-
Mass Psychogenic Illness
Wikipedia
American Family of Family Physicians: 15 Dec. 2000. Web. 28 Nov. 2009. ^ a b Phoon, W. H. (1982). ... Archived from the original on 2020-05-28 . Retrieved 2020-10-10 . ^ Josefsson, Janne (October 2, 2019). ... Current Opinion in Psychiatry 19(2) (2006): 171–74. Research Gate. Web. 28 Nov. 2009. Bartholomew, Robert. Little Green Men, Meowing Nuns and Head-Hunting Panics. ... The British Journal of Psychiatry 2002; 180: 300–06. Web. 28 Nov. 2009. [3] Jones, Timothy. "Mass Psychogenic Illness: Role of the Individual Physician." ... American Family of Family Physicians: 15 Dec. 2000. Web. 28 Nov. 2009. [4] Kerchoff, Alan C. "Analyzing a Case of Mass Psychogenic Illness."
-
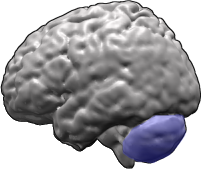
Spinocerebellar Ataxia
Wikipedia
CAG repeat , 19p Calcium channel gene SCA7 [14] ( ATXN7 ) 3rd–4th decade (0.5–60) 20 years (1–45; early onset correlates with shorter duration) Macular degeneration , upper motor neuron , slow saccades CAG repeat , 3p ( Ataxin 7 ) SCA8 [15] ( IOSCA ) 39 yrs (18–65) Normal lifespan Horizontal nystagmus (a rapid, involuntary, oscillatory motion of the eyeball ), instability, lack of coordination CTG repeat , [16] 13q SCA10 [17] ( ATXN10 ) 36 years 9 years ataxia , seizures Mexico Chromosome 22q linked pentanucleotide repeat SCA11 ( TTBK2 ) 30 yrs (15–70) Normal lifespan Mild, remain ambulatory (able to walk about on one's own) 15q SCA12 [18] ( PPP2R2B ) 33 yrs (8–55) Head and hand tremor , akinesia (loss of normal motor function, resulting in impaired muscle movement) CAG repeat , 5q SCA13 ( KCNC3 ) Childhood or adulthood depending on mutation Depending on KCNC3 (a kind of gene) Mental retardation 19q SCA14 [19] ( PRKCG ) 28 yrs (12–42) Decades (1–30) Myoclonus (a sudden twitching of muscles or parts of muscles, without any rhythm or pattern, occurring in various brain disorders) 19q SCA16 ( ITPR1 ) 39 yrs (20–66) 1–40 years Head and hand tremor 8q SCA17 ( TBP ) CAG repeat , 6q (TATA-binding protein) SCA19 , SCA22 ( KCND3 [20] ) Mild cerebellar syndrome , dysarthria SCA25 1.5–39 yrs Unknown ataxia with sensory neuropathy , vomiting and gastrointestinal pain . 2p SCA27 [21] ( FGF14 [20] ) 15–20 yrs Unknown ataxia with poor cognition , dyskinesias and tremor . ... Name OMIM RareDiseases Other Anemia, sideroblastic spinocerebellar ataxia; Pagon Bird Detter syndrome 301310 Disease ID 668 at NIH 's Office of Rare Diseases Friedreich's ataxia; Spinocerebellar ataxia, Friedreich 229300 Disease ID 6468 at NIH 's Office of Rare Diseases Infantile onset Spinocerebellar ataxia 605361 Disease ID 4062 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 1 164400 Disease ID 4071 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 2 183090 Disease ID 4072 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 3; Machado Joseph disease 109150 Disease ID 6801 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 4 600223 Disease ID 9970 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 5 600224 Disease ID 4953 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 7 164500 Disease ID 4955 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 8 603680 Disease ID 4956 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 13 605259 Disease ID 9611 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 18 607458 Disease ID 9976 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 19 607346 Disease ID 9969 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 20 608687 Disease ID 9997 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 21 607454 Disease ID 9999 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 23 610245 Disease ID 9950 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 25 608703 Disease ID 9996 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 26 609306 Disease ID 9995 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 28 610246 Disease ID 9951 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 30 117360 Disease ID 9975 at NIH 's Office of Rare Diseases Spinocerebellar ataxia 35 613908 Disease ID at NIH 's Office of Rare Diseases Spinocerebellar ataxia amyotrophy deafness syndrome Disease ID 2451 at NIH 's Office of Rare Diseases ORPHA:2074 at Orphanet Spinocerebellar ataxia, autosomal recessive 1 606002 Disease ID 4949 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, autosomal recessive 3 271250 Disease ID 9971 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, autosomal recessive 4 607317 Disease ID 4952 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, autosomal recessive 5 606937 Disease ID 9977 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, autosomal recessive 6 608029 Disease ID 4954 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, autosomal recessive 21 - mutation in SCYL1 Online Mendelian Inheritance in Man (OMIM): 616719 ORPHA:466794 Spinocerebellar ataxia, autosomal recessive, with axonal neuropathy 607250 Disease ID 10000 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, X-linked, 2 302600 Disease ID 9978 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, X-linked, 3 301790 Disease ID 9981 at NIH 's Office of Rare Diseases Spinocerebellar ataxia, X-linked, 4 301840 Disease ID 9980 at NIH 's Office of Rare Diseases Treatment [ edit ] Medication [ edit ] There is no cure for spinocerebellar ataxia, which is currently considered to be a progressive and irreversible disease, although not all types cause equally severe disability. [22] In general, treatments are directed towards alleviating symptoms, not the disease itself. ... Beverly Davidson has been working on a methodology using RNAi technology to find a potential cure for over 2 decades. [28] Her research began in the mid-1990s and progressed to work with mouse models about a decade later and most recently has moved to a study with non-human primates. ... In GeneReviews Brussino, Alessandro; Brusco, Alfredo; Dürr, Alexandra (7 February 2013). Spinocerebellar Ataxia Type 28 . University of Washington, Seattle.
-
Hyperthymesia
Wikipedia
His right amygdala , however, was 20% larger, with enhanced functional connectivity between the right amygdala and hippocampus and in other regions. [28] In 2016, HK's remarkable life story was published by HarperCollins Christian Publishing in a book entitled "The Awakening of HK Derryberry: My Unlikely Friendship with the Boy Who Remembers Everything". ... Retrieved 2014-05-29 . ^ Patihis, Lawrence (2015-08-28). "Individual differences and correlates of highly superior autobiographical memory" . ... "MRIs reveal possible source of woman's super-memory" . USA Today . January 28, 2009 ^ Svoboda, Eva; McKinnon, MC; Levine, B (27 June 2006). ... British Psychological Society . Retrieved 28 June 2012 . ^ In 2016, HK's life story was published by HarperCollins Christian Publishing in "The Awakening of HK Derryberry: My Unlikely Friendship with the Boy Who Remembers Everything," which detailed his medical condition. [1] ^ Audrey Ward (2012-09-23).
-
Salmonellosis
Wikipedia
Though Salmonella infection is frequently the cause of osteomyelitis in people with sickle-cell, it is not the most common cause, which is Staphylococcus infection. [13] Those infected may become asymptomatic carriers, but this is relatively uncommon, with shedding observed in only 0.2 to 0.6% of cases after a year. [14] Causes [ edit ] An infographic illustrating how Salmonella bacteria spread from the farm Contaminated food, often having no unusual look or smell [15] Poor kitchen hygiene, especially problematic in institutional kitchens and restaurants because this can lead to a significant outbreak Excretions from either sick or infected but apparently clinically healthy people and animals (especially dangerous are caregivers and animals) Polluted surface water and standing water (such as in shower hoses or unused water dispensers) Unhygienically thawed poultry (the meltwater contains many bacteria) An association with reptiles (pet tortoises, snakes, iguanas, [16] [17] and aquatic turtles) is well described. [18] Amphibians such as frogs Salmonella bacteria can survive for some time without a host; they are frequently found in polluted water, with contamination from the excrement of carrier animals being particularly important. [ citation needed ] The European Food Safety Authority highly recommends that when handling raw turkey meat, consumers and people involved in the food supply chain should pay attention to personal and food hygiene. [19] An estimated 142,000 Americans are infected each year with Salmonella Enteritidis from chicken eggs , [20] and about 30 die. [21] The shell of the egg may be contaminated with Salmonella by feces or environment, or its interior (yolk) may be contaminated by penetration of the bacteria through the porous shell or from a hen whose infected ovaries contaminate the egg during egg formation. [22] [23] Nevertheless, such interior egg yolk contamination is theoretically unlikely. [24] [25] [26] [27] Even under natural conditions, the rate of infection was very small (0.6% in a study of naturally contaminated eggs [28] and 3.0% among artificially and heavily infected hens [29] ). ... Current Opinion in Gastroenterology . 28 (1): 24–9. doi : 10.1097/mog.0b013e32834c453e . ... "Are the bacteria that make food smell and taste bad the same ones that make you sick?" . Tufts.edu . Retrieved 28 May 2018 . ^ "Reptile-Associated Salmonellosis—Selected States, 1998–2002" . ... EFSA Journal . 10 (9): 2893. 21 September 2012. doi : 10.2903/j.efsa.2012.2893 . ^ "Playing It Safe With Eggs" . FDA Food Facts . 2013-02-28. Archived from the original on 2013-03-01 .TNF, SPI1, IFNG, NLRC4, IL12RB1, TLR4, IL23A, IL1B, ACTB, IL18, IL15, IL12B, HAMP, RIPK3, HDAC11, PARP1, CASP1, CLDN2, IL24, LILRB4, EBNA1BP2, PDPN, RIPK1, LILRB2, LANCL1, KAT5, YAP1, OPTN, RABEPK, IFITM3, TRIM32, ARHGEF2, UCHL5, NT5C2, MPRIP, DEFB4B, MIR27B, MIR155, ARMH1, CLEC12A, IL23R, TMUB1, ASRGL1, NOD2, PERP, ATG16L1, KRT20, CYRIB, AXIN1, FOXP3, SLC40A1, SUMF2, TP63, SULT1A1, TRPV1, CXCR3, IL17A, IL9, CXCL8, IL2, IFN1@, HSPA8, HSPA4, CFH, EPO, VIM, DEFB4A, DEFB1, ABCC2, CEBPB, CD38, MS4A1, CALCA, ALPL, INSRR, ITGAE, ITGAM, RPSA, EZR, ADAR, STAT3, SNX1, RGS2, RASA1, PTGS2, PTEN, PSMD7, MAPK1, NT5E, NCAM1, MYD88, MUC2, SMAD7, SMAD2, LBP, H3P28
-
Diseases Of Affluence
Wikipedia
In 1980 less than 1% of Chinese adults were affected by diabetes, but by 2008 the prevalence was 10%. [27] It is predicted that by 2030 diabetes may affect 79.4 million people in India, 42.3 million people in China and 30.3 million in United States. [28] These changes are the result of developing nations having rapid economic development. ... The prevalence of diabetes in rural population is 1/4th that of urban population for countries like India, Bangladesh, Nepal, Bhutan and Sri Lanka. [28] Cardiovascular disease [ edit ] Cardiovascular disease refers to a disease of the heart and blood vessels. ... Behavioral and Brain Sciences . ^ "Products - Data Briefs - Number 288 - October 2017" . www.cdc.gov . 2017-11-28 . Retrieved 2018-09-30 . ^ "Diabetes Overview - Australian Institute of Health and Welfare" . ... Retrieved 2018-09-29 . ^ a b c "Heart Disease Facts & Statistics | cdc.gov" . www.cdc.gov . 2017-11-28 . Retrieved 2018-09-29 . ^ Public Health Agency of Canada (2017-08-22).
