-
Multisystem Inflammatory Syndrome In Children
Wikipedia
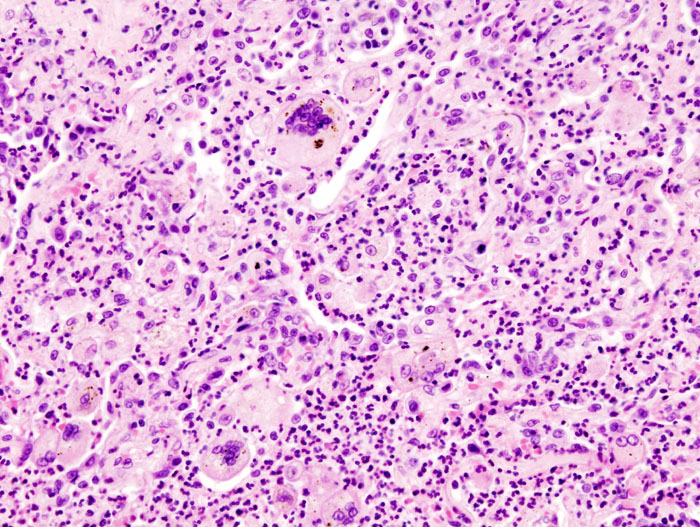
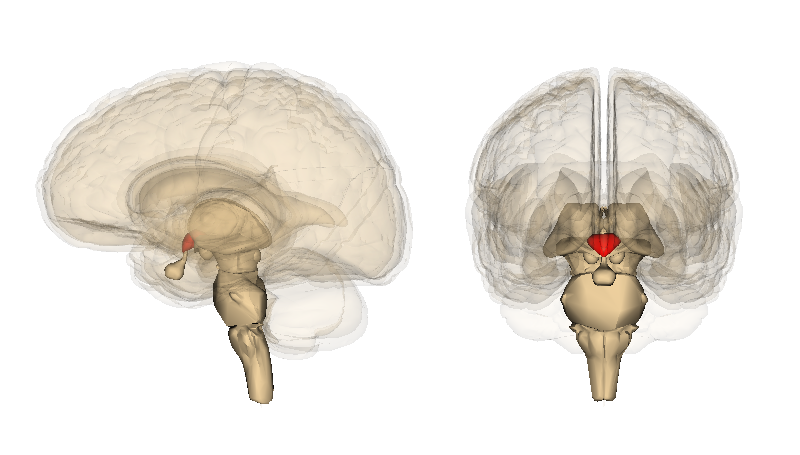
Disease of children; pediatric comorbidity from COVID-19 Paediatric multisystem inflammatory syndrome (PMIS/PIMS/PIMS-TS) Other names Multisystem inflammatory syndrome in children (MIS-C) [1] Multisystem inflammatory syndrome (MIS) in children and adolescents temporally related to COVID-19 [2] Paediatric inflammatory multisystem syndrome (PIMS), temporally associated with SARS-CoV-2 infection (PIMS-TS) [3] Kawa-COVID-19 [4] TEM image of SARS-CoV-2 , the coronavirus responsible for COVID-19 : PMIS / MIS-C is thought to be caused by an unusual biological response to infection in certain children Specialty Paediatrics Symptoms Fever , abdominal pain , diarrhoea / vomiting , low blood pressure , insufficient blood supply (shock) , pink eye , " strawberry tongue ", rashes , large lymph nodes , swollen hands/feet , neurological disturbances , among others Complications Cardiac dysfunction ; coronary artery abnormalities , including aneurysms ; acute kidney injury ; coagulopathy Usual onset typically 2–6 weeks [5] after COVID-19 exposure Causes Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Diagnostic method Clinical evaluation by specialists Differential diagnosis Alternative infectious/non-infectious causes, Kawasaki disease Treatment Intravenous immunoglobulin (IVIG); corticosteroids ; oxygen , supportive care Prognosis Response to treatment, generally good; long-term prognosis, unclear [6] Frequency Rare Deaths <2% of reported cases Multisystem inflammatory syndrome in children ( MIS-C ), or paediatric inflammatory multisystem syndrome ( PIMS / PIMS-TS ), is a rare systemic illness involving persistent fever and extreme inflammation following exposure to SARS-CoV-2 , the virus responsible for COVID-19 . [6] It can rapidly lead to medical emergencies such as insufficient blood flow around the body (a condition known as shock ). [6] Failure of one or more organs can occur. [7] A warning sign is unexplained persistent fever with severe symptoms following exposure to COVID-19. [8] Prompt referral to paediatric specialists is essential, and families need to seek urgent medical assistance. [6] Most affected children will need intensive care . [6] All affected children have persistent fever. [6] Other clinical features vary. [8] The first symptoms often include acute abdominal pain with diarrhoea or vomiting . [6] Muscle pain and general tiredness are frequent, [6] and low blood pressure is also common. [9] Symptoms can also include pink eye , rashes , enlarged lymph nodes , swollen hands and feet , and " strawberry tongue ". [5] Various mental disturbances are possible. [5] A cytokine storm may take place, [10] in which the child's innate immune system stages an excessive and uncontrolled inflammatory response. [11] Heart failure is common. [9] Clinical complications can include damage to the heart muscle , respiratory distress , acute kidney injury , and increased blood coagulation . [12] Coronary artery abnormalities can develop (ranging from dilatation to aneurysms ). [5] This life-threatening disease has proved fatal in under 2% of reported cases. [6] Early recognition and prompt specialist attention are essential. [13] Anti-inflammatory treatments have been used, with good responses being recorded for intravenous immunoglobulin (IVIG), with or without corticosteroids . [14] Oxygen is often needed. [6] Supportive care is key for treating clinical complications. [12] Most children who receive expert hospital care survive. [6] Knowledge of this newly described syndrome is evolving rapidly. [15] Its clinical features may appear somewhat similar to Kawasaki disease , a rare disease of unknown origin that typically affects young children, in which blood vessels become inflamed throughout the body. [9] It can also show features of other serious inflammatory conditions of childhood, including toxic shock and macrophage activation syndromes. [9] Nevertheless, it appears to be a separate syndrome. [16] Older children tend to be affected. [17] This emerging condition has been defined slightly differently (using different names), by the World Health Organization (WHO), [18] the Royal College of Paediatrics and Child Health (RCPCH), [7] and the Centers for Disease Control and Prevention (CDC). [1] Although the condition is thought to follow SARS-CoV-2 viral infection, antigen or antibody tests are not always positive. [3] Exclusion of alternative causes, including bacterial and other infections, is essential for differential diagnosis . [3] Some general clinical guidance has been provided by the RCPCH, [7] the National Institutes of Health , [17] the American College of Rheumatology , [19] and the American Academy of Pediatrics . [20] Clusters of new cases have been reported 2–6 weeks after local peaks in viral transmission. [5] The disease is thought to be driven by a delayed biological mechanism in certain predisposed children. [14] The European Centre for Disease Prevention and Control (ECDC) has rated risk to children in Europe as being 'low' overall, based on a 'very low' likelihood of a child developing this 'high impact' disease. [3] Regarding ethnicity , the condition seems to affect more children of African , Afro-Caribbean , and Hispanic descent, whereas Kawasaki disease affects more of East Asian ancestry. [13] Initial reports regarded children in various parts of Europe and the United States, and it was unclear to what extent the condition had gone unrecognized elsewhere. [18] Reports have since emerged of cases in various other countries around the world. [21] [22] In adults, a similar condition has occasionally been reported, which has been called multisystem inflammatory syndrome in adults ( MIS-A ). [23] Contents 1 Name 2 Background 3 Characteristics 3.1 Clinical course 4 Diagnosis 4.1 Case definitions and guidance 4.2 Differential diagnosis 5 Treatment 6 Causes 7 Mechanism 8 Epidemiology 8.1 In adults 9 History 10 Notes 11 References 12 External links Name [ edit ] The disorder has been called by various names, including: Multisystem inflammatory syndrome in children (MIS-C) [1] Multisystem inflammatory syndrome (MIS) in children and adolescents temporally related to COVID-19 [2] Paediatric inflammatory multisystem syndrome (PIMS) [7] Paediatric inflammatory multisystem syndrome, temporally associated with SARS-CoV-2 infection (PIMS-TS) [3] [6] Paediatric multisystem inflammatory syndrome (PMIS) [9] Kawa-COVID-19 [4] Background [ edit ] Symptomatic cases of COVID-19 in children have been relatively uncommon, [24] possibly because they generally experience milder disease. [25] Early infection tends to be associated with mild or no symptoms, while the later pulmonary phase, which can be life-threatening in adults, is usually mild or absent. [26] [27] While cases of children with severe symptoms are exceptional, they can occasionally require intensive care. [28] [29] [30] Fatalities have been rare. [27] [31] In April 2020, a small group of children with evidence of SARS-CoV-2 infection or exposure to COVID-19 were found to display clinical features corresponding to the diagnostic criteria of Kawasaki disease , sometimes accompanied by shock. [28] [32] Kawasaki disease is a rare syndrome which mainly affects young children (adult onset has occasionally been reported [33] ). [3] [34] [35] It is a form of vasculitis , where blood vessels become inflamed throughout the body, and it results in a persistent fever . [3] Recovery typically occurs spontaneously , though some children