduction at the hips ( McRoberts maneuver ); [2] A nterior shoulder disimpaction (suprapubic pressure); [10] R otation of the shoulder ( Rubin maneuver ); [10] M anual delivery of posterior arm; [10] E pisiotomy; [10] R oll over on all fours. [10] Typically the procedures are performed in the order listed and the sequence ends whenever a technique is successful. [10] Intentional fracturing of the clavicle is another possibility at non-operative vaginal delivery prior to Zavanelli's maneuver or symphysiotomy , both of which are considered extraordinary treatment measures. ... The technique is effective in about 42% of cases; Suprapubic pressure (or Rubin I); [14] Rubin II or posterior pressure on the anterior shoulder , which would bring the baby into an oblique position with the head somewhat towards the vagina; [15] Active delivery of the anterior arm Step 1: Index and middle fingers insertion with the hand opposite the baby's face Step 2: Baby's head slightly tilted downward with the free hand Step 3: Two fingers are placed on the humerus like a splint Step 4: Baby's hand appears under the maternal pubic symphysis, allowing the anterior arm to be delivered Wood's screw maneuver which leads to turning the anterior shoulder to the posterior and vice versa (somewhat the opposite of Rubin II maneuver); [16] Jacquemier's maneuver (also called Barnum's maneuver), or delivery of the posterior shoulder first, in which the forearm and hand are identified in the birth canal, and gently pulled; Gaskin maneuver involves moving the mother to an all fours position with the back arched, widening the pelvic outlet. [17] [18] More drastic maneuvers include: Zavanelli's maneuver , which involves pushing the baby's head back in (internal cephalic replacement) followed by a cesarean section ; [19] Intentional causing clavicular fractures , which reduces the diameter of the shoulders that requires to pass through the birth canal; [2] Maternal symphysiotomy , which makes the opening of the birth canal laxer by breaking the connective tissue between the two pubes bones; [2] Abdominal rescue, described by O'Shaughnessy, where a hysterotomy facilitates vaginal delivery of the impacted shoulder. [20] Epidemiology [ edit ] Shoulder dystocia occurs in about 0.15% to 4% of term vaginal births. [21] References [ edit ] ^ a b c d e f g Gherman, Robert B.; Gonik, Bernard (2009).
-
Hypomania
Wikipedia
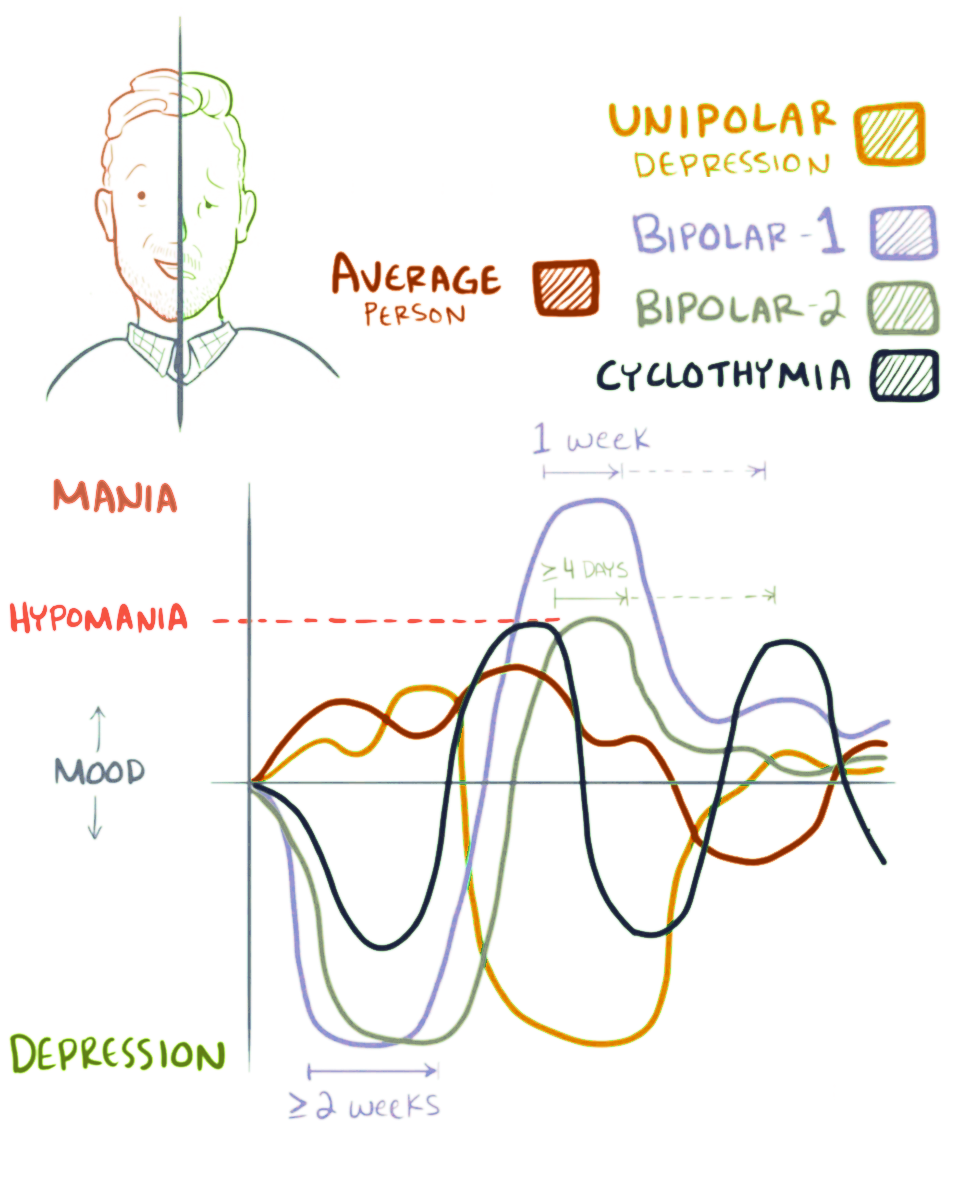
Other symptoms related to this may include feelings of grandiosity , distractibility , and hypersexuality . [1] While hypomanic behavior often generates productivity and excitement, it can become troublesome if the subject engages in risky or otherwise inadvisable behaviors, and/or the symptoms manifest themselves in trouble with everyday life events. [2] When manic episodes are separated into stages of a progression according to symptomatic severity and associated features, hypomania constitutes the first stage of the syndrome, wherein the cardinal features ( euphoria or heightened irritability, pressure of speech and activity, increased energy, decreased need for sleep, and flight of ideas) are most plainly evident. ... In such cases, one speaks of a "seasonal pattern". [11] If left untreated, and in those so predisposed, hypomania may transition into mania , which may be psychotic , in which case bipolar I disorder is the correct diagnosis. [12] Causes [ edit ] Often in those who have experienced their first episode of hypomania – generally without psychotic features – there may be a long or recent history of depression or a mix of hypomania combined with depression (known as mixed-state) prior to the emergence of manic symptoms.