-
Bloom Syndrome
Gene_reviews
Abnormalities in insulin release and glucose tolerance have been detected in the eight healthy children (ages 9 months to 13 years) and the three healthy young adults with BSyn (ages 22, 28, and 28 years) appropriately studied [Diaz et al 2006]. ... The 226 Malignant Neoplasms Diagnosed in 145 Persons in the Bloom Syndrome Registry (1954-2018) View in own window Malignancy Type / Tissue Subtype Frequency Age at Diagnosis (years) Median Mean Range Leukemia Acute myeloid 17 21 19 6-32 Acute lymphoblastic 11 14 17 4-40 Other/biphenotypic/undefined 12 18 19 2-40 Lymphoma -- 37 20 21 4-49 Oropharyngeal Tongue 9 37 37 30-48 Pharynx 6 32 34.8 31-45 Tonsil 4 40 38 25-46 Other 5 NA NA NA Upper GI Esophageal 5 39 37 25-48 Gastric 5 31 29 24-33 Other 4 NA NA NA Colorectal -- 28 37 35 16-49 Genitourinary Cervical 5 22 21 19-23 Other 9 NA NA NA Breast -- 24 33 33 21-52 Skin Basal cell 13 29 28 18-38 Squamous cell (uncategorized) 5 35 35 35-36 Other/undefined 4 NA NA NA Wilms tumor -- 8 3 3 1-8 Lung -- 4 37 36 32-40 All other -- 12 NA NA NA GI = gastrointestinal Adapted from Cunniff et al [2018] Genotype-Phenotype Correlations Homozygotes and compound heterozygotes.BLM, UNG, NSMCE2, WRN, LIG1, TP53, ATM, RECQL4, HFM1, TOPBP1, GABPA, MYC, NFE2L2, FES, IL6, FANCC, GYPA, FANCM, TGFB1, RAD51, TNF, LBR, BRCA1, H2AX, EXO1, BRCA2, MPO, DNA2, MUS81, XRS, LTBP4, TP53BP1, CCL27, SOD1, SOD2, NXF1, MVP, TXN, NREP, UBE2I, TOP3A, HSPB3, ARID5A, TOP2B, ADAM15, TRBV20OR9-2, XPA, THY1, USO1, RAD54L, ACTB, SEC14L2, DMC1, TCHP, POLD4, HPSE2, TNMD, MCPH1, ASRGL1, BRIP1, SLX4, CHEK2, LCS1, TSLP, RMI2, FOXR2, NCF1, VPS9D1-AS1, IFT80, SLC12A9, ANKH, NAT10, RIF1, MS4A12, CYCS, NOX4, APOBEC3C, PDLIM3, SMR3A, FGF21, ATRNL1, SUMO3, SPIDR, SIRT1, TREX1, SUMO2, RAD51D, SMN2, FN1, FANCD2, FANCB, FANCF, FEN1, FGF2, FLNB, FXN, SMN1, MTOR, GP1BA, GPR17, GYPB, GYPE, HIF1A, ESR1, EIF4E, EIF2S1, EDNRA, DDX1, CYLD, CYBB, CRYGD, CDKN1A, CDA, SERPINH1, CBL, CAT, CASP3, ATR, ATHS, APRT, HLA-A, HSPB1, HSPB2, PITX3, SLPI, SELP, CCL2, SCN5A, SCD, SERPINB3, ALPP, PTX3, PTPRC, PRKAR1A, PML, PLAUR, PLAT, PKM, SERPINA1, IL4, PRKN, SERPINE1, MSH2, MMP2, MLH1, MFAP1, MDM2, SMAD3, LIG4, LCAT, KRT10, ITGB3, ITGA2B, IL17A, MFT2
-
Pseudoxanthoma Elasticum
Wikipedia
This is the main source of circulating pyrophosphate (PPi), and individuals affected by PXE have strongly reduced plasma PPi levels, explaining their mineralization disorder. [19] One study suggested that mutations causing total absence of an ABCC6 protein caused a more severe disease, [20] but this could not be confirmed in a subsequent case series. [21] Given the variations in age of onset and severity it is likely that other unknown risk factors (genetic, environmental, and lifestyle) may be involved. [3] Premature atherosclerosis is also associated with mutations in the ABCC6 gene, even in those without PXE. [22] A syndrome almost indistinguishable from hereditary PXE has been described in patients with hemoglobinopathies ( sickle-cell disease and thalassemia ) through a poorly understood mechanism. [3] In addition, there appears to be another PXE-like syndrome with a similar phenotype but as a result of problems with another gene, gamma-glutamyl carboxylase . [23] Mutations in ABCC6 can also cause generalized arterial calcification of infancy. [24] In some cases of PXE, mutations in ABCC6 cannot be found, and other genes such as ENPP1 may be implicated [25] Pathophysiology [ edit ] In PXE, there is mineralization (accumulation of calcium and other minerals) and fragmentation of the elastin -containing fibers in connective tissue , but primarily in the midlaminar layer of the dermis, Bruch's membrane and the midsized arteries . [26] Recent studies have confirmed that PXE is a metabolic disease, and that its features arise because metabolites of vitamin K cannot reach peripheral tissues. [27] Low levels of PPi cause mineralization in peripheral tissues. [19] Diagnosis [ edit ] Histopathology of pseudoxanthoma elasticum: Fragmentation and calcification of middermal elastic fibers on Alizarin Red staining. [28] The diagnostic criteria for PXE are the typical skin biopsy appearance and the presence of angioid streaks in the retina. ... Diagnostic histopathological changes in lesional skin: Calcified elastic fibers in the mid and lower dermis, confirmed by positive calcium stain Differential diagnosis [ edit ] The differential diagnosis PXE-like papillary dermal elastolysis : Small flesh-colored papules in the neck region. [28] Histopathology of PXE-like papillary dermal elastolysis: Loss of elastic fibers in the papillary dermis and abnormal pattern in the reticular dermis (arrow) [28] Pseudoxanthoma elasticum versus histopathological differential diagnoses on light microscopy (LM) and electron microscopy (EM) [28] Pseudoxanthoma elasticum LM: Mid-dermal calcification and fragmentation of elastic fibers EM: Mineralization in elastic fiber core PXE-like disease with coagulation deficiency LM: Middermal calcification and fragmentation of elastic fibers EM: Mineralization in elastic fiber periphery Hemoglobinopathies LM: Middermal calcification and fragmentation of elastic fibers EM: Mineralization in elastic fiber core PXE-like papillary dermal elastolysis LM: Selective elastic tissue elimination in the papillary dermis and presence of melanophages White fibrous papulosis of the neck LM: Dermal fibrosis in papillary and mid-reticular dermis Late-onset focal dermal elastosis EM: Decrease of elastic fibers; fragmentation of remaining fibers LM: Accumulation of elastic fibers in mid- and reticular dermis without fragmentation or calcification Perforating calcific elastosis LM: Middermal calcification and degeneration of elastic fibers with transepidermal elimination Buschke-Ollendorff syndrome LM: Increased amount of hypertrophic elastic fibers in dermis EM: Altered translucent elastic fibers Elastosis perforans serpiginosa LM: Transepidermal or perifollicular perforating canals Papular elastorrhexis LM: Thickening of collagen bundles next to loss and fragmentation of elastic fibers Upper dermal elastolysis LM: Complete loss of elastic fibers in the upper dermis Middermal elastolysis LM: Complete absence of elastic fibers in the middermis Linear focal elastosis LM: Massive basophilic fibers; clumping of elastic fibers in papillary dermis Elastoderma LM: Increased, intertwining thin elastic fibers in papillary and upper reticular dermis Calcinosis cutis LM: Deposits of calcium in the dermis Treatment [ edit ] There is no confirmed treatment that directly interferes with the disease process. [5] [6] Cosmetic surgery to remove excessive skin has been used to improve aesthetic appearance in PXE patients [5] but because of the non-life-threatening nature of these symptoms, should be used with caution. [6] One of the most critical symptom of PXE is choroidal neovascularization which can lead to deterioration of central vision.
-
Cysticercosis
Wikipedia
The proposed strategy for eradication is to do multilateral intervention by treating both human and porcine populations. [27] It is feasible because treating pigs with oxfendazole has been shown to be effective and once treated, pigs are protected from further infections for at least 3 months. [28] Limitations [ edit ] Even with the concurrent treatment of humans and pigs, complete elimination is hard to achieve. ... Archived from the original on 4 December 2014 . Retrieved 28 November 2014 . ^ a b c Markell, E.K.; John, D.T.; Krotoski, W.A. (1999). ... Clinics in Laboratory Medicine . 11 (4): 1011–28. doi : 10.1016/S0272-2712(18)30532-8 . ... American Journal of Neuroradiology . 28 (8): 1501–1504. doi : 10.3174/ajnr.A0623 .