later develop mid-sized or giant coronary artery aneurysms in the heart – a potentially fatal complication. [3] [36] Symptoms of toxic shock (a syndrome caused by bacterial toxins) occasionally occur – an association sometimes referred to as 'Kawasaki shock syndrome', [37] which is characterized by systolic hypotension or signs of poor perfusion . [3] [38] While the exact cause of Kawasaki disease is unknown, one plausible explanation is that it may stem from an infection triggering an autoimmune and/or autoinflammatory response in children who are genetically predisposed . [39] [40] No specific diagnostic test exists for Kawasaki disease, and its recognition is based on various combinations of clinical and laboratory findings (including persistent fever, widespread rashes , enlarged lymph nodes , conjunctivitis , changes to the mucous membranes , and swollen hands and feet ). [3] [34] [41] Characteristics [ edit ] MIS-C / PIMS-TS is a systemic disorder involving persistent fever, extreme [6] inflammation (hyperinflammation), and organ dysfunction , which is temporally associated with exposure to COVID-19. [1] [7] Onset may be delayed or contemporary with ongoing SARS-CoV-2 infection, [42] which may pass without symptoms . [6] The time the syndrome takes to appear following the initial viral infection is debated, though it may develop between the first and second week. [43] Epidemiological data suggest that recognition of the disease may typically be delayed by 2–6 weeks, [5] and usually by 3–4 weeks. [6] By the time of presention , children have often developed antibodies to SARS-CoV-2, but test negative for the virus at RT-PCR . [6] The condition may match some or all of the diagnostic criteria for Kawasaki disease (i.e. the 'complete' or 'incomplete'/'atypical' subtypes [6] [41] ), [7] or for Kawasaki disease shock syndrome. [37] It tends to affect all paediatric age groups, ranging from infancy to adolescence. [5] [14] It can also share clinical features with other paediatric inflammatory conditions, including toxic shock syndrome, and secondary haemophagocytic lymphohistiocytosis or macrophage activation syndrome . [7] [26] Coinfections with other pathogens have been recorded. [3] Affected children always present with persistent fever. [6] Other clinical features at presentation vary. [8] In contrast to acute COVID-19, most children have gastrointestinal symptoms, such as diarrhoea , vomiting , and intense abdominal pain (sometimes severe enough to suggest appendicitis ). [6] Muscle pain and feelings of tiredness and general physical weakness are also very common. [6] [9] Some Kawasaki-like symptoms that may be present (especially in children under the age of 5) [43] include mucosal changes around the mouth (" strawberry tongue ", cracked lips , etc.), red eyes ( conjunctivitis without pus ), widespread rash (consistent with leukocytoclastic vasculitis [44] ), red or swollen hands and feet, and enlarged lymph nodes. [5] [8] [9] Chest or neck pain may also be present. [45] Severe headache and altered mental state have been reported, along with various neurological disturbances . [5] [16] [46] Features of meningitis have been reported. [8] [14] Some patients present with very low blood pressure and shock , and they may require urgent admission to a paediatric intensive care unit . [9] Cardiovascular involvement is very frequent. [6] [16] [43] Acute heart failure is common in the form of left ventricular dysfunction , [9] [47] and a left ventricular ejection fraction under 60% is frequent. [12] Shock is often of myocardial – mainly left ventricular – origin. [14] Respiratory symptoms are less common, [16] and are not usually a prominent feature. [14] [8] [47] When present, breathing difficulties are often linked to shock, [3] and are suggestive of heart failure. [8] Some children display features of a cytokine storm , [8] including extremely high serum interleukin-6 (IL-6) levels, [16] and need inotropic support to maintain cardiac output . [10] Coronary artery abnormalities, such as dilatation , are frequent. [9] Some children have developed coronary artery aneurysms. [8] Electrocardiographic (ECG) abnormalities are common. [9] Other cardiological features sometimes include inflammation of the heart valves ( valvulitis ) and of the fibrous sac surrounding the heart ( pericarditis ). [5] [47] Echocardiographic features of myocarditis (inflammation of the heart muscle) have been recorded. [5] [6] Affected children consistently show laboratory evidence of hyperinflammation. [9] Pronounced biological markers of inflammation generally include strongly raised erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), procalcitonin , ferritin , and IL6. [9] Low platelet counts and impaired blood clotting ( coagulopathy ) are also common, [14] with increased levels of D-dimer and fibrinogen . [9] Other haematological features include raised numbers of white blood cells ( leukocytosis ), characterized by high numbers of neutrophils , with many immature forms , and low numbers of lymphocytes ( lymphopaenia ). [9] Numbers of red blood cells and platelets may be either normal or decreased. [9] Acute kidney injury and low albumin levels in the blood ( hypoalbuminaemia ) are common. [26] Low blood sodium levels and raised liver enzymes have been reported. [14] Accumulations of fluid in the lungs ( pleural effusion ), around the heart ( pericardial effusion ), and in the abdomen ( ascites ) have also been reported, consistent with generalized inflammation. [26] Differences with respect to Kawasaki disease include frequent presentation with gastrointestinal symptoms such as vomiting, diarrhoea, and abdominal pain. [5] [6] Neurological involvement also appears to be relatively frequent. [8] It often affects older children, whereas Kawasaki disease usually occurs before the age of five. [6] [14] Multiorgan disease appears to be more frequent. [16] Myocarditis and cardiogenic shock shock seem to be relatively common. [16] Myocarditis may be more evident in older children and adolescents. [43] Preschool children tend to display more Kawasaki-like characteristics. [43] Features of macrophage activation syndrome appear to be more frequent than in Kawasaki disease. [17] [48] Characteristic laboratory findings that are not usually encountered in Kawasaki disease include very high levels of ventricular natriuretic peptide (a marker of heart failure), [10] as well as somewhat lower platelet counts, lower absolute lymphocyte counts, and higher CRP levels. [13] Very high troponin levels (suggestive of myocardial damage) are also common. [14] [26] [16] Clinical course [ edit ] Clinical course tends to be more severe than with Kawasaki disease. [42] A child's condition can deteriorate rapidly, even in the presence of reassuring laboratory findings. [15] Many children develop shock and heart failure. [6] Most require paediatric intensive care. [6] Supplemental oxygen is often needed, and mechanical ventilation is sometimes used. [6] Most children who receive expert multidisciplinary care survive. [6] In addition to respiratory distress , major complications that may need aggressive supportive care can include myocardial damage, acute kidney injury, and coagulopathy ( thrombophilia ). [12] In some cases, sustained cardiac arrhythmias have led to haemodynamic collapse and need for extracorporeal membrane oxygenation (ECMO). [9] Deaths have been recorded in a small minority (under 2%) of the cases reported. [6] [49] Occasionally, fatalities have followed complications of ECMO. [10] Some children exposed to COVID-19 also appear to have a less