-
Squamous Cell Skin Cancer
Wikipedia
Unlike basal-cell carcinomas , SCCs carry a higher risk of metastasis , and may spread to the regional lymph nodes , [25] Erythroplasia of Queyrat (SCC in situ of the glans or prepuce in males, [26] M [27] : 733 [28] : 656 [29] or the vulvae in females. [30] ) may be induced by human papilloma virus . [31] It is reported to occur in the corneoscleral limbus . [32] Erythroplasia of Queyrat may also occur on the anal mucosa or the oral mucosa. [33] Some sources state that this condition is synonymous with Bowen's disease , [30] however generally speaking Bowen's disease refers to carcinoma in situ of any location on the skin such as the lower leg. ... Squamous cell carcinoma in situ , showing prominent dyskeratosis and aberrant mitoses at all levels of the epidermis, along with marked parakeratosis. [12] In situ disease [ edit ] Bowen's disease is essentially equivalent to and used interchangeably with SCC in situ , when not having invaded through the basement membrane . [12] Depending on source, it is classified as precancerous [13] or SCC in situ (technically cancerous but non-invasive). [38] [39] In SCC in situ (Bowen's disease), atypical squamous cells proliferate through the whole thickness of the epidermis. [12] The entire tumor is confined to the epidermis and does not invade into the dermis. [12] The cells are often highly atypical under the microscope , and may in fact look more unusual than the cells of some invasive squamous cell carcinomas. [12] SCC in situ , high magnification, demonstrating an intact basement membrane. [12] SCC in situ SCC in situ SCC in situ SCC in situ Erythroplasia of Queyrat is a particular type of Bowen's disease that can arise on the glans or prepuce in males, [26] [27] : 733 [28] : 656 [29] and the vulvae in females. [30] It mainly occurs in uncircumcised males, [30] [40] over the age of 40. [33] It is named for French dermatologist Louis Queyrat (1856–1933), [41] [42] [43] who was head of the dermatology service of l'Hôpital Ricord, a venereal hospital in Paris, now Hôpital Cochin . [44] Invasive disease [ edit ] In invasive SCC, tumor cells infiltrate through the basement membrane. ... PMID 20935675 . ^ "Cutaneous Squamous Cell Carcinoma: Practice Essentials, Background, Pathophysiology" . 28 June 2016. Archived from the original on 6 April 2017 . Retrieved 15 March 2017 . ^ "Cutaneous Squamous Cell Carcinoma: Practice Essentials, Background, Pathophysiology" . 28 June 2016. Archived from the original on 6 April 2017 .BRAF, FYN, CDKN2A, TP53, HRAS, KNSTRN, COL7A1, TERT, OCA2, AHR, MC1R, RSPO1, ERBB2, IRF4, TERC, ERCC4, LAMB3, LAMA3, KRT14, KRT5, ERCC3, RALY, BCL2L12, IRF3, CYP21A2, SEC16A, DDB2, LAMC2, GJB6, ERCC2, PIK3CA, GJB2, EGFR, TRPS1, ERCC5, TYR, MMP1, XPC, LMNA, CD274, TINF2, STK19, SLC45A2, RAC1, LPP, CRNKL1, PIK3CG, PIK3CD, PIK3CB, FUT1, PTGS2, CD44, KRT7, EPHB2, MYC, TAL1, STAT3, SCLY, MTCO2P12, BCL2, CCND1, NOTCH1, COX2, VEGFA, GRHL3, SOX2, YAP1, MAPK1, INPP5A, PTEN, RARRES2, H3P10, TMC8, TSPAN1, AKT1, MIR20A, TNF, MIR21, RELA, CDH13, ACKR3, KLF4, SIRT1, MIR497, NET1, COL17A1, SLC6A5, KRT16, MIR135B, TMC6, S100A8, CTNNB1, MIR361, CABIN1, IL10, PRPF38B, LGR5, ATF3, POLH, YBX1, PPARG, KRT20, VIM, CD68, MTHFR, CAMP, CD200, MMP13, MMP9, MS4A1, MIR31, IL22, SRC, CTTN, EGF, MIR186, FOXE1, SLC6A2, EIF4E, MIR205, TGFB1, FGFR2, HOXA9, HOXB7, LINC00319, MIR203A, IGFBP3, MIR30A, EPHA1, PICSAR, HPLH1, DLC1, BECN1, CADM1, SIN3A, CLDN1, ZNRD2, G0S2, SLCO1B3, CFDP1, KYNU, TNFSF12, ARTN, HDAC3, HERC2, CCRL2, CXCL13, CLEC2D, HPGDS, WWP1, SMPX, DAPK2, PPARGC1A, RHOBTB1, LZTS1, PRAF2, PPP1R13L, NLRP1, ZHX2, FAM114A2, HDAC9, TRIM32, EFS, DNM1L, CYFIP1, AIM2, POLQ, DCTN6, CXCR6, SLIT2, SF3B1, LPAR2, BRD4, IGF2BP1, PDPN, TRIM16, USP8, SMUG1, CKAP4, ISG15, ZMIZ1, GEMIN4, MIR143, TNFSF12-TNFSF13, MIR17HG, MIR34A, MIR221, MIR217, MIR204, MIR181A2, MIR154, MIR148A, MIR142, FOPNL, MALAT1, TICAM2, DPH3, CAVIN1, TINCR, PRSS55, RMDN2, KRT72, CD200R1, MIR326, MIR346, MIR424, MIR490, H3P23, LOC110806263, LINC01048, OCLN, LINC00963, MIR3619, MIR1193, TMED7-TICAM2, MIR664A, MIR1238, MIR1207, MIR1247, DEFB4B, HOTAIR, MIR766, LINC00520, POU5F1P4, POU5F1P3, MIR506, RBM45, NLRP3, TMED7, MRGBP, SPHK2, METTL3, PARD3, ERBIN, PAG1, POLR3E, NBPF1, SYBU, ZNF654, RMDN3, TP53RK, DEF8, RETREG1, RIPK4, WWOX, RAB23, SIRT6, TNFRSF12A, RMDN1, NDUFA13, PCBP4, RAB25, TP63, AICDA, LMLN, SPZ1, CARD11, TMPRSS13, ARHGAP24, TCF7L1, TXNDC5, SRCIN1, CD276, PDCD1LG2, UBA5, TNFAIP8L2, MAPKAP1, CARD14, WNK1, GORASP1, LGR6, OVOL2, ANKRD36B, AKR1C3, ADRA1A, DENR, HSD11B2, HLA-DRB1, HLA-DQA1, HIF1A, NR3C1, GRN, GPR42, GPER1, GPR1, GNA12, GLB1, GABPA, FN1, FOXC2, FOXG1, FHL1, FGF10, EFEMP1, FAP, PTK2B, HMGB1, HSF1, ESRRA, TNC, MAGEA12, SMAD4, SMAD2, LIMK1, LAMC1, KTN1, KRT17, KRT8, KRAS, KPNA4, KLKB1, JAK1, IVL, STT3A, ITGB1, IL6, IL1B, RBPJ, IFI27, EZH2, ESR2, MCL1, CKS1B, CDKN2B, CDK9, CDK6, CDH1, CDC25A, CDC20, RUNX1, C3, BRS3, CFB, BAX, AR, AQP3, FAS, APRT, XIAP, APAF1, AGRP, AGER, CHI3L1, CCR5, ESR1, CLDN7, ERCC1, EIF4G2, EGR3, EDNRA, HBEGF, DLX3, TIMM8A, DEFB4A, GADD45A, DAPK1, CD55, CYP3A4, CTNNA1, CTLA4, CCN2, CSHL1, CRMP1, CRIP2, CREBBP, MAL, MCM2, MLRL, ZEB1, SYT1, STAT2, STAT1, SSTR4, SPRR1A, ADRA2B, SOAT1, SLC2A1, ST3GAL1, SFRP5, SFRP1, CXCL12, SDC2, SDC1, CCL8, SERPINB4, SERPINB3, S100A9, S100A7, TCF7L2, PPP1R11, RPE65, TGFBR1, TAF15, SEM1, TFEB, XRCC1, WNT1, NSD2, VSNL1, EZR, VEGFC, VCP, UVRAG, UTRN, USF1, TRAF6, CRISP2, TP73, TLR4, THBS1, TGFBR2, S100A4, RNF2, MAP3K4, PCBP1, PCSK6, PEBP1, OVOL1, CLDN11, OSM, ODC1, NOTCH2, NOS2, NFE2L2, NEDD8, NCAM1, MMUT, MST1, MSMB, MSH2, MMP7, MAP3K9, MLH1, MFAP1, PRKN, CDK16, RET, PDCD1, REN, OPN1LW, RASA1, RAF1, PTPRD, PTGDS, PTCH1, PSMD9, PSMD2, MAP2K7, MAPK8, MAPK3, PPARD, POU5F1, PLK1, PLAT, PIN1, SERPINB9, PDK1, SOX4
-
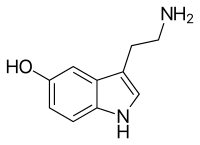
Serotonin Syndrome
Wikipedia
It can take at least four weeks for this enzyme to be replaced by the body in the instance of irreversible inhibitors. [28] With respect to tricyclic antidepressants only clomipramine and imipramine have a risk of causing SS. [29] Many medications may have been incorrectly thought to cause serotonin syndrome. ... The first evaluated criteria were introduced in 1991 by Harvey Sternbach . [4] [28] [55] Researchers later developed the Hunter Toxicity Criteria Decision Rules, which have better sensitivity and specificity , 84% and 97%, respectively, when compared with the gold standard of diagnosis by a medical toxicologist. [4] [8] As of 2007, Sternbach's criteria were still the most commonly used. [7] The most important symptoms for diagnosing serotonin syndrome are tremor, extreme aggressiveness, akathisia , or clonus (spontaneous, inducible and ocular). [8] Physical examination of the patient should include assessment of deep-tendon reflexes and muscle rigidity, the dryness of the mucosa of the mouth , the size and reactivity of the pupils, the intensity of bowel sounds, skin color, and the presence or absence of sweating. [4] The patient's history also plays an important role in diagnosis, investigations should include inquiries about the use of prescription and over-the-counter drugs, illicit substances, and dietary supplements , as all these agents have been implicated in the development of serotonin syndrome. [4] To fulfill the Hunter Criteria, a patient must have taken a serotonergic agent and meet one of the following conditions: [8] Spontaneous clonus , or Inducible clonus plus agitation or diaphoresis , or Ocular clonus plus agitation or diaphoresis , or Tremor plus hyperreflexia , or Hypertonism plus temperature > 38 °C (100 °F) plus ocular clonus or inducible clonus Differential diagnosis [ edit ] Serotonin toxicity has a characteristic picture which is generally hard to confuse with other medical conditions , but in some situations it may go unrecognized because it may be mistaken for a viral illness , anxiety disorders , neurological disorder , anticholinergic poisoning, sympathomimetic toxicity, or worsening psychiatric condition. [4] [7] [56] The condition most often confused with serotonin syndrome is neuroleptic malignant syndrome (NMS). [57] [58] The clinical features of neuroleptic malignant syndrome and serotonin syndrome share some features which can make differentiating them difficult. [59] In both conditions, autonomic dysfunction and altered mental status develop. [51] However, they are actually very different conditions with different underlying dysfunction (serotonin excess vs dopamine blockade). ... More severe cases may require muscular paralysis with vecuronium , intubation , and artificial ventilation. [4] [7] Suxamethonium is not recommended for muscular paralysis as it may increase the risk of cardiac dysrhythmia from hyperkalemia associated with rhabdomyolysis. [4] Antipyretic agents are not recommended as the increase in body temperature is due to muscular activity, not a hypothalamic temperature set point abnormality. [4] Prognosis [ edit ] Upon the discontinuation of serotonergic drugs, most cases of serotonin syndrome resolve within 24 hours, [4] [7] [67] [68] although in some cases delirium may persist for a number of days. [28] Symptoms typically persist for a longer time frame in patients taking drugs which have a long elimination half-life , active metabolites, or a protracted duration of action. [4] Cases have reported muscle pain and weakness persisting for months, [69] and antidepressant discontinuation may contribute to ongoing features. [70] Following appropriate medical management, serotonin syndrome is generally associated with a favorable prognosis. [71] Epidemiology [ edit ] Epidemiological studies of serotonin syndrome are difficult as many physicians are unaware of the diagnosis or they may miss the syndrome due to its variable manifestations. [4] [72] In 1998 a survey conducted in England found that 85% of the general practitioners that had prescribed the antidepressant nefazodone were unaware of serotonin syndrome. [40] The incidence may be increasing as a larger number of pro-serotonergic drugs (drugs which increase serotonin levels) are now being used in clinical practice. [63] One postmarketing surveillance study identified an incidence of 0.4 cases per 1000 patient-months for patients who were taking nefazodone . [40] Additionally, around 14 to 16 percent of persons who overdose on SSRIs are thought to develop serotonin syndrome. [43] Notable cases [ edit ] Phenelzine is a MAOI which contributed to serotonin syndrome in the Libby Zion case The most widely recognized example of serotonin syndrome was the death of Libby Zion in 1984. [73] Zion was a freshman at Bennington College at her death on March 5, 1984, at age 18. ... Archived from the original on 2013-01-26 . Retrieved 2013-01-28 . ^ a b Birmes P, Coppin D, Schmitt L, Lauque D (May 2003). ... Archived from the original on 2013-02-01 . Retrieved 2013-01-28 . ^ Prator B (2006). "Serotonin syndrome".
-
Malignant Hyperthermia
Wikipedia
The higher the score (above 6), the more likely a reaction constituted MH: [27] Respiratory acidosis (end-tidal CO 2 above 55 mmHg/7.32 kPa or arterial pCO 2 above 60 mmHg/7.98 kPa) Heart involvement (unexplained sinus tachycardia , ventricular tachycardia or ventricular fibrillation ) Metabolic acidosis (base excess lower than -8, pH <7.25) Muscle rigidity (generalized rigidity including severe masseter muscle rigidity) Muscle breakdown (CK >20,000/L units, cola colored urine or excess myoglobin in urine or serum, potassium above 6 mmol/l) Temperature increase (rapidly increasing temperature, T >38.8 °C) Other (rapid reversal of MH signs with dantrolene, elevated resting serum CK levels) Family history (autosomal dominant pattern) Prevention [ edit ] In the past, the prophylactic use of dantrolene was recommended for MH-susceptible patients undergoing general anesthesia. [28] However, multiple retrospective studies have demonstrated the safety of trigger-free general anesthesia in these patients in the absence of prophylactic dantrolene administration. ... Only five of these patients exhibited signs consistent with MH, four of which were treated successfully with parenteral dantrolene, and the remaining one recovered with only symptomatic therapy. [29] After weighing its questionable benefits against its possible adverse effects (including nausea, vomiting, muscle weakness and prolonged duration of action of nondepolarizing neuromuscular blocking agents [30] ), experts no longer recommend the use of prophylactic dantrolene prior to trigger-free general anesthesia in MH-susceptible patients. [28] Anesthesia machine preparation [ edit ] Anesthesia for people with known MH susceptible requires avoidance of triggering agent concentrations above 5 parts per million (all volatile anesthetic agents and succinylcholine). ... After the widespread introduction of treatment with dantrolene, the mortality of malignant hyperthermia fell from 80% in the 1960s to less than 5%. [5] Dantrolene remains the only drug known to be effective in the treatment of MH. [28] The recommended dose of dantrolene is 2.5 mg/kg, repeated as necessary. [5] It is recommended that each hospital keeps a minimum stock of 36 dantrolene vials (720 mg), sufficient for four doses in a 70-kg person. [34] Training [ edit ] This is a mixed modality medical simulation of the treatment of malignant hyperthermia by anesthesia residents. ... The Journal of Biological Chemistry . 278 (28): 25722–30. doi : 10.1074/jbc.M302165200 .RYR1, CACNA1S, STAC3, SCN4A, BIN1, EDAR, SCN5A, TRAF6, ELP1, CRLF1, ABCA12, CLCF1, HSPG2, MTMR14, TRAPPC9, KDF1, EDARADD, NALCN, MYF6, MYH3, CHRND, CHRNG, CHRNA1, DNM2, GCDH, RYR2, CASQ1, BCHE, RUNX2, SELENON, CBS, DMD, EPHA3, CBSL, MHS2, CACNA2D1, SNRNP27, SLC24A3, MEPE, EIF3K, CACNA1C, ATP2A1, H19, AICDA, GYPA, SPAG9, GYPB, MHS3, TRPV1, FLNA, QDPR, PRODH, ARVD3, KCNA1, IL6, HTR3A, GPI, HAL, GYPE, COL4A1
-
Acute Liver Failure
Wikipedia
The 1993 classification defines hyperacute as within 1 week, acute as 8–28 days, and subacute as 4–12 weeks; [1] both the speed with which the disease develops and the underlying cause strongly affect outcomes. [2] Contents 1 Signs and symptoms 1.1 Encephalopathy and cerebral edema 1.2 Coagulopathy 1.3 Kidney failure 1.4 Inflammation and infection 1.5 Metabolic derangements 1.6 Haemodynamic and cardio-respiratory compromise 1.7 Late pregnancy 2 Causes 3 Pathophysiology 4 Diagnosis 4.1 Definition 5 Treatment 5.1 General concerns 5.2 Neurologic complications 5.3 Cardiovascular complications 5.4 Pulmonary complications 5.5 Coagulopathy and gastrointestinal bleeding 5.6 Nutrition, electrolytes, and metabolic derangements 5.7 Infection 5.8 Liver transplantation 5.9 Acetylcysteine 6 Prognosis 7 Terminology 8 References 9 External links Signs and symptoms [ edit ] The main features of acute liver failure are rapid-onset jaundice, weakness, and eventually, changes in mental status that can begin as mild confusion but progress to coma. [ citation needed ] Encephalopathy and cerebral edema [ edit ] In ALF, hepatic encephalopathy leads to cerebral edema , coma , brain herniation , and eventually death. ... This is sub-divided into "fulminant hepatic failure", which requires onset of encephalopathy within 8 weeks, and "subfulminant", which describes onset of encephalopathy after 8 weeks but before 26 weeks. [22] Another scheme defines "hyperacute" as onset within 7 days, "acute" as onset between 7 and 28 days, and "subacute" as onset between 28 days and 24 weeks. [21] page 1557 Treatment [ edit ] King's College Hospital criteria for liver transplantation in acute liver failure [23] Patients with paracetamol toxicity pH < 7.3 or Prothrombin time > 100 seconds and serum creatinine level > 3.4 mg/dL (> 300 μmol/l) if in grade III or IV encephalopathy Other patients Prothrombin time > 100 seconds or Three of the following variables : Age < 10 yr or > 40 years Cause: Hepatitis C or E halothane hepatitis idiosyncratic drug reaction Duration of jaundice before encephalopathy > 7 days Prothrombin time > 50 seconds Serum bilirubin level > 17.6 mg/dL (> 300 μmol/l) General concerns [ edit ] Because ALF often involves the rapid deterioration of mental status and the potential for multiorgan failure, patients should be managed in the intensive care unit. [24] For patients not at a transplant center, the possibility of rapid progression of ALF makes early consultation with a transplant facility critical. ... Vasoconstrictive agents (especially vasopressin) should be avoided. [28] Pulmonary complications [ edit ] Pulmonary edema and pulmonary infections are commonly seen in patients with ALF.TNF, ATP7B, HGF, FAS, ALB, IL1RN, GC, MAPK8, KRT8, KRT18, GFER, FASLG, CSF3, SERPINC1, CAST, GPNMB, PANX1, CD74, FST, POMC, SCO1, ALDOB, INHBA, INS, IL6, TLR4, CASP3, NOS3, PTGS2, ABCC2, NOS2, MET, CD14, CASP9, ATM, KCNJ10, PTAFR, CASP12, UCP2, COL1A2, HSPA8, FGA, BRIP1, THBD, INS-IGF2, LTC4S, NBAS, POLG, RINT1, TRMU, FAH, POLG2, JAK2, SCYL1, MST1, PORCN, HADH, GPT, GPR35, VPS13A, MPV17, ITCH, F5, CYC1, RYR1, GFM1, ACAD9, IKZF1, MEFV, CACNA1S, EIF2AK3, LARS1, TCF4, HLA-B, HMGB1, IL1B, F2, CCL4, IL10, MIR122, HMOX1, PPARA, STON1, AFM, GTF2A1L, MIR223, NLRP3, SLC1A2, HDAC2, STON1-GTF2A1L, HDAC6, MSC, IL1A, UGT1A, TP53, SLC17A5, ABCG2, SYT1, CXCL12, PEBP1, OTC, PRKAA1, RELA, WNK1, BCHE, AFP, IFNG, AHSG, GORASP1, GSK3B, PIM3, DDIT3, DGUOK, EXOSC3, BCL2L11, MIR17, MFN2, MIR155, ABCB6, AIM2, BTBD8, YAP1, IFNL3, PPARGC1B, APOA5, PIK3IP1, LMLN, MIR19A, LONP1, MIR210, ATG7, PPIG, MIR214, RGN, TIMELESS, SQSTM1, MIR375, MIR1224, TNFRSF10B, RIPK1, OCLN, BECN1, SOCS1, ARHGEF5, SHANK3, KHDRBS1, TXNIP, KCTD9, HAMP, ACKR3, NAT10, HAVCR1, SIGLEC9, PDLIM3, IGHV1-3, ATRNL1, TLR9, STX18, ERO1A, SCLC1, RRM2B, SLC25A37, CXCL16, NUP62, SERAC1, SLC27A5, DCTN4, CYSLTR1, CCL27, SLA2, EVA1A, TMPRSS13, SESN2, SIRT1, PARP9, ASRGL1, DHDDS, GSDMD, SIRT2, TBC1D9, TFEB, ACADM, VWF, GABPA, CYP2E1, CYP3A4, ESR1, FABP1, FABP7, FBP1, FCGR3A, FCGR3B, FOXO3, G6PD, GFAP, VIP, CXCR3, GTF2H1, HIF1A, HNF4A, HSPA5, HSPG2, ID1, IFNA1, IFNA13, IFNB1, CYP1A2, CX3CR1, CTNNB1, CTLA4, AHR, AKT1, ALAS1, ALPP, AMCN, AQP4, AR, ATHS, BCL2, OPN1SW, BID, BST2, CASP8, CD86, ENTPD1, CD40LG, CEL, CGA, CCR5, KLF6, CRP, IL1R1, IL2, CXCL8, S100A10, CCL2, SDC1, SLC6A12, SLC12A2, SLPI, SOAT1, STAR, STAT1, STAT3, MAP3K7, PPP1R11, TGFB1, TGFBR2, THBS1, THPO, TLR2, TLR3, TNFAIP3, TNFAIP6, TXN, UGT2B7, S100A12, RHD, IL18, ACP3, ITGAM, MARS1, KMT2A, MPO, MSMB, COX2, MYD88, NFE2L2, NT5E, SERPINE1, ABCB1, PIK3CA, PIK3CB, PIM1, PIK3CD, PIK3CG, SERPINF2, PPP2R5A, PRKAA2, PRKAB1, RBP4, MTCO2P12
-
Rocky Mountain Spotted Fever
Wikipedia
Public Health Service was ordered to the region, and he led a research team at an abandoned schoolhouse through about 1924. [27] [28] Spencer was assisted by R. R. Parker, Bill Gettinger, Henry Cowan, Henry Greenup, Elmer Greenup, Gene Hughes, Salsbury, Kerlee, and others, of whom Gettinger, Cowan and Kerlee died of Rocky Mountain spotted fever. [28] Through a series of discoveries, the team found that a previous blood meal was necessary to make the tick deadly to its hosts, as well as other facets of the disease. [28] On May 19, 1924, Spencer put a large dose of mashed wood ticks, from lot 2351B, and some weak carbolic acid into his arm by injection. This vaccine worked, and for some years after it was used by people in that region to convert the illness from one with high fatality rate (albeit low incidence) to one that could be either prevented entirely (for many of them) or modified to a non-deadly form (for the rest). [28] Today there is no commercially available vaccine for RMSF [21] because, unlike in the 1920s when Spencer and colleagues developed one, antibiotics are now available to treat the disease, so prevention by vaccination is no longer the sole defense against likely death.