severe Kawasaki-like disease. [32] Ventricular function often recovers before discharge from hospital (often after 6–10 days). [6] Coronary artery aneurysms can develop even in the absence of Kawasaki-like features. [5] Their frequency and severity is uncertain. [13] So far, they have been recorded in 7% of reported cases. [6] Long-term prognosis is unclear. [9] Diagnosis [ edit ] Preliminary WHO case definition [18] Children and adolescents 0–19 years of age with fever >3 days AND Two of the following: Rash or bilateral non- purulent conjunctivitis or muco-cutaneous inflammation signs (oral, hands or feet) Hypotension or shock Features of myocardial dysfunction, pericarditis, valvulitis, or coronary abnormalities (including ECHO findings or elevated Troponin/ NT-proBNP ) Evidence of coagulopathy (by PT , PTT , elevated d-Dimers) Acute gastrointestinal problems (diarrhoea, vomiting, or abdominal pain) AND Elevated markers of inflammation such as ESR, C-reactive protein, or procalcitonin AND No other obvious microbial cause of inflammation, including bacterial sepsis, staphylococcal or streptococcal shock syndromes AND Evidence of COVID-19 ( RT-PCR , antigen test or serology positive), or likely contact with patients with COVID-19 ( Note: Consider this syndrome in children with features of typical or atypical Kawasaki disease or toxic shock syndrome.) ... In the United States, more than 200 cases were suspected by mid-May, [110] including some 145 in New York; [111] [112] 186 confirmed cases were eventually diagnosed between 15 March and 20 May in 26 US states . [113] [114] As of 11 May 2020, five fatalities were reported (1 in France, 1 in the UK, 3 in the US). [3] In peer-reviewed medical journals, case series and related studies of the new condition were rapidly reported from countries including the UK; [115] [116] Italy; [69] Spain; [117] [118] [119] France and Switzerland; [120] France; [4] [121] [122] and across the US, [113] [123] including New York. [67] [124] [125] The emerging observations suggested somewhat greater variety in the severity of symptoms than was originally thought. [17] The proposal of a new clinical entity during a pandemic also prompted scientific discussion about its possible distinction from Kawasaki disease, and the potential role of COVID-19. [32] [52] [59] [65] [66] [73] [94] [96] By 15 July, 342 confirmed MIS-C cases (including 6 deaths) had been recorded in the US across 36 states plus Washington DC . [72] [126] Most (71%) of the children were Hispanic/Latino or non-Hispanic Black people, and the CDC underlined the need to learn the reasons for such a preponderance. [72] [127] By 29 July, a total of 570 cases and 10 deaths had been reported across 40 states, Washington DC, and New York City. [49] Until late May, no confirmed case had been documented outside the EU/EEA/UK and USA. [3] No suspicious case had been observed in East Asia or Southeast Asia (or in Australia or New Zealand ). [73] [128] [129] The absence of documented cases in China and other Asian countries that had already experienced a COVID-19 epidemic led to conjectures regarding the possibility of a significant evolution of the virus, or variations in susceptibility in different populations. [26] On 2 June, news emerged of a first case of MIS-C diagnosed in Peru . [130] [131] In Brazil , cases of MIS-C have been reported in São Paulo , [132] and in the context of a prospective study in Pará ; [133] more children with severe late manifestations of COVID-19 were being admitted to paediatric intensive care units in the region. [133] In Chile , 42 confirmed cases of MIS-C had been recorded nationally by June 28, including 27 in the capital, Santiago. [134] In Russia , 13 children had been treated (5 with intensive care) by mid-June for a multisystem inflammatory syndrome at the Morozov Children's Hospital in Moscow , including a 2-year-old girl with the COVID-19 infection who died on 23 May following an initial diagnosis of suspected Kawasaki disease. [78] In Iran , a case report (first submitted in May) described severe MIS-C in a 5-year-old girl who had presented with shock and was initially diagnosed with Kawasaki disease, [85] and further cases of the new syndrome have been recorded. [86] In India , a case of suspected MIS-C was reported in late May regarding a child who had presented in a COVID-19 hotspot in Kerala . [80] An editorial commentary urged clinicians to have a high level of diagnostic suspicion and follow WHO and CDC definitions to facilitate timely identification and treatment of cases. [135] During July, suspected cases were being flagged and reported in Mumbai , [136] in Delhi , [137] Chennai , [79] and elsewhere. [138] In Pakistan , [139] at least 24 children were said to have Kawasaki-like symptoms in Lahore , [140] where 8 cases fulfilling WHO criteria were prospectively identified by 30 June. [81] In Kazakhstan , 14 cases were confirmed by 20 August (among 2,357 children known to have been infected). [82] Cases have been recorded in Israel , [88] including one of a child who presented with severe central nervous system involvement and complement deficiency . [89] In Turkey , four children with a Kawasaki-like disease probably associated with COVID-19 are reported to have been admitted to the children's hospital of Hacettepe University in Ankara between 13 April and 11 July. [84] In Algeria , a first case was recorded in June. [90] In Egypt , on 10 July the authorities denied rumours of the existence of cases of Kawasaki-like disease in the country. [141] In South Africa , the first 23 affected children were treated in Cape Town – the initial epicentre of the national COVID-19 epidemic – between 4 June and 24 July. [91] In Ecuador , the Ministry of Health announced on 19 July the presence of 46 probable cases. [142] In Costa Rica , a national public health organization announced towards the end of August that three children had been diagnosed with MIS-C. [143] Cases of MIS-C had also been recorded in many other Latin American countries, including Argentina , Bolivia , Colombia , Cuba , the Dominican Republic , El Salvador , Guatemala , Honduras , Mexico , Nicaragua , Panama , Uruguay , and Venezuela , as well as in Puerto Rico . [22] News of a first confirmed case of PIMS-TS in Australia emerged (from Victoria ) on 4 September, along with news of other suspected cases under review. [144] In South Korea , news of two confirmed cases broke on 5 October [83] (and the existence of a case dating back to the end of April was reported in November [75] ).
-
Dupuytren's Contracture
Wikipedia
He described the condition and the operation in The Lancet in 1834 [27] after presenting it in 1833, and posthumously in 1836 in a French publication by Hôtel-Dieu de Paris . [28] The procedure he described was a minimally invasive needle procedure. ... Postgraduate Medical Journal . 81 (957): 425–28. doi : 10.1136/pgmj.2004.027425 . ... Archived from the original on 2017-06-28. ^ "Progression of Dupuytren's disease" . ... The Journal of Hand Surgery: Journal of the British Society for Surgery of the Hand . 28 (5): 427–31. doi : 10.1016/S0266-7681(03)00013-5 . ... The Bone & Joint Journal . 31B (3): 443. ^ Therapies for Dupuytren's contracture and Ledderhose disease with possibly less benefit , International Dupuytren Society, 19 January 2011 Archived 14 March 2011 at the Wayback Machine . ^ Cold Laser Treatment Archived 2013-11-09 at the Wayback Machine at International Dupuytren Society online forum. Accessed: 28 August 2012. ^ Jerosch-Herold, Christina; Shepstone, Lee; Chojnowski, Adrian J.; Larson, Debbie (2008).