-
Tetanus
Wikipedia
Hence, stepping on a nail (rusty or not) may result in a tetanus infection, as the low-oxygen (anaerobic) environment may exist under the skin, and the puncturing object can deliver endospores to a suitable environment for growth. [26] It is a common misconception that rust itself is the cause and that a puncture from a rust-free nail is not a risk. [27] [28] Pathophysiology [ edit ] A neurotransmitter-filled vesicle before and after exposure to the tetanus toxin. ... The guidelines for such events in the United States for non-pregnant people 11 years and older are as follows: [1] Vaccination status Clean, minor wounds All other wounds Unknown or less than 3 doses of tetanus toxoid containing vaccine Tdap and recommend catch-up vaccination Tdap and recommend catch-up vaccination Tetanus immunoglobulin 3 or more doses of tetanus toxoid containing vaccine AND less than 5 years since last dose No indication No indication 3 or more doses of tetanus toxoid containing vaccine AND 5–10 years since last dose No indication Tdap preferred (if not yet received) or Td 3 or more doses of tetanus toxoid containing vaccine AND more than 10 years since last dose Tdap preferred (if not yet received) or Td Tdap preferred (if not yet received) or Td Treatment [ edit ] Tetanus deaths per million persons in 2012 0–1 1–2 2–3 4–8 9–13 14–28 29–151 Mild tetanus [ edit ] Mild cases of tetanus can be treated with: [40] Tetanus immunoglobulin (TIG), [1] also called tetanus antibodies or tetanus antitoxin. [39] It can be given as intravenous therapy or by intramuscular injection . ... "Changes in severe accidental tetanus mortality in the ICU during two decades in Brazil" . Intensive Care Med . 28 (7): 930–5. doi : 10.1007/s00134-002-1332-4 . ... "Trismus in cephalic tetanus from a foot injury" . Korean J. Intern. Med . 28 (1): 121. doi : 10.3904/kjim.2013.28.1.121 . ... Recommendations and Reports . 40 (RR-10): 1–28. August 1991. PMID 1865873 . ^ Porter JD, Perkin MA, Corbel MJ, Farrington CP, Watkins JT, Begg NT (1992).
-
Typhoid Fever
Wikipedia
Archived from the original on 6 June 2016 . Retrieved 28 March 2015 . ^ a b c d e f g h i j k l m n Wain J, Hendriksen RS, Mikoleit ML, Keddy KH, Ochiai RL (March 2015). ... Archived from the original on 2 April 2015 . Retrieved 28 March 2015 . ^ a b c d Milligan R, Paul M, Richardson M, Neuberger A (May 2018). ... Archived from the original on 2017-02-28. ^ Chatham-Stephens K, Medalla F, Hughes M, Appiah GD, Aubert RD, Caidi H, et al. ... Archived from the original on 11 January 2008 . Retrieved 28 March 2015 . Resembling or characteristic of typhus ^ "Typhoid" . ... Archived from the original on 2011-11-02 . Retrieved 2007-08-28 . ^ Crump JA, Luby SP, Mintz ED (May 2004).
-
Hiv/aids
Wikipedia
HIV/AIDS Other names HIV disease, HIV infection [1] [2] The red ribbon is a symbol for solidarity with HIV-positive people and those living with AIDS. [3] Specialty Infectious disease , immunology Symptoms Early : Flu-like illness [4] Later : Large lymph nodes , fever, weight loss [4] Complications Opportunistic infections , tumors [4] Duration Lifelong [4] Causes Human immunodeficiency virus (HIV) [4] Risk factors Exposure to blood, breast milk, sex, men who have sex with men , drug users , prisoners , sex workers and their clients [4] Diagnostic method Blood tests [4] Prevention Safe sex , needle exchange , male circumcision , pre-exposure prophylaxis , post-exposure prophylaxis [4] Treatment Antiretroviral therapy [4] Prognosis Near normal life expectancy with treatment [5] [6] 11 years life expectancy without treatment [7] Frequency 55.9 million – 100 million total cases [8] 1.7 million new cases (2019) [8] 38 million living with HIV (2019) [8] Deaths 32.7 million total deaths [8] 690,000 (2019) [8] Human immunodeficiency virus infection and acquired immunodeficiency syndrome ( HIV/AIDS ) is a spectrum of conditions caused by infection with the human immunodeficiency virus (HIV), [9] [10] [11] a retrovirus . [12] Following initial infection a person may not notice any symptoms, or may experience a brief period of influenza-like illness . [4] Typically, this is followed by a prolonged period with no symptoms. [5] If the infection progresses, it interferes more with the immune system , increasing the risk of developing common infections such as tuberculosis , as well as other opportunistic infections , and tumors which are otherwise rare in people who have normal immune function. [4] These late symptoms of infection are referred to as acquired immunodeficiency syndrome (AIDS). [5] This stage is often also associated with unintended weight loss . [5] HIV is spread primarily by unprotected sex (including anal and oral sex ), contaminated blood transfusions , hypodermic needles , and from mother to child during pregnancy , delivery, or breastfeeding. [13] Some bodily fluids, such as saliva, sweat and tears, do not transmit the virus. [14] Methods of prevention include safe sex , needle exchange programs , treating those who are infected , and pre- & post-exposure prophylaxis . [4] Disease in a baby can often be prevented by giving both the mother and child antiretroviral medication . [4] There is no cure or vaccine ; however, antiretroviral treatment can slow the course of the disease and may lead to a near-normal life expectancy. [5] [6] Treatment is recommended as soon as the diagnosis is made. [15] Without treatment, the average survival time after infection is 11 years. [7] In 2018, about 37.9 million people were living with HIV and it resulted in 770,000 deaths. [8] An estimated 20.6 million of these live in eastern and southern Africa. [16] Between the time that AIDS was identified (in the early 1980s) and 2018, the disease caused an estimated 32 million deaths worldwide. [8] HIV/AIDS is considered a pandemic —a disease outbreak which is present over a large area and is actively spreading. [17] HIV made the jump from other primates to humans in west-central Africa in the early-to-mid 20th century. [18] AIDS was first recognized by the United States Centers for Disease Control and Prevention (CDC) in 1981 and its cause—HIV infection—was identified in the early part of the decade. [19] HIV/AIDS has had a large impact on society, both as an illness and as a source of discrimination . [20] The disease also has large economic impacts . [20] There are many misconceptions about HIV/AIDS , such as the belief that it can be transmitted by casual non-sexual contact. [21] The disease has become subject to many controversies involving religion , including the Catholic Church's position not to support condom use as prevention. [22] It has attracted international medical and political attention as well as large-scale funding since it was identified in the 1980s. [23] Play media Video summary ( script ) Contents 1 Signs and symptoms 1.1 Acute infection 1.2 Clinical latency 1.3 Acquired immunodeficiency syndrome 2 Transmission 2.1 Sexual 2.2 Body fluids 2.3 Mother-to-child 3 Virology 4 Pathophysiology 5 Diagnosis 5.1 HIV testing 5.2 Classifications 6 Prevention 6.1 Sexual contact 6.2 Pre-exposure 6.3 Post-exposure 6.4 Mother-to-child 6.5 Vaccination 7 Treatment 7.1 Antiviral therapy 7.2 Opportunistic infections 7.3 Diet 7.4 Alternative medicine 8 Prognosis 9 Epidemiology 10 History 10.1 Discovery 10.2 Origins 11 Society and culture 11.1 Stigma 11.2 Economic impact 11.3 Religion and AIDS 11.4 Media portrayal 11.5 Criminal transmission 11.6 Misconceptions 12 Research 13 References 14 External links Signs and symptoms Main article: Signs and symptoms of HIV/AIDS There are three main stages of HIV infection: acute infection, clinical latency, and AIDS. [1] [24] Acute infection Main symptoms of acute HIV infection The initial period following the contraction of HIV is called acute HIV, primary HIV or acute retroviral syndrome. [24] [25] Many individuals develop an influenza-like illness or a mononucleosis-like illness 2–4 weeks after exposure while others have no significant symptoms. [26] [27] Symptoms occur in 40–90% of cases and most commonly include fever , large tender lymph nodes , throat inflammation , a rash , headache, tiredness, and/or sores of the mouth and genitals. [25] [27] The rash, which occurs in 20–50% of