-
Gout
Wikipedia
., beans , peas , lentils , and spinach ) is not associated with gout. [25] Neither is total dietary protein . [24] [25] Alcohol consumption is strongly associated with increased risk, with wine presenting somewhat less of a risk than beer or spirits . [25] [26] Eating skim milk powder enriched with glycomacropeptide (GMP) and G600 milk fat extract may reduce pain but may result in diarrhea and nausea. [27] Physical fitness, healthy weight, low-fat dairy products, and to a lesser extent, coffee and taking vitamin C, appear to decrease the risk of gout; [28] [29] [30] [31] however, taking vitamin C supplements does not appear to have a significant effect in people who already have established gout. [4] Peanuts, brown bread, and fruit also appear protective. [22] This is believed to be partly due to their effect in reducing insulin resistance . [30] Genetics [ edit ] Gout is partly genetic, contributing to about 60% of variability in uric acid level. [8] The SLC2A9 , SLC22A12 , and ABCG2 genes have been found to be commonly associated with gout and variations in them can approximately double the risk. [32] [33] Loss-of-function mutations in SLC2A9 and SLC22A12 causes low blood uric acid levels by reducing urate absorption and unopposed urate secretion. [33] The rare genetic disorders familial juvenile hyperuricemic nephropathy , medullary cystic kidney disease , phosphoribosylpyrophosphate synthetase superactivity and hypoxanthine-guanine phosphoribosyltransferase deficiency as seen in Lesch–Nyhan syndrome , are complicated by gout. [8] Medical conditions [ edit ] Gout frequently occurs in combination with other medical problems . ... PMID 27380294 . ^ a b c d e f g h i j k l m n o p q r s t u v w x y z aa ab ac ad ae af ag ah Richette P, Bardin T (January 2010). "Gout". Lancet . 375 (9711): 318–28. doi : 10.1016/S0140-6736(09)60883-7 . ... PMID 27166465 . ^ "Febuxostat for the management of hyperuricaemia in people with gout Guidance and guidelines" . www.nice.org.uk . 17 December 2008. Archived from the original on 28 March 2017 . Retrieved 28 March 2017 . ^ "Drug Safety and Availability – FDA adds Boxed Warning for increased risk of death with gout medicine Uloric (febuxostat)" . ... PMID 20238366 . ^ "Krystexxa" . www.ema.europa.eu . Archived from the original on 28 March 2017 . Retrieved 28 March 2017 . ^ "Pegloticase: withdrawal of its EU marketing authorisation is welcome".ABCG2, SLC2A9, CD14, IL1B, IL1RN, ALPK1, XDH, CARD8, ALDH16A1, HPRT1, ZNF518B, HNF1B, DARS2, BCAS3, ALX4, RNF115, MACROD1, SEC61A1, NRBP1, A1CF, MLXIPL, TRIM54, MEPE, PRKAG2, SFMBT1, CNTN5, SLC22A11, CARMIL1, RBFOX1, SHLD2, ABCA1, TBL2, FNDC4, SLC17A4, ABCC9, SLC17A2, H2AC5P, BAIAP2, TRIM38, KAT5, SCGN, POLR3C, SLC17A3, SLC22A7, CD160, NXPH4, GPN1, R3HDM2, MLXIP, SLC4A1AP, FSTL4, CUX2, IFT172, FBXO22, ZSCAN31, WNT5B, SLC13A3, TRIM46, LINC02537, RAF1P1, LHFPL3, KRT8P26, OR7E35P, CRIP3, FAM86MP, LINC01460, LINC01405, ALG1L3P, ADPGK-AS1, H2BC2P, MUC22, AADACL2-AS1, CT69, LINC01229, RFX3-AS1, B4GALT1-AS1, PPM1K-DT, RELA-DT, NRXN2-AS1, HNF1A-AS1, NALCN, H2BC1, CLNK, WDR1, INHBE, QRICH2, RNASEH2C, C2orf16, ZNF512, AP5B1, UBE2Q2, SLC22A12, ZNF513, CNIH2, NRG4, NIPAL1, FAM53A, LINC01010, NUDT17, KRTCAP3, SLC16A9, H2AC1, JAZF1, SH2B3, ABCG1, SNX17, ORC4, IGF1R, INHBC, INSR, KCNQ1, LRP6, MAP3K11, MPV17, MUC1, SLC22A18AS, HLF, OVOL1, PDE1C, PDZK1, PFKM, PKD2, ACVR2A, PPM1G, PRKCA, HNF4G, HGF, PRPS1, CYP2E1, ALDH2, ANK1, APOE, ATP1A4, BDKRB2, CFTR, CLCNKB, CYP2C8, EPB42, HFE, FGFR2, FRK, G6PC, SLC37A4, GCKR, GTF3C2, H1-2, H1-6, MAPK6, PPARD, H2BP5, ZMYM6, SPP1, SPTA1, SPTB, ABCC8, SLC5A6, ALDH1A2, PTPRD, HNF1A, TPST1, H4C2, H4C3, H3C2, H2BC4, UMOD, VDR, H2AC4, BAZ1B, BCL7B, NRXN2, PYGM, BABAM2, MAP4K2, RAB27B, RARB, MRPL33, RREB1, ATXN2, SLC22A1, SLC4A1, SLC12A3, SLC17A1, H2AC6, CXCL8, ADIPOQ, CRP, BCL2, CXCL16, NR2C2, MT1B, PRKG2, POMC, S100A9, CCL2, IL33, MTTP, SLC40A1, SIRT1, MAP3K7, IL18, IL6, TGFB1, TNF, HLA-B, IL4
-
Avian Influenza
Wikipedia
Highly pathogenic strains spread quickly among flocks and can destroy a flock within 28 hours; the less pathogenic strains may affect egg production but are much less deadly. [ citation needed ] Although it is possible for humans to contract the avian influenza virus from birds, human-to-human contact is much more difficult without prolonged contact. ... After culling all of the poultry in the area, no more cases were diagnosed. [23] In 2006, the first human-to-human transmission likely occurred when 7 members of a family in Sumatra became infected after contact with a family member who had worked with infected poultry. [27] Although millions of birds have become infected with the virus since its discovery, 359 people have died from H5N1 in twelve countries according to World Health Organization reports as of August 10, 2012. [28] The H5N1 outbreak in Thailand caused massive economic losses, especially among poultry workers. ... Archived (PDF) from the original on 2019-06-27 . Retrieved 2020-03-28 . Avian influenza strains are those well adapted to birds ^ Chapter Two : Avian Influenza by Timm C. ... Archived from the original on 2006-09-14 . Retrieved 2020-03-28 . full text of online book ^ [1] CDC has a phylogenetic tree showing the relationship between dozens of highly pathogenic varieties of the Z genotype of avian flu virus H5N1 and ancestral strains. ^ Hiromoto, Y.; Yamazaki, Y.; Fukushima, T.; Saito, T.; Lindstrom, S. ... "History of high pathogenic avian influenza" . Rev. Sci. Tech . 28 (1): 19–38. doi : 10.20506/rst.28.1.1856 .
-
Antineoplastic Resistance
Wikipedia
The tolerance of DNA damage can grant cancer cells a method of resistance to those drugs which normally induce apoptosis through DNA damage. [2] [12] Other genes involved in the apoptotic pathway related drug resistance include h-ras and bcl-2 /bax. [25] Oncogenic h-ras has been found to increase expression of ERCC1, resulting in enhanced DNA repair (see above). [26] Inhibition of h-ras was found to increase cisplatin sensitivity in glioblastoma cells. [27] Upregulated expression of Bcl-2 in leukemic cells ( non-Hodgkin’s lymphoma ) resulted in decreased levels of apoptosis in response to chemotherapeutic agents, as Bcl-2 is a pro-survival oncogene . [28] Altered target molecules [ edit ] During targeted therapy , oftentimes the target has modified itself and decreased its expression to the point that therapy is no longer effective. ... PMID 9109439 . ^ Hoffmeyer, S.; Burk, O.; von Richter, O.; Arnold; et al. (2000-03-28). "Functional polymorphisms of the human multidrug-resistance gene: Multiple sequence variations and correlation of one allele with P-glycoprotein expression and activity in vivo" .
-
Agoraphobia
Wikipedia
One such approach links the development of agoraphobia with modernity . [28] Factors considered contributing to agoraphobia within modernity are the ubiquity of cars and urbanization. ... Retrieved 2009-08-07 . ^ Julia Moskin (February 28, 2007). "From Phobia To Fame: A Southern Cook's Memoir" .
-
Dental Fluorosis
Wikipedia
The treatment options are: Mild cases: Tooth bleaching [14] Moderate cases: Enamel microabrasion (outer affected layer of enamel is abraded in an acidic environment) [14] Severe cases: Composite fillings , Micro-abrasion, Veneers , Crowns [14] Epidemiology [ edit ] Fluorosis is extremely common, with 41% of adolescents having definite fluorosis, and another 20% "questionably" having fluorosis according to the Centers for Disease Control. [27] As of 2005 [update] surveys conducted by the National Institute of Dental and Craniofacial Research in the USA between 1986 and 1987 [28] and by the Center of Disease Control between 1999 and 2004 [27] are the only national sources of data concerning the prevalence of dental fluorosis. ... Dietary reference intakes for fluoride [28] : 25 Age group Reference weight kg (lb) Adequate intake (mg/day) Tolerable upper intake (mg/day) Infants 0–6 months 7 (16) 0.01 0.7 Infants 7–12 months 9 (20) 0.5 0.9 Children 1–3 years 13 (29) 0.7 1.3 Children 4–8 years 22 (48) 1.0 2.2 Children 9–13 years 40 (88) 2.0 10 Boys 14–18 years 64 (142) 3.0 10 Girls 14–18 years 57 (125) 3.0 10 Males 19 years and over 76 (166) 4.0 10 Females 19 years and over 61 (133) 3.0 10 If the water supply is fluoridated at the level of 1 ppm, one must consume one litre of water in order to take in 1 mg of fluoride.FIS1, DNM1L, MFN1, ESR1, COL1A2, MMP20, MMP2, BGLAP, VDR, TP53, PRL, CALCR, TGFB1, MPO, AQP5, MMP9, GSTP1, COMT, TUFT1, COL14A1, SIRT1, TNFSF11, ACAN, TFIP11, HPGDS, OSTM1, TIMP1, ODAM, MIER1, MMP25, SLCO6A1, ATP6V0D2, FAM83H, GSTK1, MIR155, MIR200C, TIMP2, PTH, TGFBR2, SOD2, BCL2, RUNX2, CDKN2A, CLCN7, CLU, DCX, DLX1, DLX2, ESR2, ESRRB, FRZB, GPR18, SMAD3, MGMT, MLH1, MMP13, NFATC1, MAPK8, ALOX15, ROS1, SOD1, H3P10
-
Compulsive Buying Disorder
Wikipedia
Scientists reported compulsive buyers have significant changeable activity in this area of the brain. [14] Compulsive buying seems to represent a search for self in people whose identity is neither firmly felt nor dependable, as indicated by the way purchases often provide social or personal identity-markers. [26] Those with associated disorders such as anxiety, depression and poor impulse control are particularly likely to be attempting to treat symptoms of low self-esteem through compulsive shopping. [27] Others, however, object that such psychological explanations for compulsive buying do not apply to all people with CBD. [28] Social conditions also play an important role in CBD, the rise of consumer culture contributing to the view of compulsive buying as a specifically postmodern addiction, particularly with regard to internet buying platforms. [29] Readily available credit cards enable casual spending beyond one's means, and some would suggest that the compulsive buyer should lock up or destroy credit cards altogether. [30] Online shopping also facilitates CBD, with online auction addiction, used to escape feelings of depression or guilt, becoming a recognizable problem. [31] What differentiates CBD from healthy shopping is the compulsive, destructive and chronic nature of the buying. ... Oxford; New York: Oxford University Press. p. 28 . ISBN 978-0-19-530699-6 . OCLC 153773333 . ^ Abramowitz, Jonathan S.; Houts, Arthur C. (2006).