cases, presents itself on the trunk and is maculopapular , classically. [28] Some people also develop opportunistic infections at this stage. [25] Gastrointestinal symptoms, such as vomiting or diarrhea may occur. [27] Neurological symptoms of peripheral neuropathy or Guillain–Barré syndrome also occurs. [27] The duration of the symptoms varies, but is usually one or two weeks. [27] Owing to their nonspecific character, these symptoms are not often recognized as signs of HIV infection. ... Acquired immunodeficiency syndrome (AIDS) is defined as an HIV infection with either a CD4 + T cell count below 200 cells per µL or the occurrence of specific diseases associated with HIV infection. [27] In the absence of specific treatment, around half of people infected with HIV develop AIDS within ten years. [27] The most common initial conditions that alert to the presence of AIDS are pneumocystis pneumonia (40%), cachexia in the form of HIV wasting syndrome (20%), and esophageal candidiasis . [27] Other common signs include recurrent respiratory tract infections . [27] Opportunistic infections may be caused by bacteria , viruses , fungi , and parasites that are normally controlled by the immune system. [34] Which infections occur depends partly on what organisms are common in the person's environment. [27] These infections may affect nearly every organ system . [35] People with AIDS have an increased risk of developing various viral-induced cancers, including Kaposi's sarcoma , Burkitt's lymphoma , primary central nervous system lymphoma , and cervical cancer . [28] Kaposi's sarcoma is the most common cancer, occurring in 10% to 20% of people with HIV. [36] The second-most common cancer is lymphoma, which is the cause of death of nearly 16% of people with AIDS and is the initial sign of AIDS in 3% to 4%. [36] Both these cancers are associated with human herpesvirus 8 (HHV-8). [36] Cervical cancer occurs more frequently in those with AIDS because of its association with human papillomavirus (HPV). [36] Conjunctival cancer (of the layer that lines the inner part of eyelids and the white part of the eye) is also more common in those with HIV. [37] Additionally, people with AIDS frequently have systemic symptoms such as prolonged fevers, sweats (particularly at night), swollen lymph nodes, chills, weakness, and unintended weight loss . [38] Diarrhea is another common symptom, present in about 90% of people with AIDS. [39] They can also be affected by diverse psychiatric and neurological symptoms independent of opportunistic infections and cancers. [40] Transmission Average per act risk of getting HIV by exposure route to an infected source Exposure route Chance of infection Blood transfusion 90% [41] Childbirth (to child) 25% [42] [ clarification needed ] Needle-sharing injection drug use 0.67% [43] Percutaneous needle stick 0.30% [44] Receptive anal intercourse * 0.04–3.0% [45] Insertive anal intercourse * 0.03% [46] Receptive penile-vaginal intercourse * 0.05–0.30% [45] [47] Insertive penile-vaginal intercourse * 0.01–0.38% [45] [47] Receptive oral intercourse *§ 0–0.04% [45] Insertive oral intercourse *§ 0–0.005% [48] * assuming no condom use § source refers to oral intercourse performed on a man HIV is spread by three main routes: sexual contact , significant exposure to infected body fluids or tissues, and from mother to child during pregnancy, delivery, or breastfeeding (known as vertical transmission ). [13] There is no risk of acquiring HIV if exposed to feces , nasal secretions, saliva, sputum , sweat, tears, urine, or vomit unless these are contaminated with blood. [49] It is also possible to be co-infected by more than one strain of HIV—a condition known as HIV superinfection . [50] Sexual The most frequent mode of transmission of HIV is through sexual contact with an infected person. [13] However, an HIV-positive person who has an undetectable viral load as a result of long-term treatment has effectively no risk of transmitting HIV sexually. [51] [52] The existence of functionally noncontagious HIV-positive people on antiretroviral therapy was controversially publicized in the 2008 Swiss Statement , and has since become accepted as medically sound. [53] Globally, the most common mode of HIV transmission is via sexual contacts between people of the opposite sex ; [13] however, the pattern of transmission varies among countries. ... CD4 + T Lymphocyte count (cells/mm³) HIV RNA copies per mL of plasma Days after exposure needed for the test to be accurate [108] Blood test Days Antibody test (rapid test, ELISA 3rd gen) 23–90 Antibody and p24 antigen test (ELISA 4th gen) 18–45 PCR 10–33 HIV/AIDS is diagnosed via laboratory testing and then staged based on the presence of certain signs or symptoms . [25] HIV screening is recommended by the United States Preventive Services Task Force for all people 15 years to 65 years of age, including all pregnant women. [109] Additionally, testing is recommended for those at high risk, which includes anyone diagnosed with a sexually transmitted illness. [28] [109] In many areas of the world, a third of HIV carriers only discover they are infected at an advanced stage of the disease when AIDS or severe immunodeficiency has become apparent. [28] HIV testing HIV Rapid Test being administered Oraquick Most people infected with HIV develop specific antibodies (i.e. seroconvert ) within three to twelve weeks after the initial infection. [27] Diagnosis of primary HIV before seroconversion is done by measuring HIV- RNA or p24 antigen . [27] Positive results obtained by antibody or PCR testing are confirmed either by a different antibody or by PCR. [25] Antibody tests in children younger than 18 months are typically inaccurate, due to the continued presence of maternal antibodies . [110] Thus HIV infection can only be diagnosed by PCR testing for HIV RNA or DNA, or via testing for the p24 antigen. [25] Much of the world lacks access to reliable PCR testing, and people in many places simply wait until either symptoms develop or the child is old enough for accurate antibody testing. [110] In sub-Saharan Africa between 2007 and 2009, between 30% and 70% of the population were aware of their HIV status. [111] In 2009, between 3.6% and 42% of men and women in sub-Saharan countries were tested; [111] this represented a significant increase compared to previous years. [111] Classifications Two main clinical staging systems are used to classify HIV and HIV-related disease for surveillance purposes: the WHO disease staging system for HIV infection and disease , [25] and the CDC classification system for HIV infection . [112] The CDC's classification system is more frequently adopted in developed countries. ... As of March 2020 [update] , two persons have been successfully cleared of HIV. [156] Rapid initiation of anti-retroviral therapy within one week of diagnosis appear to improve treatment outcomes in low and medium-income settings. [157] Antiviral therapy Stribild – a common once-daily ART regime consisting of elvitegravir , emtricitabine , tenofovir and the booster cobicistat Current HAART options are combinations (or "cocktails") consisting of at least three medications belonging to at least two types, or "classes", of antiretroviral agents. [158] Initially, treatment is typically a non-nucleoside reverse transcriptase inhibitor (NNRTI) plus two nucleoside analog reverse transcriptase inhibitors (NRTIs). [159] Typical NRTIs include: zidovudine (AZT) or tenofovir (TDF) and lamivudine (3TC) or emtricitabine (FTC). [159] As of 2019, dolutegravir/lamivudine/tenofovir is listed by the World Health Organization as the first-line treatment for adults, with tenofovir/lamivudine/efavirenz as an alternative. [160] Combinations of agents that include protease inhibitors (PI) are used if the above regimen loses effectiveness. [158] The World Health Organization and the United States recommend antiretrovirals in people of all ages (including pregnant women) as soon as the diagnosis is made, regardless of CD4 count. [15] [126] [161] Once treatment is begun, it is recommended that it is continued without breaks or "holidays". [28] Many people are diagnosed only after treatment ideally should have begun. [28] The desired outcome of treatment is a long-term plasma HIV-RNA count below 50 copies/mL. [28] Levels to determine if treatment is effective are initially recommended after four weeks and once levels fall below 50 copies/mL checks every three to six months are typically adequate. [28] Inadequate control is deemed to be greater than 400 copies/mL. [28] Based