-
Viral Disease
Wikipedia
Groups: I - dsDNA II - ssDNA III - dsRNA IV - positive-sense ssRNA V - negative-sense ssRNA VI - ssRNA-RT VII - dsDNA-RT Clinically important virus families and species with characteristics Family Baltimore group Important species Envelopment Adenoviridae I [3] [4] Adenovirus [3] [4] N [3] [4] Herpesviridae I [3] [4] Herpes simplex, type 1 , Herpes simplex, type 2 , Varicella-zoster virus , Epstein–Barr virus , Human cytomegalovirus , Human herpesvirus, type 8 [5] [6] [7] Y [3] [4] Papillomaviridae I [3] [8] Human papillomavirus [3] [8] N [3] [8] Polyomaviridae I [3] [9] BK virus , JC virus [3] [9] N [3] [9] Poxviridae I [3] [4] Smallpox [3] [4] Y [3] [4] Parvoviridae II [3] [4] Parvovirus B19 [3] [4] N [3] [4] Reoviridae III [10] Rotavirus , [10] Orbivirus , Coltivirus , Banna virus N [4] Astroviridae IV [11] Human astrovirus [4] N [4] Caliciviridae IV [10] Norwalk virus [4] N [4] Coronaviridae IV [12] Human coronavirus 229E , Human coronavirus NL63 , Human coronavirus OC43 , Human coronavirus HKU1 , Middle East respiratory syndrome-related coronavirus , Severe acute respiratory syndrome coronavirus , [4] Severe acute respiratory syndrome coronavirus 2 Y [4] Flaviviridae IV [3] [4] [13] Hepatitis C virus , [3] yellow fever virus , [3] dengue virus , [3] West Nile virus , [3] TBE virus , [4] Zika virus Y [3] [4] Hepeviridae IV [14] Hepatitis E virus [4] N [4] [14] Matonaviridae IV [3] [4] [15] Rubella virus [3] [16] Y [3] [4] Picornaviridae IV [17] coxsackievirus , hepatitis A virus , poliovirus , [4] rhinovirus N [4] Arenaviridae V [18] Lassa virus [4] [18] Y [4] [18] Bunyaviridae V [19] Crimean-Congo hemorrhagic fever virus , Hantaan virus [4] Y [4] [19] Filoviridae V [20] Ebola virus , [20] Marburg virus [20] Y [4] Orthomyxoviridae V [3] [21] Influenza virus [3] [21] Y [3] [21] Paramyxoviridae V [22] Measles virus , [3] Mumps virus , [3] Parainfluenza virus [3] [4] Y [3] [22] Pneumoviridae V [23] Respiratory syncytial virus [3] Y [3] Rhabdoviridae V [24] Rabies virus [3] [4] Y [3] [4] Unassigned [25] V [25] Hepatitis D [25] Y [25] Retroviridae VI [3] [26] HIV [3] [4] Y [3] [4] Hepadnaviridae VII [3] Hepatitis B virus [3] [4] Y [3] [4] Clinical characteristics [ edit ] The clinical characteristics of viruses may differ substantially among species within the same family: Type Family Transmission Diseases Treatment Prevention Adenovirus Adenoviridae droplet contact [3] fecal-oral [3] venereal [3] direct eye contact [3] gastroenteritis [3] keratoconjunctivitis [3] pharyngitis [3] pharyngoconjunctival fever [3] None [3] Adenovirus vaccine hand washing covering mouth when coughing or sneezing avoiding close contact with the sick Coxsackievirus Picornaviridae fecal-oral [3] [27] respiratory [27] droplet contact [3] Hand, foot and mouth disease [28] pleurodynia [27] aseptic meningitis [27] pericarditis myocarditis None [3] hand washing covering mouth when coughing/sneezing avoiding contaminated food/water improved sanitation Cytomegalovirus Herpesviridae vertical transmission [3] [29] [30] bodily fluids [3] infectious mononucleosis [3] Cytomegalic inclusion disease [3] Premature birth [30] liver , lung and spleen diseases in the newborn [30] Small size at birth [30] Small head size [30] congenital seizures in the newborn [30] ganciclovir [3] cidofovir [3] foscarnet [3] hand washing avoid sharing food and drinks with others safe sex Epstein–Barr virus Herpesviridae saliva [3] infectious mononucleosis [3] Burkitt's lymphoma [3] Hodgkin's lymphoma nasopharyngeal carcinoma None [3] avoiding close contact with the sick Hepatitis A virus Picornaviridae fecal-oral [3] [31] acute hepatitis [3] [31] Immunoglobulin ( post-exposure prophylaxis ) [3] Hepatitis A vaccine [3] [31] avoiding contaminated food/water [3] improved sanitation Hepatitis B virus Hepadnaviridae bodily fluids [3] Vertical and sexual [32] acute hepatitis [3] [32] chronic hepatitis [32] hepatic cirrhosis [32] hepatocellular carcinoma [32] Lamivudine [3] [32] immunoglobulin [3] Adefovir [3] Entecavir [3] Pegylated interferon alfa-2 [3] Hepatitis B vaccine [3] [32] immunoglobulin (perinatal and post-exposure prophylaxis) [3] avoiding shared needles/syringes safe sex Hepatitis C virus Flaviviridae blood [3] sexual contact [3] acute hepatitis [3] [33] chronic hepatitis [3] hepatic cirrhosis [3] hepatocellular carcinoma [3] Ribavirin [3] [33] Pegylated interferon alfa-2 [3] avoiding shared needles/syringes safe sex Herpes simplex virus, type 1 Herpesviridae direct contact [3] [29] saliva [3] [29] herpes labialis , [3] cold sores [3] [29] – can recur by latency [3] gingivostomatitis in children [3] tonsillitis & pharyngitis in adults [3] keratoconjunctivitis [3] acyclovir [3] [29] famciclovir [3] [29] foscarnet [3] penciclovir [3] avoiding close contact with lesions safe sex Herpes simplex virus, type 2 Herpesviridae sexual contact [3] [29] vertical transmission [3] [29] Skin vesicles, mucosal ulcers, [29] Oral and/or genital [29] Can be latent [3] Aseptic meningitis [3] acyclovir [3] [29] famciclovir [3] [29] foscarnet [3] penciclovir [3] cidofovir [3] avoiding close contact with lesions [3] safe sex [3] HIV Retroviridae sexual contact [3] [34] blood [3] [34] breast milk [3] [34] vertical transmission AIDS [3] HAART , [3] such as protease inhibitors [34] and reverse-transcriptase inhibitors [34] zidovudine (perinatally) [3] blood product screening [3] safe sex [3] avoiding shared needles/syringes Human coronavirus 229E (HCoV-229E) Coronaviridae droplet contact fomites common cold pneumonia bronchiolitis Human coronavirus NL63 (HCoV-NL63) Coronaviridae droplet contact common cold rhinitis bronchitis bronchiolitis pneumonia croup Human coronavirus OC43 (HCoV-OC43) Coronaviridae common cold pneumonia Human coronavirus HKU1 (HCoV-HKU1) Coronaviridae common cold pneumonia bronchiolitis Human herpesvirus, type 8 Herpesviridae Saliva [29] Sexual [29] Kaposi sarcoma [3] multicentric Castleman disease [3] primary effusion lymphoma [3] many in evaluation-stage [3] avoid close contact with lesions safe sex Human papillomavirus Papillomaviridae direct contact [3] [35] sexual contact [35] vertical transmission ( common , flat , plantar and anogenital warts , laryngeal papillomas , epidermodysplasia verruciformis ) [3] Malignancies for some species ( cervical carcinoma , [35] squamous cell carcinomas ) [3] liquid nitrogen [3] laser vaporization [3] cytotoxic chemicals [3] interferon [3] cidofovir [3] HPV vaccine [3] [35] avoiding close contact with lesions [3] safe sex [3] Influenza virus Orthomyxoviridae droplet contact [3] influenza [3] ( Reye syndrome ) [3] amantadine [3] [21] rimantadine [3] [21] zanamivir [3] [21] oseltamivir [3] [21] influenza vaccine [3] [21] amantadine [3] rimantadine [3] hand washing covering mouth when coughing/sneezing avoiding close contact with the sick Measles virus Paramyxoviridae droplet contact [3] [22] measles [3] [22] postinfectious encephalomyelitis [3] None [3] MMR vaccine [3] [22] quarantining the sick avoiding contact with the sick Middle East respiratory syndrome-related coronavirus (MERS-CoV) Coronaviridae close human contact Middle East respiratory syndrome (MERS) Mumps virus Paramyxoviridae droplet contact [3] [22] mumps [3] [22] None [3] MMR vaccine [3] [22] avoiding close contact with the sick Parainfluenza virus Paramyxoviridae droplet contact [3] [22] croup [3] pneumonia [3] bronchiolitis [3] common cold [3] None [3] hand washing covering mouth when coughing/sneezing Poliovirus Picornaviridae fecal-oral [3] poliomyelitis [3] None [3] Polio vaccine [3] [31] avoiding contaminated food and water improved sanitation Rabies virus Rhabdoviridae animal bite [3] [24] droplet contact [3] rabies [3] (fatal encephalitis) [24] Post-exposure prophylaxis [3] rabies vaccine [24] avoiding rabid animals Respiratory syncytial virus Pneumoviridae droplet contact [3] [22] hand to mouth [3] bronchiolitis [3] pneumonia [3] influenza-like syndrome [3] severe bronchiolitis with pneumonia [3] ( ribavirin ) [3] hand washing [3] avoiding close contact with the sick [3] palivizumab in high risk individuals [3] covering mouth when coughing/sneezing Rubella virus Togaviridae Respiratory [36] droplet contact [3] congenital rubella [3] [36] German measles [3] None [3] MMR vaccine [3] [36] avoiding close contact with the sick Severe acute respiratory syndrome coronavirus (SARS-CoV) Coronaviridae droplet contact severe acute respiratory syndrome (SARS) Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) Coronaviridae droplet contact coronavirus disease 2019 (COVID-19) hand washing covering mouth when coughing or sneezing social distancing Varicella-zoster virus Herpesviridae droplet contact [3] direct contact chickenpox [29] herpes zoster [3] Congenital varicella syndrome [29] Varicella : acyclovir [3] famciclovir [3] valacyclovir [3] Zoster : acyclovir [3] famciclovir [3] Varicella : varicella vaccine [3] varicella-zoster immunoglobulin [3] avoiding close contact with the sick Zoster : vaccine varicella-zoster immunoglobulin See also [ edit ] List of latent human viral infections Pathogenic bacteria References [ edit ] ^ Taylor, M.P.; Kobiler, O.; Enquist, L. ... International Committee on Taxonomy of Viruses (ICTV) . Retrieved 2020-05-28 . ^ Tuthill, Tobias J.; Groppelli, Elisabetta; Hogle, James M.; Rowlands, David J. (2010).
-
Diabetic Neuropathy
Wikipedia
It is estimated that neuropathy affects 25% of people with diabetes. [28] Diabetic neuropathy is implicated in 50–75% of nontraumatic amputations . ... "Treatment of painful diabetic neuropathy" . Ther Adv Chronic Dis . 6 (1): 15–28. doi : 10.1177/2040622314552071 .INSR, TLR4, CASP3, TGFB1, CAT, NTF3, HGF, GRM5, MME, CHRM2, MMP2, SGK1, AKR1B1, MMP9, LEPR, NGF, BDNF, IL1B, TNF, IGF1, NGFR, MPZ, TRPA1, NTRK1, BECN1, HHIP, PTGS2, MAPK14, SREBF1, BAD, TGFB2, BDKRB1, LRRK2, TGFB3, NRG1, MBP, CNR1, VEGFA, NFE2L2, GABPA, APOE, MTHFR, TNFSF11, PARP1, GSTT1, NPY, GSTM1, SIRT1, EPO, ST3GAL4, TRPV1, VDR, UCP3, TXN, TTR, TLR5, TKT, THBD, UCP2, HSPB3, SCG2, LOH19CR1, MIR25, MIR199A2, MIR199A1, MIR155, COL6A5, RPAIN, TMX1, FTO, SEMA6A, KIDINS220, STAP2, DUOX1, GAL, NOX4, DUOX2, ARIH1, DIANPH, NFASC, PNPLA6, PPARGC1A, TXNIP, DCAF1, SMPD1, NRP1, RIPK1, RNMT, IRS2, SOD2, PDE4A, SLC6A6, HMOX1, GRB2, GPX1, GLO1, GAP43, MTOR, FOXO3, ACSL1, EPOR, ENO2, DPYSL2, DECR1, ACE, CYBB, CSF3, COL11A2, CCR8, CAV1, C3, HCN2, ATP1A1, XIAP, ALOX15, ALB, GSTP1, AGFG1, SHH, HSPB1, CCL1, RPS19, ROS1, RELA, PTPN1, PSMD9, MAPK3, PRKCD, PMM2, PLAT, SERPINE2, PGF, AGER, TNFRSF11B, NOTCH1, MIF, MFAP4, LPO, IL10, IL6, IGFBP5, IGF1R, HSPB2, MIR499A
-
Aspiration Pneumonia
Wikipedia
Aspiration pneumonia most often develops due to micro-aspiration of saliva, or bacteria carried on food and liquids, in combination with impaired host immune function. [28] Chronic inflammation of the lungs is a key feature in aspiration pneumonia in elderly nursing home residents and presents as a sporadic fever (one day per week for several months). ... Choking [ edit ] After falls, choking on food presents as the second highest cause of preventable death in aged care. [28] Although food choking risk is commonly associated with young children, data shows that individuals over 65 years of age have a choking incidence that is seven times higher than children aged 1–4 years.
-
Medical Abortion
Wikipedia
Food and Drug Administration (FDA). [21] This model has been shown to be safe, effective, efficient, and satisfactory. [22] [23] [16] Complete abortion can be confirmed via telephone-based assessment. [24] Contraindications [ edit ] Contraindications to mifepristone are inherited porphyria , chronic adrenal failure , and ectopic pregnancy. [25] [26] Some consider an intrauterine device in place to be a contraindication as well. [26] A previous allergic reaction to mifepristone or misoprostol is also a contraindication. [25] Many studies excluded women with severe medical problems such as heart and liver disease or severe anemia. [26] Caution is required in a range of circumstances including: [25] long-term corticosteroid use; bleeding disorder; severe anemia In some cases, it may be appropriate to refer people with preexisting medical conditions to a hospital-based abortion provider. [27] Adverse effects [ edit ] Symptoms that require immediate medical attention: [28] Heavy bleeding (enough blood to soak through four sanitary pads in 2 hours) Abdominal pain, nausea, vomiting, diarrhea, fever for more than 24 hours after taking mifepristone Fever of 38 °C (100.4 °F) or higher for more than 4 hours Most women will have cramping and bleeding heavier than a menstrual period. [26] Nausea, vomiting, diarrhea, headache, dizziness, and fever/chills are also common. ... "Interruption of nonviable pregnancies of 24–28 weeks' gestation using medical methods" .