on these criteria treatment is effective in more than 95% of people during the first year. [28] Benefits of treatment include a decreased risk of progression to AIDS and a decreased risk of death. [162] In the developing world, treatment also improves physical and mental health. [163] With treatment, there is a 70% reduced risk of acquiring tuberculosis. [158] Additional benefits include a decreased risk of transmission of the disease to sexual partners and a decrease in mother-to-child transmission. [158] [164] The effectiveness of treatment depends to a large part on compliance. [28] Reasons for non-adherence to treatment include poor access to medical care, [165] inadequate social supports, mental illness and drug abuse . [166] The complexity of treatment regimens (due to pill numbers and dosing frequency) and adverse effects may reduce adherence. [167] Even though cost is an important issue with some medications, [168] 47% of those who needed them were taking them in low- and middle-income countries as of 2010 [update] , [155] and the rate of adherence is similar in low-income and high-income countries. [169] Specific adverse events are related to the antiretroviral agent taken. [170] Some relatively common adverse events include: lipodystrophy syndrome , dyslipidemia , and diabetes mellitus , especially with protease inhibitors. [24] Other common symptoms include diarrhea, [170] [171] and an increased risk of cardiovascular disease . [172] Newer recommended treatments are associated with fewer adverse effects. [28] Certain medications may be associated with birth defects and therefore may be unsuitable for women hoping to have children. [28] Treatment recommendations for children are somewhat different from those for adults. ... Dietary intake of micronutrients at RDA levels by HIV-infected adults is recommended by the WHO; higher intake of vitamin A , zinc , and iron can produce adverse effects in HIV-positive adults, and is not recommended unless there is documented deficiency. [184] [185] [186] [187] Dietary supplementation for people who are infected with HIV and who have inadequate nutrition or dietary deficiencies may strengthen their immune systems or help them recover from infections; however, evidence indicating an overall benefit in morbidity or reduction in mortality is not consistent. [188] Evidence for supplementation with selenium is mixed with some tentative evidence of benefit. [189] For pregnant and lactating women with HIV, multivitamin supplement improves outcomes for both mothers and children. [190] If the pregnant or lactating mother has been advised to take anti-retroviral medication to prevent mother-to-child HIV transmission, multivitamin supplements should not replace these treatments. [190] There is some evidence that vitamin A supplementation in children with an HIV infection reduces mortality and improves growth. [191] Alternative medicine In the US, approximately 60% of people with HIV use various forms of complementary or alternative medicine , [192] whose effectiveness has not been established. [193] There is not enough evidence to support the use of herbal medicines . [194] There is insufficient evidence to recommend or support the use of medical cannabis to try to increase appetite or weight gain. [195] Prognosis Deaths due to HIV/AIDS per million persons in 2012 0 1–4 5–12 13–34 35–61 62–134 135–215 216–458 459–1,402 1,403–5,828 HIV/AIDS has become a chronic rather than an acutely fatal disease in many areas of the world. [196] Prognosis varies between people, and both the CD4 count and viral load are useful for predicted outcomes. [27] Without treatment, average survival time after infection with HIV is estimated to be 9 to 11 years, depending on the HIV subtype. [7] After the diagnosis of AIDS, if treatment is not available, survival ranges between 6 and 19 months. [197] [198] HAART and appropriate prevention of opportunistic infections reduces the death rate by 80%, and raises the life expectancy for a newly diagnosed young adult to 20–50 years. [196] [199] [200] This is between two thirds [199] and nearly that of the general population. [28] [201] If treatment is started late in the infection, prognosis is not as good: [28] for example, if treatment is begun following the diagnosis of AIDS, life expectancy is ~10–40 years. [28] [196] Half of infants born with HIV die before two years of age without treatment. [178] Disability-adjusted life year for HIV and AIDS per 100,000 inhabitants as of 2004. no data ≤ 10 10–25 25–50 50–100 100–500 500–1000 1,000–2,500 2,500–5,000 5,000–7500 7,500–10,000 10,000–50,000 ≥ 50,000 The primary causes of death from HIV/AIDS are opportunistic infections and cancer , both of which are frequently the result of the progressive failure of the immune system. [181] [202] Risk of cancer appears to increase once the CD4 count is below 500/μL. [28] The rate of clinical disease progression varies widely between individuals and has been shown to be affected by a number of factors such as a person's susceptibility and immune function; [203] their access to health care, the presence of co-infections; [197] [204] and the particular strain (or strains) of the virus involved. [205] [206] Tuberculosis co-infection is one of the leading causes of sickness and death in those with HIV/AIDS being present in a third of all HIV-infected people and causing 25% of HIV-related deaths. [207] HIV is also one of the most important risk factors for tuberculosis. [208] Hepatitis C is another very common co-infection where each disease increases the progression of the other. [209] The two most common cancers associated with HIV/AIDS are Kaposi's sarcoma and AIDS-related non-Hodgkin's lymphoma . [202] Other cancers that are more frequent include anal cancer , Burkitt's lymphoma , primary central nervous system lymphoma , and cervical cancer . [28] [210] Even with anti-retroviral treatment, over the long term HIV-infected people may experience neurocognitive disorders , [211] osteoporosis , [212] neuropathy , [213] cancers, [214] [215] nephropathy , [216] and cardiovascular disease . [171] Some conditions, such as lipodystrophy , may be caused both by HIV and its treatment. [171] Epidemiology Main article: Epidemiology of HIV/AIDS See or edit source data .IL2, IFNG, IFNA1, TNF, HLA-B, HCG18, HCG17, SNHG32, CCR5, ZNRD1, ITIH4, CCR2, ERVW-1, OR12D3, PSORS1C1, DDR1, GABBR1, ERVK-20, ERVK-18, OR5V1, TNXB, ERVK-32, TP53, CXCL12, RNF39, LINC02571, PARD3B, DGKI, HCP5, CXCR4, IL10, TAT, ERVK-6, NRSN1, S100B, IL6, CHP1, TPPP, CD9, TMED2, H3P19, HLA-A, CCL5, PDLIM7, CCL2, MYC, IL1B, CD4, BCL6, MBL2, IL4, CXCL10, IL7, ADA, BCL2, CCL3L1, IL1A, B2M, ABCB1, CXCR6, IL15, APOBEC3G, DHFR, TRBV20OR9-2, FAS, F3, TLR4, GPAT3, ARC, FCGR3A, GC, APOE, ABCB6, ENTPD4, SLK, MRPL28, ACTR2, SUB1, ERVK-9, AHSA1, GRAP2, ERVK-21, JAM3, ERVK-25, VDR, TIA1, TIMP1, H3P9, LOC107987479, UNG, ERVK-19, VEGFA, SPAG9, ERVK-24, AIMP2, MICA, SOCS1, TNFSF10, ARHGEF7, ERVK-10, RNF19A, ZHX2, AICDA, PGPEP1, TGM2, CASC1, CLEC9A, USE1, NCR3, ACSS2, INTS2, DNAJB12, IL21, TBATA, GORASP1, WNK1, CARD14, NAF1, ACCS, C6orf120, MIR150, ANGPTL2, CD24, CA14, PLA2G15, LAS1L, POLDIP2, LAMP3, IGHV3-75, NXT1, ERVK-8, TLR9, MIR146B, CD209, MIR375, ASCC1, TLR7, ERVK-7, RTEL1, THBS1, NAT2, PRDX2, MSTN, DHPS, DUSP5, EPO, F9, FCGR3B, FGF1, FGF2, FGF3, FGF5, FUT1, GFAP, CYP2D6, GPI, NR3C1, HIF1A, HLA-C, HLA-DRB1, HLA-G, HSP90AA1, HSPD1, ICAM1, IFNB1, CYP27B1, CX3CR1, TRG, C4BPA, APP, FASLG, AR, ATM, ATP6V1E1, BAX, BCHE, BMP1, BST2, C3, CD14, MAPK14, TNFRSF8, CD34, CD38, ENTPD1, CD40, CDKN2B, CCR8, CR2, CRK, CRP, IGF1, IL1RN, IL5, RELA, PLK1, PML, PRCP, MAPK1, PRNP, PSMD8, PTEN, PTN, RAF1, RBL2, CCL3, IL7R, CCL4, CCL18, CXCL11, SFTPD, SOD1, SP1, STAT3, SYT1, TAC1, TAP2, PLAUR, PIN1, PAK2, OSM, CXCL8, IL12B, IL16, IL17A, IL18, INSRR, LDLR, LGALS1, LRP1, LSAMP, CYP4F3, SMAD3, MBP, MMP2, MMP9, MST1R, CYTB, MYD88, NFKB1, YBX1, OPRM1, H3P40
-
Leishmaniasis
Wikipedia