-
Hypoactive Sexual Desire Disorder
Wikipedia
It was within this context that the diagnosis of ISD was created. [27] In the revision of the DSM-III, published in 1987 (DSM-III-R), ISD was subdivided into two categories: Hypoactive Sexual Desire Disorder and Sexual Aversion Disorder (SAD). [28] The former is a lack of interest in sex and the latter is a phobic aversion to sex. ... "Beyond dysfunction: a new view of women's sexual problems". J Sex Marital Ther . 28 (Suppl 1): 225–32. doi : 10.1080/00926230252851357 .
-
Spanish Flu
Wikipedia
In Senegal it was named 'the Brazilian flu', and in Brazil 'the German flu', while in Poland it was known as 'the Bolshevik disease'. [20] In Spain itself, the nickname for the flu, the "Naples Soldier", was adopted from a 1916 operetta, The Song of Forgetting ( La canción del olvido ) after one of the librettists quipped that the play's most popular musical number, Naples Soldier , was as catchy as the flu. [21] Today, however, 'Spanish flu' (Gripe Española) is the most widely used name for the pandemic in Spain. [22] Other terms for this virus include the "1918 influenza pandemic," the "1918 flu pandemic", or variations of these. [23] [24] [25] History Timeline First wave of early 1918 The pandemic is conventionally marked as having begun on 4 March 1918 with the recording of the case of Albert Gitchell, an army cook at Camp Funston in Kansas , United States, despite there likely having been cases before him. [26] The disease had been observed in Haskell County in January 1918, prompting local doctor Loring Miner to warn the US Public Health Service 's academic journal. [27] Within days, 522 men at the camp had reported sick. [28] By 11 March 1918, the virus had reached Queens , New York. [29] Failure to take preventive measures in March/April was later criticized. [30] As the US had entered World War I , the disease quickly spread from Camp Funston, a major training ground for troops of the American Expeditionary Forces , to other US Army camps and Europe, becoming an epidemic in the Midwest , East Coast , and French ports by April 1918, and reaching the Western Front by the middle of the month. [26] It then quickly spread to the rest of France, Great Britain, Italy, and Spain and in May reached Breslau and Odessa . [26] After the signing of the Treaty of Brest-Litovsk (March 1918), Germany started releasing Russian prisoners of war, who then brought the disease to their country. [31] It reached North Africa, India, and Japan in May, and soon after had likely gone around the world as there had been recorded cases in Southeast Asia in April. [32] In June an outbreak was reported in China. [33] After reaching Australia in July, the wave started to recede. [32] The first wave of the flu lasted from the first quarter of 1918 and was relatively mild. [34] Mortality rates were not appreciably above normal; [35] in the United States ~75,000 flu-related deaths were reported in the first six months of 1918, compared to ~63,000 deaths during the same time period in 1915. [36] In Madrid, Spain, fewer than 1,000 people died from influenza between May and June 1918. [37] There were no reported quarantines during the first quarter of 1918. However, the first wave caused a significant disruption in the military operations of World War I , with three-quarters of French troops, half the British forces, and over 900,000 German soldiers sick. [38] Seattle police wearing masks in December 1918 Deadly second wave of late 1918 The second wave began in the second half of August, probably spreading to Boston and Freetown , Sierra Leone , by ships from Brest , where it had likely arrived with American troops or French recruits for naval training. [38] From the Boston Navy Yard and Camp Devens (later renamed Fort Devens ), about 30 miles west of Boston, other U.S. military sites were soon afflicted, as were troops being transported to Europe. [39] Helped by troop movements, it spread over the next two months to all of North America, and then to Central and South America, also reaching Brazil and the Caribbean on ships. [40] In July 1918, the Ottoman Empire saw its first cases in some soldiers. [41] From Freetown, the pandemic continued to spread through West Africa along the coast, rivers, and the colonial railways, and from railheads to more remote communities, while South Africa received it in September on ships bringing back members of the South African Native Labour Corps returning from France. [40] From there it spread around southern Africa and beyond the Zambezi , reaching Ethiopia in November. [42] On September 15, New York City saw its first fatality from influenza. [43] The Philadelphia Liberty Loans Parade , held in Philadelphia , Pennsylvania , on 28 September 1918 to promote government bonds for World War I, resulted in 12,000 deaths after a major outbreak of the illness spread among people who had attended the parade. [44] From Europe, the second wave swept through Russia in a southwest–northeast diagonal front, as well as being brought to Arkhangelsk by the North Russia intervention , and then spread throughout Asia following the Russian Civil War and the Trans-Siberian railway , reaching Iran (where it spread through the holy city of Mashhad ), and then later India in September, as well as China and Japan in October. [45] The celebrations of the Armistice of 11 November 1918 also caused outbreaks in Lima and Nairobi , but by December the wave was mostly over. [46] American Expeditionary Force victims of the Spanish flu at U.S. ... Similarly, in Western Samoa 22% of the population of 38,000 died within two months. [141] In Istanbul , capital of the Ottoman Empire, 6,403 [142] to 10,000 [41] died, giving the city a mortality rate of at least 0,56%. [142] In New Zealand , the flu killed an estimated 6,400 Pakeha and 2,500 indigenous Maori in six weeks, with Māori dying at eight times the rate of Pakeha. [143] [144] In the US, about 28% of the population of 105 million became infected, and 500,000 to 850,000 died (0.48 to 0.81 percent of the population). [145] [146] [147] Native American tribes were particularly hard hit.
-
Cannabinoid Hyperemesis Syndrome
Wikipedia
One woman in the study reported that warm baths provided the only relief from the nausea, severe vomiting, and stomach pain and reportedly burned herself in a hot water bath three times trying to get relief. [25] Society and culture [ edit ] CHS is not very well known. [26] Some emergency room physicians have referred to the symptoms as "scromiting," a portmanteau of "screaming" and "vomiting." [27] In lieu of a correct diagnosis, the average patient in the US may be charged $100,000 or more in medical bills through emergency department visits. [26] An emergency department physician in 2018 commented that the condition wasn't on their "radar" in the 5 years prior, though the condition was being diagnosed more often now. [28] Many people are struck by the notion that cannabis could induce symptoms of nausea and vomiting, given the common perception that cannabis can be used to prevent nausea and vomiting. [28] Research directions [ edit ] It is unclear why CHS is disproportionately uncommon in recognition of how widely used cannabis is throughout the world.
-
Calculus (Dental)
Wikipedia
Domestic pets, such as dogs and cats , frequently accumulate large calculus deposits. [28] Animals with highly abrasive diets, such as ruminants and equids , rarely form thick deposits and instead tend to form thin calculus deposits that often have a metallic or opalescent sheen. [29] In animals, calculus should not be confused with crown cementum , [30] a layer of calcified dental tissue that encases the tooth root underneath the gingival margin and is gradually lost through periodontal disease. ... "Dental biofilms: difficult therapeutic targets". Periodontology 2000 . 28 (1): 12–55. doi : 10.1034/j.1600-0757.2002.280102.x .