It affects as many as 12 million people worldwide, with 1.5–2.0 million new cases each year. [24] The visceral form of leishmaniasis has an estimated incidence of 500,000 new cases. [25] In 2014, more than 90% of new cases reported to WHO occurred in six countries: Brazil, Ethiopia, India, Somalia, South Sudan and Sudan. [26] As of 2010, it caused about 52,000 deaths, down from 87,000 in 1990. [10] Different types of the disease occur in different regions of the world. [2] Cutaneous disease is most common in Afghanistan, Algeria, Brazil, Colombia, and Iran, while mucocutaneous disease is most common in Bolivia, Brazil, and Peru, and visceral disease is most common in Bangladesh, Brazil, Ethiopia, India, and Sudan. [2] Leishmaniasis is found through much of the Americas from northern Argentina to South Texas , though not in Uruguay or Chile , and has recently been shown to be spreading to North Texas and Oklahoma, [27] [28] and further expansion to the north may be facilitated by climate change as more habitat becomes suitable for vector and reservoir species for leishmaniasis. [29] Leishmaniasis is also known as papalomoyo , papa lo moyo, úlcera de los chicleros , and chiclera in Latin America. [30] During 2004, an estimated 3,400 troops from the Colombian army, operating in the jungles near the south of the country (in particular around the Meta and Guaviare departments), were infected with leishmaniasis. ... Archived from the original on 4 December 2014 . Retrieved 28 November 2014 . ^ James WD, Berger TG, Elston DM (2006). ... Caister Academic Press. ISBN 978-1-904455-28-8 . Archived from the original on 23 April 2008. [ page needed ] ^ Dacie JV, Bain BJ, Bates I (2006). ... Retrieved 8 December 2015 . ^ Birsel R (28 June 2002). "Disfiguring epidemic hits 270,000 Afghans" . e-Ariana .TNF, IFNG, IL10, IL6, ARG1, IL18, CRP, TNFRSF18, MCL1, HSPA4, IL1B, SLC11A1, CXCL10, NLRP3, IL17A, TLR2, CCR5, TLR4, IL32, PRDX2, LEP, TGFB1, CD274, FCN2, CD163, MTOR, HM13, IL4, BCL2, BAX, LMLN, IGF1, HIF1A, ANXA1, VDR, UNG, TAM, NR0B2, EZR, ADA, TLR3, STAT1, MAPK3, MAPK4, EIF2AK2, PSG5, PSMD7, PTHLH, PTPN1, PTPN2, PTPN6, RPA1, RPS6, CCL2, CCL8, CXCL11, SLC1A5, SLC1A7, SNAP25, SOAT1, SPP1, TP63, EIF2S2, CDK5R1, GOPC, FOXP3, HSPA14, CD244, TOLLIP, FBLIM1, MSTO1, FBXW7, ACSS2, PDXP, SLC52A2, ALDH1A2, TMPRSS13, DCLK3, IL33, CDCA5, PWAR1, ARMH1, HNP1, CCR2, UPK3B, DLL1, SGSM3, NOX1, PABPC1, NR1I2, SPHK1, EIF2B4, EIF2B2, PRKAB1, HSPB3, SLC7A6, ARHGEF2, AIM2, H6PD, RABEPK, LANCL1, TNFSF13B, EBNA1BP2, CD160, GABARAPL2, GABARAPL1, PRDX5, POLR1A, MAPK1, NOS2, PRKAA2, PRKAA1, CST3, CTLA4, CTSB, CTSL, CYP51A1, DDT, DHFR, DPAGT1, DPP4, DSPP, DUSP4, EEF1B2, EEF2, EGFR, EIF2B1, F2R, FCGR2A, FECH, FLI1, CPB1, CCR7, LRBA, ATR, AKT1, ALDH1A1, APEX1, APRT, AQP1, ATM, ATP2A3, ATP2B4, PRDM1, CD69, BRCA1, CAPN1, CD1A, CD28, CD86, CD40, CD40LG, CD44, FPR2, G6PD, GAPDH, CYTB, MNAT1, CD200, MPG, MPL, MPST, MRC1, MSMB, MST1, AHR, MFAP1, PAEP, PHB, PIK3CA, PIK3CB, PIK3CD, PIK3CG, PLP1, PNOC, MAP3K10, MBL2, GCHFR, IFNB1, GCK, GTF3C1, HLA-C, HMOX1, HSPD1, IFN1@, IFNA1, IFNA13, IL1A, LTA, IL9, IL12A, IL12RB1, IL13, ITGA4, ITGAL, JAK2, RPSA, H3P28
-
Thalassemia
Wikipedia
The severity of the α-thalassemias is correlated with the number of affected α-globin; alleles: the greater, the more severe will be the manifestations of the disease. [28] Alpha-thalassemias result in decreased alpha-globin production; therefore, fewer alpha-globin chains are produced, resulting in an excess of β chains in adults and excess γ chains in newborns. ... Alpha thalassemias often are found in people from Southeast Asia, the Middle East, China, and in those of African descent. [29] # of missing alleles Types of alpha thalassemia [28] Symptoms 1 Silent carrier No symptoms 2 Alpha thalassemia trait Minor anemia 3 Hemoglobin H disease Mild to moderate anemia may lead normal life 4 Hydrops fetalis Fetal death usually occurs at birth Beta-thalassemia [ edit ] Main article: Beta-thalassemia Beta thalassemias are due to mutations in the HBB gene on chromosome 11, [30] also inherited in an autosomal, recessive fashion. ... – NHLBI, NIH" . www.nhlbi.nih.gov . Archived from the original on 28 July 2017 . Retrieved 6 September 2017 . ^ https://play.google.com/store/apps/details? ... ISBN 978-0-07-164114-2 . ^ Ngim, CF; Lai, NM; Hong, JY; Tan, SL; Ramadas, A; Muthukumarasamy, P; Thong, MK (28 May 2020). "Growth hormone therapy for people with thalassaemia" .PPP1R15A, HBA2, HBG2, HBA1, HBB, HBD, HBG1, HAMP, HBFQTL2, AHSP, PMCH, SEA, HFE, G6PD, GDF15, EPO, VDR, KLF1, HBZ, BRD4, LNPEP, SERPINB6, SORBS1, GH1, CAP1, HACD1, RN7SL263P, TMPRSS6, CTAA1, IL6, HBS1L, UGT1A1, HP, CSF3, IFNL3, TFRC, TNFRSF11B, SLC4A1, BCL11A, SERPINA1, GATA1, ITGB1, FXN, SCT, FAS, LINC01193, NPRL3, LILRA5, SLC40A1, YY1, VCAM1, TRV-AAC1-4, SOD1, MIR144, HBD, RAB4B-EGLN2, RHCE, TNF, PROCR, NOG, UGT1A7, DLL1, HPGDS, KRT20, NAAA, CHMP2B, UGT1A10, CADM1, UGT1A8, RAD21, PRG4, UGT1A6, UGT1A4, CD177, KIDINS220, SEPTIN9, EGLN2, EGLN3, ZFPM1, UPF1, ABO, PTH, CD34, F2, PHC1, DNTT, DMRT1, DLX4, CYP3A4, CYP2E1, CTLA4, CST3, CRP, CPB2, TNFRSF8, GABPA, CD28, MS4A1, CD1C, CD1B, RUNX1, B2M, ATRX, SERPINC1, APOE, APEX1, AFP, FN1, GCG, PSMB6, ITGA2B, PROS1, PGD, PDR, PC, SLC11A2, ACVR2B, MYH9, MYB, CD46, EPCAM, JAK2, IL3, GPT, IGHG3, IGF1, IFNG, IFNA2, HPX, HPFH2, HMGB1, HLA-DRB1, HLA-B, HLA-A, GSR, NFE2L2
-
Xeroderma Pigmentosum
Wikipedia
Symptoms can be avoided or controlled by completely avoiding exposure to sunlight, either by staying indoors or wearing protective clothing and using sunscreen when outdoors. [24] Keratosis can also be treated by using cryotherapy or fluorouracil . [4] In more severe cases of XP, even minuscule amounts of UV light, for example, from covered windows or fluorescent bulbs, can be very dangerous and trigger symptoms. [25] On September 10, 2020, Clinuvel Pharmaceuticals announced that it was investigating the use of its FDA-approved flagship drug Scenesse as a potential treatment to increase pain-free light exposure for patients with xeroderma pigmentosum. [26] [27] [28] Prognosis [ edit ] The average life expectancy of an individual with any type of XP and no neurological symptoms is approximately 37 years, and 29 years if neurological symptoms are present. [3] In the United States , the probability for individuals with the disorder to survive until 40 years of age may be as high as 70% if they have never been exposed to sunlight in their life. [29] In India , many patients with XP die at an early age from skin cancers . ... Library of Medicine. 26 June 2018 . Retrieved 28 June 2018 . ^ a b "Xeroderma pigmentosum" . dermnetnz.org . ... NORD (National Organization for Rare Disorders) . 2017 . Retrieved 28 June 2018 . ^ a b c d e f g h "Xeroderma pigmentosum" . ... Department of Health and Human Services. 2018 . Retrieved 28 June 2018 . ^ a b Ahmad S, Hanaoka F (2008).XPA, XPC, POLH, ERCC5, ERCC2, ERCC1, DDB2, ERCC4, ERCC3, TERF2, GTF2H1, TP53, NR1H2, BIVM-ERCC5, GTF2H2, GTF2H3, GTF2H5, GTF2H4, POLQ, CAT, XRCC1, CSH2, XRCC6P5, HPRT1, LIG4, ERCC6, CSH1, HRAS, OGG1, HPGDS, PCNA, PTEN, XRCC3, ENDOV, CDKN2A, GSTM1, SIRT1, MC1R, LCE2B, HSPA9, RAD23A, NRAS, FUS, WDR76, ATR, BRIP1, CHEK1, DDB1, BCL2, DECR1, ERCC8, CCNH, ATM, TYMS, BTN2A2, PTF1A, IRF9, EXO1, HERC2, RAD54L, H3P38, PDIK1L, HFM1, UBE3B, USP7, IFI44, XRCC2, CATSPER1, TDG, SLX4, XYLT2, VPS11, RTEL1, CRLF3, DEFB103A, DEFB103B, MEPE, WDR77, LRRC59, RNU1-1, VEPH1, PRDX5, SMUG1, AAGAB, KAT7, ZC3H12D, NAT1, TALDO1, CGA, FEN1, EGFR, NQO1, TIMM8A, DDX11, GADD45A, CYP1B1, CSNK2A1, CRYZ, COMT, CETN2, SYCP1, CDK7, CDK4, DDR1, BRAF, BRCA1, BAX, ATF3, ASIP, FAS, APEX1, GOT1, GSTM2, GSTT1, HGF, SULT1A1, STAT3, ST13, SMO, RNU2-1, RNU1-4, RECQL, RAD23B, PTCH1, PTAFR, MAPK8, PRKDC, POMC, AKT1, ODC1, NPM1, NCAM1, MYC, MPO, LBR, KIT, H3P33
-
Angelman Syndrome
Wikipedia
However, there are difficulties in ascertaining the levels and types of anticonvulsant medications needed to establish control, because people with AS often have multiple types of seizures. [28] Many families use melatonin to promote sleep in a condition which often affects sleep patterns. ... Archived from the original on 27 August 2016 . Retrieved 28 April 2017 . ^ a b c d e f g h i j k "Angelman Syndrome – NORD (National Organization for Rare Disorders)" . ... Archived from the original on 13 November 2016 . Retrieved 28 April 2017 . ^ a b "Common Misdiagnoses | FAST" . ... "Is Angelman syndrome an alternate result of del(15)(q11q13)?". Am J Med Genet . 28 (4): 829–38. doi : 10.1002/ajmg.1320280407 .UBE3A, CDKL5, MECP2, GABRB3, SNRPN, SNHG14, SYNGAP1, SLC6A1, PRKN, MUL1, ASXL3, CBLL2, KCNQ3, UBE2K, SNURF, OCA2, MKRN3, SLC9A6, PRNP, GABRG3, TCF4, HERC2, SNORD116@, HDAC1, RNF2, PVALB, ATP10A, UROD, STOML3, GABRA5, DYRK1A, MC1R, NIPA1, HTC2, BDNF, CYFIP1, H3P12, COPS2, ATP8A1, ZNF197, HDAC9, EEF1E1, MIR708, LMLN, NPAP1, DDI1, ATRAID, DYM, EPHA6, LAMTOR1, CYP26B1, SLC5A7, HAP1, DERL1, ASPM, NIPA2, TPPP2, TMPRSS13, TUBGCP5, NPAS3, ACTB, HERC1, MEF2C, CAMK2A, CDKN2C, CFL1, CREBBP, CYP11A1, DBI, DNAH8, EP300, ERBB4, ESR1, FOXG1, FMR1, HDAC2, HTR1A, MSMB, CASK, MST1, MTHFR, NDN, NNAT, NR4A2, PAFAH1B1, PSMD4, SCG5, SLC6A3, APP, TOP1, TP53, UBE2I, MAFK, TJP1