-
Otitis Media
Wikipedia
These risk factors increase the incidence and duration of OME during the first two years of life. [28] Chronic suppurative otitis media [ edit ] Chronic suppurative otitis media (CSOM) is a chronic inflammation of the middle ear and mastoid cavity that is characterised by discharge from the middle ear through a perforated tympanic membrane for at least 6 weeks. ... Medscape. Archived from the original on 28 March 2013 . Retrieved 17 March 2013 . ^ Laine MK, Tähtinen PA, Ruuskanen O, Huovinen P, Ruohola A (May 2010). ... S2CID 24036039 . ^ Shaikh N, Hoberman A, Rockette HE, Kurs-Lasky M (March 28, 2012). "Development of an algorithm for the diagnosis of otitis media" (PDF) . ... ISBN 978-0-323-35776-0 . ^ a b Fortanier, Alexandre C.; Venekamp, Roderick P.; Boonacker, Chantal Wb; Hak, Eelko; Schilder, Anne Gm; Sanders, Elisabeth Am; Damoiseaux, Roger Amj (28 May 2019). "Pneumococcal conjugate vaccines for preventing acute otitis media in children" .RSPH4A, TNF, A2ML1, IL6, MUC5AC, IL1B, IL10, FBXO11, BPIFA1, RPL38, SH3PXD2B, MUC4, TGIF1, MUC1, IL1A, FGFR1, MECOM, EYA4, NF2, E2F4, NAGLU, SCGB1A1, DNAH5, TP73, BTC, CTSL, TBX1, CTSK, CTSB, CBY1, SCN2B, EDARADD, IDUA, LMNA, PHEX, ENPP1, CAT, SALL4, NOS2, CXCR4, PNP, TNFSF11, CD3D, CYBC1, CCDC47, DCLRE1C, NSD1, SLC2A1, NCF1, PRX, TCIRG1, BTK, WAS, NBN, NCF2, NCF4, ALMS1, CD3E, CD247, IKBKB, TLK2, FGFR3, DNAAF3, RPGR, IL2RG, RAG2, NIPBL, RAG1, IL7R, RNF168, CYBB, CYBA, CLCN7, PTPRC, SNX10, STX17-AS1, CCDC39, MBL2, TLR2, TLR4, CD14, TLR9, CASP3, DUSP1, COPD, PYCARD, MBL3P, DEFB4A, STS, MCPH1, DHRS2, DEFB4B, MPO, MUC5B, CCR2, CAPN14, SFTPA2, TRAP, SFTPA1, KAT5, MIR146B, SMC2, POLD4, ADAMTS13, NISCH, MIR146A, CFAP97, FLVCR1, TIPRL, CRYGEP, SLC25A21, ITFG1, METTL8, PACC1, PPP2R2D, GALNT14, POLE4, PORCN, ABO, PIK3CD, VEGFA, ELANE, KRT5, ITGB2, ITGAM, ITGAL, ITGA5, CXCL8, IL6R, IL5, IL2, IFNG, FUT2, ATN1, CD46, CRYGC, COL2A1, CD44, CASP9, CASP1, VPS51, C7, BPI, AQP1, AQP8, AKT1, LIMK1, MEFV, TLR5, PIK3CG, SLC11A1, CCL3, CCL2, S100B, S100A12, S100A9, S100A8, S100A1, RAC1, PTEN, PIP, JAG1, MIF, PIK3CB, PIK3CA, PAX9, PAK1, SERPINE1, OPHN1, NT5E, MUC2, MMP9, MMP8, MMP2, H3P5
-
Bronchitis
Wikipedia
No specific testing is normally needed in order to diagnose acute bronchitis. [19] Treatment [ edit ] One form of prevention is to avoid smoking and other lung irritants. [20] Frequent hand washing may also be protective. [20] Treatment for acute bronchitis usually involves rest, paracetamol (acetaminophen), and NSAIDs to help with the fever. [7] [8] Cough medicine has little support for its use, and is not recommended in children under the age of six. [4] [21] There is tentative evidence that salbutamol may be useful in treating wheezing ; however, it may result in nervousness and tremors. [4] [22] Antibiotics should generally not be used. [18] An exception is when acute bronchitis is due to pertussis . [4] Tentative evidence supports honey and pelargonium to help with symptoms. [4] Getting plenty of rest and drinking enough fluids are often recommended as well. [23] Chinese medicinal herbs are of unclear effect. [24] Epidemiology [ edit ] Acute bronchitis is one of the most common diseases. [7] [14] About 5% of adults are affected, and about 6% of children have at least one episode a year. [2] [15] It occurs more often in the winter. [2] More than 10 million people in the US visit a doctor each year for this condition, with about 70% receiving antibiotics which are mostly not needed. [7] There are efforts to decrease the use of antibiotics in acute bronchitis. [14] Acute bronchitis is the most common type of bronchitis. [5] Chronic bronchitis [ edit ] See also: Chronic obstructive pulmonary disease Chronic bronchitis is defined as a productive cough that lasts for three months or more per year for at least two years. [1] [10] When this occurs together with decreased airflow it is known as chronic obstructive pulmonary disease (COPD). [25] [26] Many people with chronic bronchitis have COPD however, most people with COPD do not have chronic bronchitis. [10] [27] Estimates of the number of people with COPD who have chronic bronchitis are 7 to 40%. [28] [29] Estimates of the number of people who smoke and have chronic bronchitis who also have COPD is 60%. [30] The term "chronic bronchitis" was used in previous definitions of COPD but is no longer included in the definition. [10] [31] [32] The term is still used clinically. [33] While both chronic bronchitis and emphysema are often associated with COPD, neither is needed to make the diagnosis. [33] A Chinese consensus commented on symptomatic types of COPD that include chronic bronchitis and with frequent exacerbations. [34] Chronic bronchitis is a respiratory disease marked by overproduction of mucus and mucins . [9] [35] The excess mucus is produced by goblet cells and enlarged submucosal glands in response to long-term irritation. [36] The mucous glands in the submucosa secrete more than the goblet cells. [37] Mucins thicken mucus, and their concentration has been found to be high in cases of chronic bronchitis, and also to correlate with the severity of the disease. [38] Excess mucus can narrow the airways, thereby limiting airflow and accelerating the decline in lung function, and result in COPD. [34] [39] Excess mucus shows itself as a chronic productive cough and its severity and volume of sputum can fluctuate in periods of acute exacerbations. [34] In COPD, those with the chronic bronchitic phenotype with associated chronic excess mucus, experience a worse quality of life than those without. [34] The increased secretions are initially cleared by coughing. [35] The cough is often worse soon after awakening, and the sputum produced may have a yellow or green color and may be streaked with specks of blood. [40] In the early stages, a cough can maintain mucus clearance. ... Retrieved 30 December 2012 . ^ "Industrial bronchitis: MedlinePlus Medical Encyclopedia" . medlineplus.gov . Retrieved 28 May 2019 . ^ "What Causes COPD" .HDAC2, RNF168, COPD, CFTR, ATR, XBP1, MAPK8, PTGDS, RAB5A, RAG1, ROS1, SARS1, CCL5, TGFB1, TP53, VEGFA, PLA2G6, XPC, PLOD1, TNFRSF18, KEAP1, POSTN, HPGDS, SGSM3, SARS2, ERVK-6, HDAC11, SPECC1, MIR146A, MAPK1, PDE4A, CD59, GPT, CRP, CSF2, EGFR, ELANE, ELN, EPHB2, EPHX1, ERN1, FOXJ1, FLNA, GABPA, GYPA, NFE2L2, GYPB, GYPE, IFNA1, IFNA13, IL1RN, IL4, CXCL8, IRF4, LTA, MBL2, MUC5AC, ERVK-32
-
Wernicke Encephalopathy
Wikipedia
There may be tachycardia, dyspnea, chest pain, orthostatic hypotension, changes in heart rate and blood pressure. [26] The lack of thiamine sometimes affects other major energy consumers, the myocardium, and also patients may have developed cardiomegaly. [27] Heart failure with lactic acidosis syndrome has been observed. [28] Cardiac abnormalities are an aspect of the WE, which was not included in the traditional approach, [3] [29] and are not classified as a separate disease. ... "Characteristics of the memory loss of a patient with Wernicke-Korsakoff's syndrome without alcoholism". Neuropsychologia . 28 (2): 171–9. doi : 10.1016/0028-3932(90)90099-A .
-
Emergent Virus
Wikipedia
In order to overcome host-range restrictions and sustain efficient human-human transmission, viruses originating from an animal reservoir will normally undergo mutation , genetic recombination and reassortment . [20] Due to their rapid replication and high mutation rates, RNA viruses are more likely to successfully adapt for invasion of a new host population. [3] Examples of animal sources [ edit ] Bats [ edit ] Different bat species While bats are essential members of many ecosystems, [24] they are also frequently implicated as frequent sources of emerging virus infections. [25] Their immune systems have evolved in such a way as to suppress any inflammatory response to viral infections, thereby allowing them to become tolerant hosts for evolving viruses, and consequently provide major reservoirs of zoonotic viruses. [26] They are associated with more zoonotic viruses per host species than any other mammal, and molecular studies have demonstrated that they are the natural hosts for several high-profile zoonotic viruses, including severe acute respiratory syndrome-related coronaviruses and Ebola / Marburg hemorrhagic fever filoviruses. [27] In terms of their potential for spillover events, bats have taken over the leading role previously assigned to rodents. [26] Viruses can be transmitted from bats via several mechanisms, including bat bite, [28] aerosolization of saliva (e.g. during echolocation ) and faeces/urine. [29] Due to their distinct ecology /behaviour, bats are naturally more susceptible to viral infection and transmission. ... Emerging Infectious Diseases . 6 (4): 319–28. doi : 10.3201/eid0604.000401 . PMC 2640881 .